Translate this page into:
Acute generalized exanthematous pustulosis in a child probably induced by terbinafine
2 Department of Pathology, Celal Bayar University, Faculty of Medicine, Manisa, Turkey
Correspondence Address:
Aylin T�rel Ermertcan
Celal Bayar University, Faculty of Medicine, Department of Dermatology, 45010, Manisa
Turkey
| How to cite this article: Bayata S, Ermertcan AT, Ates M, Temiz P. Acute generalized exanthematous pustulosis in a child probably induced by terbinafine. Indian J Dermatol Venereol Leprol 2015;81:95 |
Sir,
Acute generalized exanthematous pustulosis (AGEP) is a cutaneous adverse drug reaction, frequently caused by antimicrobials. Aminopenicillins and macrolides are the leading causes of this reaction. [1]
A 14-year-old boy was referred to us from the pediatric outpatient clinic, with complaints of reddened skin, itchy eruptions and fever. Cutaneous examination showed a generalized eruption of confluent, tiny, millimeter-sized pustules on an erythematous base, most pronounced over the lower extremities [[Figure - 1], [Figure - 2], [Figure - 3]]. Systemic examination was within normal limits. History revealed that he had recently been prescribed oral terbinafine 250 mg per day for tinea cruris, and the rash had appeared on the third day of treatment. He was not using any other systemic or topical medications. The clinical possibilities considered included pustular psoriasis and acute generalized exanthematous pustulosis.
 |
| Figure 1: Millimeter-sized pustules coalescing on a generalized erythematous base over the back |
 |
| Figure 2: Millimeter-sized pustules localized on the lower extremities |
 |
| Figure 3: Close up view of the pustules |
Routine blood tests showed leukocytosis (18600 cells/mm 3 ), neutrophilia (80.3%), eosinophilia (2.9%) and an increased erythrocyte sedimentation rate (43 mm/hr). A skin biopsy showed a normal granular layer, subcorneal pustules, dermal edema and a perivascular mixed inflammatory infiltrate with eosinophils [Figure - 4]. Based on the clinical and histopathological findings, the patient was diagnosed to have acute generalized exanthematous pustulosis.
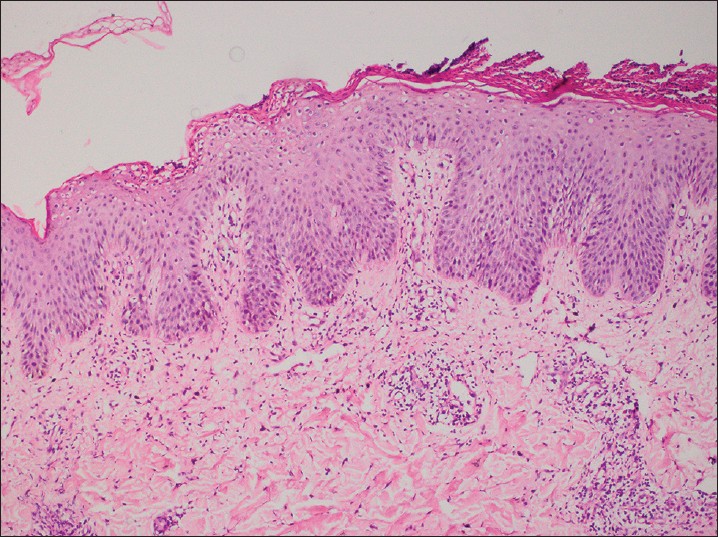 |
| Figure 4: Normal granular layer, subcorneal pustules, dermal edema and perivascular mixed inflammatory infiltrate with eosinophils (HE, ×40) |
Terbinafine was suspected to be the causative drug and was discontinued. Symptomatic treatment was given with antipyretics, mid-potent topical steroids, emollients and wet dressings. The lesions disappeared within 2 weeks, followed by desquamation.
The allylamine antifungal terbinafine is reported to cause adverse reactions in more than 7% of cases, 2% of which affect the skin, including severe reactions like Stevens-Johnson syndrome [1] . Terbinafine has also been associated with acute generalized exanthematous pustulosis and pustular psoriasis. [2]
In children, acute generalized exanthematous pustulosis is mainly attributed to antibiotics, antipyretic analgesics and vaccines. [3] The eruption is clinically difficult to distinguish from other pustular dermatoses such as pustular psoriasis, and histopathological findings are also not easily differentiated. [1],[2] Generalized pustular psoriasis has been triggered as well as exacerbated by the use of terbinafine. The difference between drug-induced acute generalized exanthematous pustulosis and pustular psoriasis becomes more evident as the disease progresses, because the former usually resolves spontaneously in 10-15 days. [2]
As the treatment options differ greatly, skin biopsy should be undertaken to differentiate acute generalized exanthematous pustulosis from other pustular dermatoses such as pustular psoriasis. The typical changes of psoriasis such as acanthosis and papillomatosis are usually absent in acute generalized exanthematous pustulosis. [4] The presence of eosinophils, necrotic keratinocytes and a mixed neutrophil-rich interstitial and mid-dermal infiltrate, and the absence of tortuous, dilated blood vessels, are features suggestive of acute generalized exanthematous pustulosis rather than pustular psoriasis. [5]
This case report highlights the fact that although high fever accompanied by a pustular eruption may prompt us to suspect an infectious disease or pustular psoriasis, drug reactions must also be considered in the differential diagnosis.
| 1. |
Beltraminelli HS, Lerch M, Arnold A, Bircher AJ, Haeusermann P. Acute generalized exanthematous pustulosis induced by the antifungal terbinafine: Case report and review of the literature. Br J Dermatol 2005;152:780-3.
[Google Scholar]
|
| 2. |
Duckworth L, Maheshwari MB, Thomson MA. A diagnostic challenge: Acute generalized exanthematous pustulosis or pustular psoriasis due to terbinafine. Clin Exp Dermatol 2012;37:24-7.
[Google Scholar]
|
| 3. |
Zhang JL, Chen X, Li J, Xie HF. Clinical analysis of childhood acute generalized exanthematous pustulosis. Zhongguo Dang Dai Er Ke Za Zhi 2008;10:497-9.
[Google Scholar]
|
| 4. |
Fernando SL. Acute generalized exanthematous pustulosis. Australas J Dermatol 2012;53:87-92.
[Google Scholar]
|
| 5. |
Kardaun SH, Kuiper H, Fidler V, Jonkman MF. The histopathological spectrum of acute generalized exanthematous pustulosis (AGEP) and its differentiation from generalized pustular psoriasis. J Cutan Pathol 2010;37:1220-9.
[Google Scholar]
|
Fulltext Views
5,403
PDF downloads
3,106





