Acute graft rejection following bilateral cadaveric hand transplant
Corresponding author: Dr. Laxmisha Chandrashekar, Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India. laxmishac@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramar SY, Logamoorthy R, Srinivas BH, Chandrashekar L. Acute graft rejection following bilateral cadaveric hand transplant. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_71_2025
Dear Editor,
A 31-year-old man presented with diffuse raised scaly lesions and oedema on the transplanted limbs for a month, five years after a bilateral cadaveric hand transplant. His post-transplant immunosuppressive regimen, consisting of oral prednisolone, tacrolimus, and mycophenolate mofetil (MMF), was compromised by multiple lapses in adherence over several months and irregular follow-up. Cutaneous examination revealed multiple violaceous papules and plaques with diffuse scaling, along with well-to-ill-defined keratotic plaques on bilateral palms [Figure 1a]. All fingernails were dystrophic with haemorrhagic crusting over the fingertips. Dermoscopy of skin lesions revealed Wickham’s striae with intervening areas of normal skin [Figure 1b]. A forearm biopsy revealed hyperkeratosis, acanthosis, apoptotic keratinocytes, lymphocyte exocytosis, and basal vacuolar degeneration. In addition, there was a band-like lichenoid infiltrate of lymphocytes and eosinophils at the dermo-epidermal junction [Figures 2a and 2b] and perivascular and peri-adnexal regions, as well as squamous metaplasia of eccrine ducts. Immunohistochemistry was strongly positive for CD3+ [Figure 2c] and CD8+ in the inflammatory infiltrate, weakly positive for CD4+, negative for CD20+ [Figure 2d], and non-contributory for C4d+. The severity of allograft rejection was classified as Grade 3 based on histological findings. The findings indicated acute graft rejection due to immunosuppression noncompliance, which resolved with pulse intravenous methylprednisolone (500 mg) twice daily for three days, after which he was maintained on tacrolimus, 1 mg in the morning and 0.5 mg at night, along with MMF 1 g twice daily [Figure 3].

- Diffuse scaly violaceous papules and plaques over the transplanted area involving the bilateral forearm and palms.
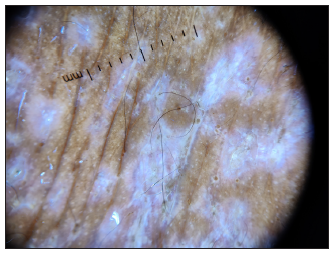
- Dermoscopy (DL4, 10× magnification, polarised mode) of violaceous papules on the forearm revealed Wickham’s striae characterised by fine, whitish reticular lines.
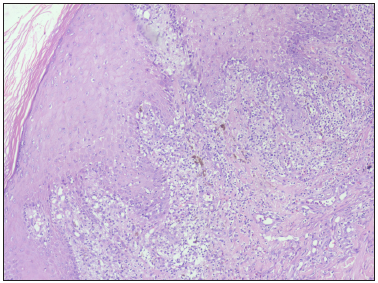
- Section shows hyperkeratosis of the epidermis with interface dermatitis at the dermo-epidermal junction (Haematoxylin & eosin, 100x).
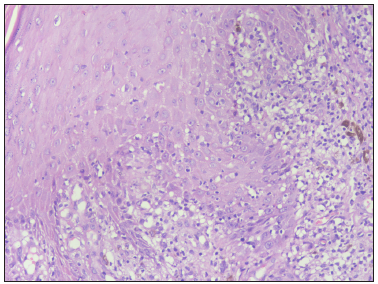
- Basal cell vacuolation and lymphocytic infiltrate at the dermo-epidermal junction (Haematoxylin and eosin, 400x).
- Positive immunohistochemical staining for CD3, highlighting the dermal infiltrate of T-lymphocytes (40x).
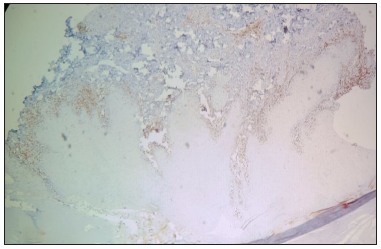
- Negative immunohistochemical staining for CD20, indicating the absence of B-lymphocytes within the infiltrate (40x).

- Resolution of the skin lesions following treatment with post inflammatory pigmentation.
Hand transplantation, especially using cadaveric donors, has emerged as a viable option for patients with upper limb loss. However, acute graft rejection poses a substantial risk, potentially compromising graft survival and function. Acute graft rejection involves immune-mediated damage to the transplanted tissue. The skin is particularly vulnerable due to its immunogenic properties, which makes detecting and managing rejection crucial. It typically occurs within weeks to months post-transplantation and is characterised by T-cell and antibody-mediated responses against donor antigens.1 Outcomes from hand transplants performed worldwide showed that acute skin rejection typically affects the dorsal and volar areas of the forearm and wrist. This involvement can be either patchy and localised or diffuse and uniform. The contributing groups have collectively observed a total of 34 rejection episodes in patients transplanted at their respective centers.2-5 The skin’s high immunogenicity, due to potent antigen-presenting cells like Langerhans cells and keratinocytes, contributes to this high incidence. The visible nature of hand transplants facilitates early detection and frequent biopsies, leading to a higher reported incidence of acute rejection compared to other organ transplants. In addition to classical rejection, some patients experienced an atypical form of rejection characterised by a desquamative palmar rash and nail dystrophy. This novel rejection pattern was associated with mechanical stress to the palms, potentially triggering and sustaining an immune response.6,7 In conclusion, acute graft rejection remains a formidable challenge in hand transplantation, necessitating vigilant monitoring and proactive management strategies. Our case underscores the consequences of non-compliance with immunosuppressive therapy and emphasises the need for comprehensive patient care to ensure long-term graft survival and functional outcomes. Further research into the mechanisms underlying atypical rejection patterns and tailored therapeutic approaches is essential for improving patient outcomes in hand transplantation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Face, upper extremity, and concomitant transplantation: Evolution of a discipline. Transplantation. 2012;93:105-11.
- [Google Scholar]
- The international registry on hand and composite tissue transplantation. Transplantation. 2005;79:1210-4.
- [CrossRef] [PubMed] [Google Scholar]
- Successful hand transplantation—one-year follow-up. N Engl J Med. 2000;343:468-73.
- [CrossRef] [PubMed] [Google Scholar]
- Status 5 years after bilateral hand transplantation. Am J Transplant. 2006;6:834-41.
- [CrossRef] [PubMed] [Google Scholar]
- First forearm transplantation: Outcome at 3 years. Am J Transplant. 2007;7:1753-62.
- [CrossRef] [PubMed] [Google Scholar]
- Two decades of hand transplantation: A systematic review of outcomes. Ann Plast Surg. 2022;88:335-44.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical acute rejection after hand transplantation. Am J Transplant. 2008;8:688-96.
- [CrossRef] [PubMed] [Google Scholar]





