Translate this page into:
Acute skin failure: Concept, causes, consequences and care
Correspondence Address:
Arun C Inamadar
Department of Dermatology, BLDEA's SBMP Medical College, Hospital and Research Centre, Bijapur- 586103, Karnataka
India
| How to cite this article: Inamadar AC, Palit A. Acute skin failure: Concept, causes, consequences and care. Indian J Dermatol Venereol Leprol 2005;71:379-385 |
Abstract
Acute skin failure is a state of total dysfunction of the skin resulting from different dermatological conditions. It constitutes a dermatological emergency and requires a multi-disciplinary, intensive care approach. Its effective management is possible only when the underlying pathomechanism of each event is clear to the treating clinician. The concept of skin failure is new to non-dermatologist clinicians and sketchy among many dermatologists. Here the pathomechanism of skin failure has been analyzed and a guideline for monitoring has been provided. There is a need for intensive care units for patients with acute skin failure.

 |
 |
Skin failure
Skin failure has been defined as loss of normal temperature control with inability to maintain the core body temperature, and failure to prevent percutaneous loss of fluid, electrolytes and protein, with resulting imbalance, and failure of the mechanical barrier to prevent penetration of foreign materials.[1]
The concept of skin failure is not well known and the need for intensive care in dermatology is overlooked. However, acute skin failure is no less serious than visceral dysfunctions like cardiac, pulmonary, renal or hepatic failure. Though Ryan had included a wide range of conditions reflecting physical and psychological disabilities in dermatology under skin failure, here the discussion has been restricted to conditions that give rise to extensive structural disruption and total functional impairment of the skin.[2]
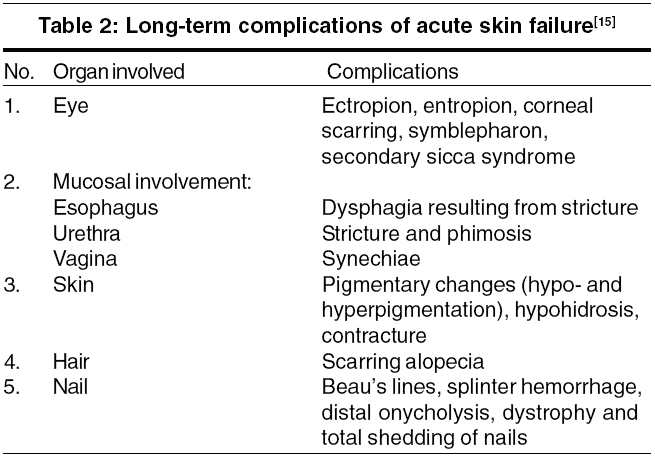
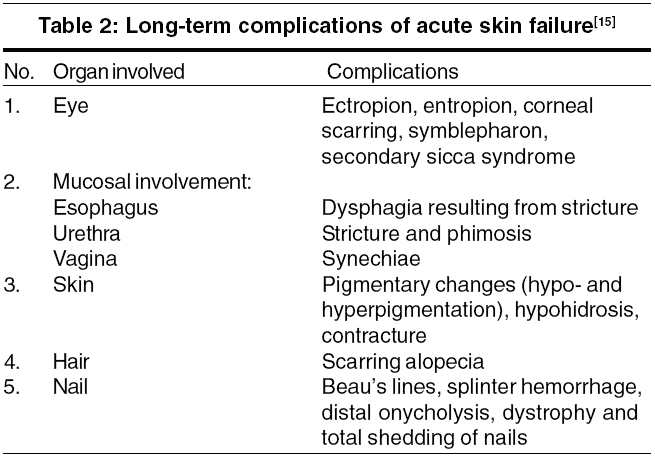
Causes of acute skin failure Acute skin failure is a consequence of various primary dermatological disorders. As with other organ failures, patients with acute skin failure deserve special attention and management protocol. The causes of acute skin failure have been summarized in [Table - 1].
Consequences of acute skin failure Acute skin failure is associated with hemodynamic changes, impaired thermoregulatory control and metabolic complications. In addition, fluid and electrolyte imbalance and loss of essential nutrients affect patient survival. The major consequences of acute skin failure have been discussed below.
Altered hemodynamics: Persistent inflammation of the skin leads to marked peripheral vasodilatation and increased cutaneous blood flow, clinically evident as widespread scarlet erythema and edema. This is especially evident in cases of chronic long-standing erythroderma. In addition, there is increased blood volume and cardiac output, which may jeopardize an already compromised cardiovascular system (hypertensive, ischemic or valvular heart disease) resulting in high-output cardiac failure.
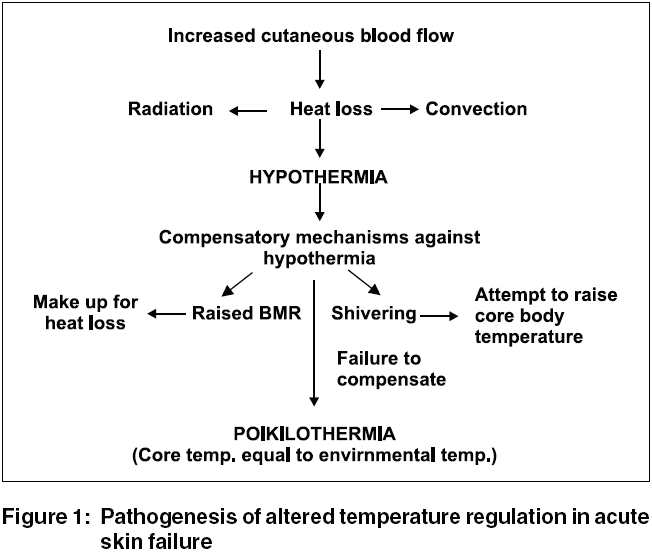
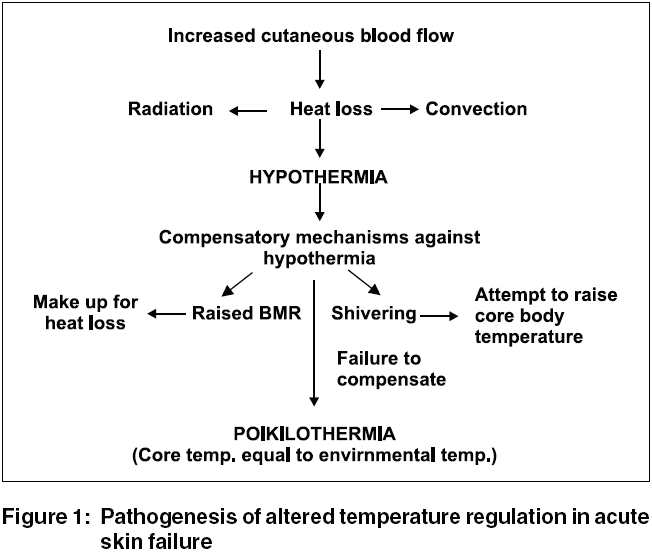
Altered thermoregulation: Hypothermia is a very common occurrence in these patients. A schematic representation of the major alteration in temperature regulation mechanism has been given in [Figure - 1].[3],[4] However, in the majority of patients with extensive skin lesions; there may be fever even in the absence of infection. This is mediated by interleukin-1, produced by damaged keratinocytes.[5] With underlying conditions like psoriasis, the skin is already hypohidrotic or anhidrotic due to intraepidermal occlusion of the sweat ducts, and hyperthermia may be seen.[3] Sudden onset hypothermia in a relatively stabilized patient, rather than fever, may be a premonitory sign of septic shock.[6]
Metabolic abnormalities: As a compensatory mechanism for total heat loss, there is a rise of the basal metabolic rate (BMR). A hyperglycemic state and glycosuria are common in these patients (50%)[6] and result from associated pancreatitis and decreased insulin secretion, relative insulin resistance, stress, and infection. Altered glucose metabolism enhances caloric loss by depleting tissue protein as an energy source. Shivering (high grade muscular activity), as a compensatory mechanism for hypothermia, is also highly energy consuming.
Fluid and electrolyte imbalance: The usual total water loss through the skin is 400 ml/day6 (600-1000 ml/day in temperate climates).[7] In patients with acute skin failure, the daily percutaneous water loss far exceeds this. This is due to impaired barrier function of the skin resulting in increased transepidermal water loss (TEWL), and enhanced percutaneous fluid loss by transpiration (proportionate to the raised BMR).
TEWL is highest at the peak of loss of skin through scaling. The average daily fluid loss in adult TEN patients with approximately 50% body surface area (BSA) involvement is 3-4 liters.[8] If fluid replacement is not adequate, there is reduction in the intravascular volume and formation of hyperosmolar urine. The manifestations are dehydration and decreased urinary output. This is associated with electrolyte imbalance (low Na+ and high K+), and raised serum levels of urea and creatinine (prerenal uremia). Patients with toxic epidermal necrolysis and autoimmune bullous disorders have, in addition, extra loss of Na+, K+ and Cl- in the blister fluid.[6] Hypophosphatemia is a common complication in these patients, aggravating insulin resistance, and altering the neurological status and diaphragmatic function. Patients with acute generalized pustular psoriasis may develop acute hypocalcemia secondary to severe hypoalbuminemia.
Loss of nutrients: The principal nutrients lost in acute skin failure are protein and iron. The main causes of hypoproteinemia are continuous loss through shed scales, increased BMR, decreased hepatic synthesis, dermatogenic enteropathy leading to protein loss (seen in fulminant psoriasis and other cases of chronic erythroderma), and dilution due to hypervolemia (which is not of much significance).
The normal material exfoliated from the skin amounts to 500-1000 mg/day.[4] It is increased several folds (9 g/m2 body surface area/day)[3] in different disease states precipitating acute skin failure. Diffuse scaling leads to protein loss of approximately 20-30 g/m2 BSA/day.[4] This amount varies with the underlying diseases, the maximum being in psoriasis followed by drug reactions and eczema.[4] In presence of exudative skin lesions, the combined protein loss through oozing from the skin surface and urine (urinary nitrogen derived from hypercatabolism) may amount to 150-200 g/day.[6]
The rise in BMR seen among patients with acute skin failure occurs at the cost of catabolism of tissue protein. Alteration in glucose metabolism enhances further depletion of tissue protein. The cumulative effect of these factors is a negative nitrogen balance, increased urinary nitrogen and hypoalbuminemia. In cases with preexisting, long-standing erythroderma, protein deficiency is evident as prominent muscle wasting.
In addition to the loss through the shed skin, there is impaired absorption and utilization of iron and vitamin B12. An increased cellular turnover rate gives rise to relative folate deficiency. All these factors contribute to anemia.
Peripheral edema: Peripheral edema is common in long-standing cases. Its probable causes are:
1. Increased capillary leakage and consequent shift of fluid to extravascular spaces[3] Significantly increased levels of circulating vascular permeability factor (VPF)/ vascular endothelial growth factor (VEGF) are found in psoriasis, eczema and other causes of erythroderma[9]
2. Hypoalbuminemia
3. Associated cardiac failure
4. Inflammation resulting from the primary skin disease
VPF and VEGF are multifunctional cytokines liberated by lesional keratinocytes which induce dermal capillary proliferation and enhance microvascular permeability.[9]
Pulmonary complications: Aspiration pneumonitis is common in severely ill patients. Pulmonary involvement may be a systemic manifestation and a dreaded complication of TEN. Severe pulmonary edema (secondary to capillary leak syndrome) and adult respiratory distress syndrome (ARDS) are complications of erythroderma.[9],[10] Overzealous correction of hypovolemia frequently gives rise to overt pulmonary edema (30%).[6]
Altered immune function: lymphopenia (90%), neutropenia (30%) and thrombocytopenia (15%) are well-known complications of TEN.[6] Impaired chemotaxis and phagocytosis of granulocytes and low serum gamma globulin levels are common.[3] CD4+ T lymphocytopenia may be associated even in the absence of HIV infection.[3]
Infection: Damaged barrier function of the skin facilitates colonization and systemic entry of commensal, exogenous and endogenous (gut flora) microorganisms. The incidence of septic complications is increased in the presence of altered body defence mechanisms.
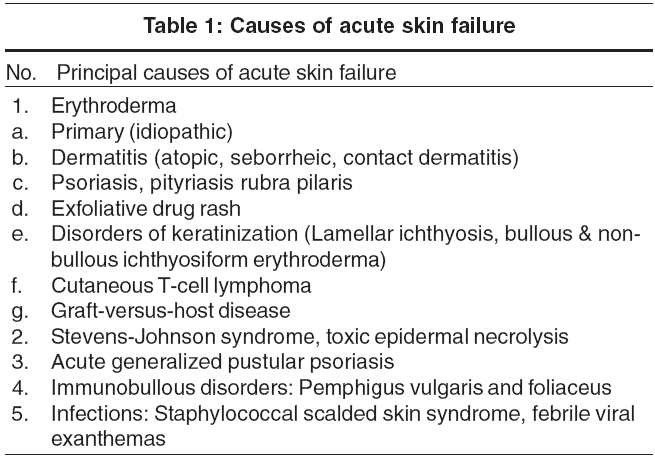
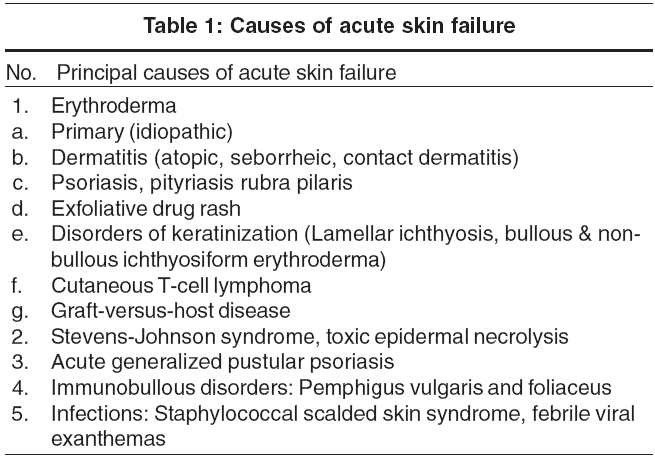
Additionally, patients may develop deep vein thrombosis resulting from prolonged immobilization. Chronic illness, and associated anxiety and sleeplessness may give rise to stress ulcers. In the healing phase, some sequelae may involve the eyes, mucous membranes, skin, hair and nail. These long-term complications [Table - 2] can cause great morbidity.
Care of patients with acute skin failure Establishment of an intensive care unit for patients with acute skin failure was first conceptualized by Professor Renι Touraine in 1976.[6] The necessity of establishing such a unit in every dermatological tertiary care center has since been well recognized.
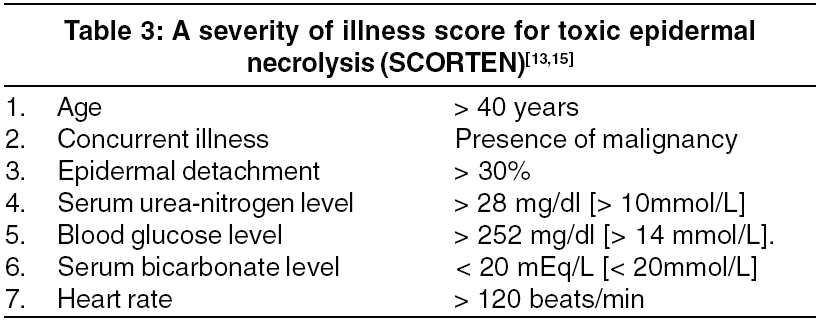
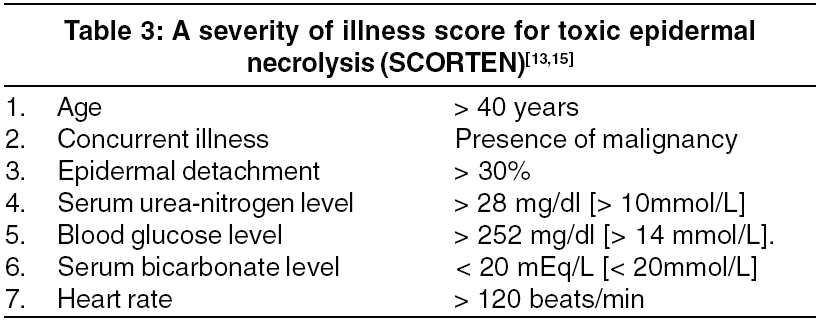
Assessment of the severity of the disease helps in planning the management. An approximate idea of body surface area involvement can be obtained by application of the ′rule of nines.′[11] Disease specific scoring systems like PASI (Psoriasis Area Severity Index) and EASI (Eczema Area Severity Index) determine the extent of skin involvement but are not helpful to assess systemic parameters. SAPS (Simplified Acute Physiological Score) is a useful guide to the clinical and biological parameters to be monitored as well as prognostic factors.[12] SCORTEN, a TEN-specific severity scale, is an accurate predictor of mortality.[13] It is based on seven independent risk factors [Table - 3] that are evaluated within the first 24 hours of admission. The mortality rate assessed by SCORTEN is proportional to the number of risk factors present in an individual patient, as compared to SAPS, which indicated a poor agreement between expected and actual mortality.[13],[14] Trent et al observed that the expected mortality rates with 0 -1 risk factors and 5 or more risk factors were 3.2% and 90% respectively with SCORTEN.[14]
The management of patients with acute skin failure requires well-synchronized teamwork. In addition to experienced dermatologists, internists and well-trained, devoted nursing staff are needed for continuous monitoring of patients. The pillars in the management of such patients are nursing care; monitoring hemodynamic changes; fluid, electrolyte balance and nutrition; prevention of complication (e.g. sepsis); prompt identification of risk factors; and topical therapy.
Nursing care and general measures Most institutions in India do not have intensive care units for patients with acute skin failure. Hence, patients can be managed in burn units or in a specialized ward. The environmental temperature should be maintained at 30°-32°C;[6] alternatively, an infrared lamp can be used to reduce shivering and the associated energy loss. Use of air-fluidized beds and a burn-cage ensures patient comfort and easy handling. However, air-fluidized beds may increase the evaporative fluid loss from the body surface, and are better avoided till major fluid and electrolyte imbalance is corrected.[6]
Regular cleaning and removal of crusts from the oral and nasal cavities, and care of the eyes, genitalia and perianal region has to be ensured. In female patients with TEN, periodic examination of the vagina for erosions is mandatory, as timely use of dressings reduces the chances of vaginal synechiae formation.[15] Once or twice daily bathing in lukewarm water (35°-38°C) is recommended.[6] Introduction of an intravenous line and urinary catheter or condom drainage are mandatory. A nasogastric tube should be considered in the presence of severe mucosal involvement restricting oral intake or in severely ill patients. In addition to feeding, it helps in assessing gastric emptying. An hourly record of the pulse, respiratory rate, blood pressure, and urine volume and osmolality is essential. The body temperature and gastric emptying (measuring volume of gastric aspiration) should be recorded every 3 to 4 hours. An accurate daily intake-output chart should be maintained.
Monitoring hemodynamic changes Since there is continuous loss of water through the body surface, patients with acute skin failure are under a continuous threat of developing hypovolemia. The important indicators of hemodynamic status in such patients are pulse rate, urine output and urine osmolality. Arterial blood pressure is not much helpful in this regard as the body tends to maintain a normal level through release of catecholamines, as in other conditions with stress.[6] A urine output of 50-100 ml/hour and an osmolality lower than 1020 are indicative of adequate tissue perfusion.[6] However, while assessing the adequacy of urine output in these patients, hyperglycemia has to be ruled out as it is commonly associated. A reduction in urine volume may be an early indicator of hypovolemia or septicemia. A pulse rate of 120 or more/minute, even in the presence of precipitating factors like septicemia and fever, indicates a negative fluid balance.[6]
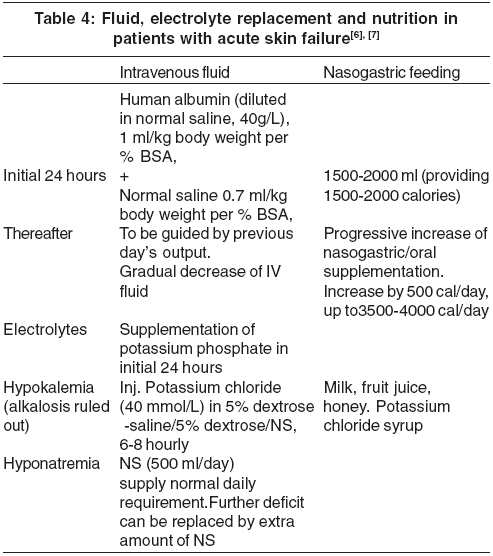
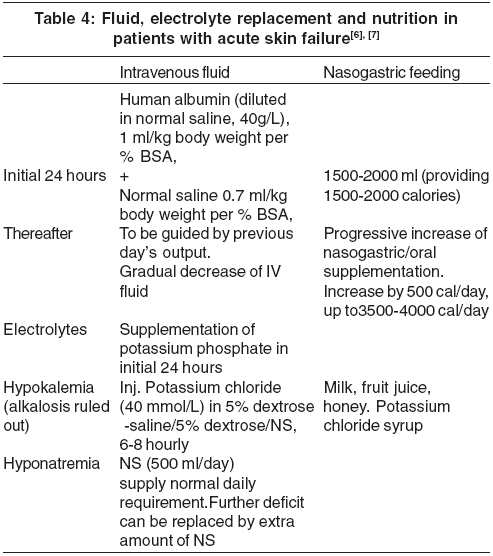
Fluid, electrolyte and nutrition Like other states of shock, intravascular fluid loss must be replaced quickly. Thereafter, the total body water and electrolytes can be restored gradually. The initial fluids of choice are colloids (human albumin or fresh frozen plasma) and normal saline (NS). Human albumin is a better choice than plasma, because there is no risk of infections. The daily fluid requirement in a patient with acute skin failure has to be calculated depending on the previous day′s output. A combination of intravenous and enteral supplementation has to be given. A schedule for fluid and nutritional supplementation has been presented in [Table - 4].[6]
Though toxic epidermal necrolysis is often compared with burn injury, the fluid requirement is 2/3rd to 3/4th of that of patients with burns covering the same area.[6] This is because the depth of tissue destruction and underlying vascular injury is less in case of TEN and subcutaneous edema is milder.
Prolonged infusion with NS may precipitate gradual hypokalemia and the chance of this increase if feeding is withheld for more than 96 hours.[7] Occasionally, hypokalemia may be present in spite of a normal serum value. [7]
The patient′s diet should be high in protein, 2-3 g/kg body weight per day in adults and 3-4 g/ kg body weight per day in children.[6] In acutely ill patients, gastric emptying may be delayed, resulting in regurgitation and inhalation during repeated nasogastric feeding. If the residual gastric aspirate is more than 50 ml, periodic feeding should be withheld.[6]
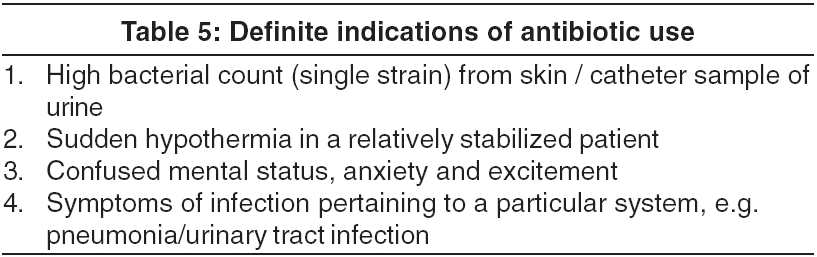
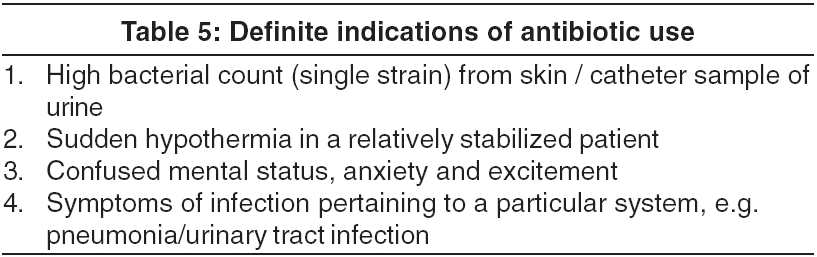
Prevention of sepsis Hand washing and aseptic handling of the patient has the greatest impact in reducing the chances of infection. Barrier nursing should be practiced stringently. Introduction of a central venous catheter through contaminated skin carries an inevitable risk of precipitating septicemia and is better avoided in certain circumstances.[6] Bacteriology of the skin lesions (culture sensitivity test of discharge or pus) should be performed initially and on alternate days, so that sepsis can be identified at the earliest or antibiotics can be changed promptly. An altered sensorium, in the form of anxiety or confusion, may be the first sign of sepsis.[6] An increased respiratory rate may be the first sign of hypoxia resulting from pneumonia.[6] The prophylactic use of antibiotics in the absence of evident infection is not agreeable to many authors. The indications of antibiotic use are given in [Table - 5].
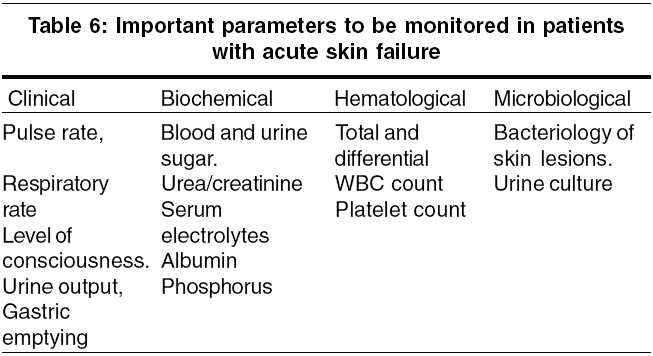
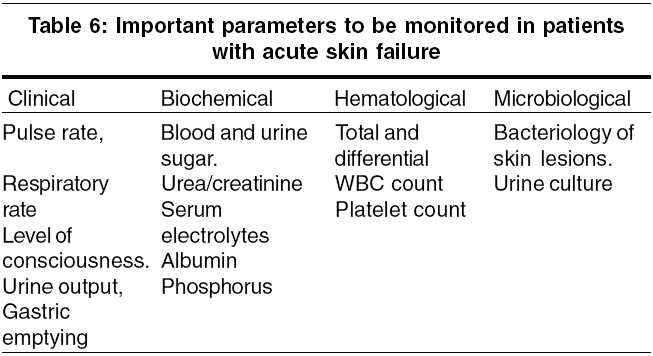
The poor prognostic factors in acute skin failure are older age, larger body surface area involvement, presence of severe neutropenia, early thrombocytopenia, high blood urea nitrogen level and a causative drug with long half life in drug-induced cases.[15] [Table - 6] provides a list of important parameters to be monitored in these patients. In spite of stringent management, acute skin failure is associated with a high mortality, resulting from various systemic causes [Table - 7].[10],[15]
Topical management An oozy, denuded skin should be managed conservatively. In patients with TEN, the detachable epidermis is preferably left in place. Topical agents (0.5% silver nitrate) can be used as paints or dressings.[6] Non-physiologic lipids (petrolatum jelly, lanolin) in vapor-permeable dressings (gauze) can be used as barrier repair agents. Use of physiologic lipids (component mixture of cholesterol, ceramide and free fatty acids in an optimized ratio of 3:1:1), accelerates the barrier repair.[16] Moreover, use of these emollients prevents the skin surface from sticking to the bed or the apparel. Traditionally banana leaves have been used as non-sticky dressings at various centers in India. Other biological dressings like amnion and collagen-based skin substitutes can be used when available.[6] Newer modalities available for covering areas with epidermal detachment in patients with TEN are cadaveric allografts, cultured human allogeneic or autologous epidermal sheets, and human newborn fibroblasts cultured on a nylon mesh of Biobrane.[17]
Other measures Individual cases should be considered for anticoagulant therapy, sedatives like diazepam or morphine to reduce anxiety and apprehension, and H2-blockers to prevent stress ulcers. In the presence of significant hyperglycemia, insulin should be added as per medical advice. Ophthalmic care should be provided in the form of protective ocular pads, periodic instillation of normal saline or artificial tears, and preventive measures for synechiae formation. Use of gas-permeable scleral contact lenses improves the visual acuity, reduces photophobia and discomfort, and prevents further sequelae by facilitating healing of corneal epithelial defects.[17] An amniotic membrane has been successfully used for dressing eye lesions in patients with TEN.[18]
Identification of the underlying disorder that has resulted in acute skin failure is of immense importance. In cases with adverse cutaneous drug reactions, the causative drug has to be stopped immediately and chemically related drugs avoided. This measure is especially helpful in controlling the condition if the causative drug has a short half life. Specific therapies like intravenous immunoglobulin, methotrexate and systemic steroid are to be administered in cases like TEN, psoriatic erythroderma and drug hypersensitivity syndrome respectively.
Care of patients with acute skin failure does not end with clinical improvement of the condition. The discharge sheet should bear clear instructions regarding avoidance of specific and chemically related drugs in cases of severe adverse cutaneous drug reactions. Patients with ophthalmic sequelae should be followed up to prevent visual handicap. Photoprotection should be advised for few months to prevent chances of cutaneous pigmentary changes.
KEY Points
1.Patients with extensive skin lesions may be febrile even in absence of infection.
2.Sudden onset hypothermia in a relatively stabilized patient may be a premonitory sign of septic shock.
3.A pulse rate of 120 or more / minute, even in presence of precipitating factors like septicemia and fever indicates a negative fluid balance. A normal blood pressure may be misleading in such a case.
4.Increased respiratory rate may be the first sign of hypoxia resulting from pneumonia/ pulmonary edema.
5.A reduction in urine volume may be an early indicator of hypovolemia or septicemia.
6.An altered sensorium, in the form of anxiety or confusion may be the first sign of sepsis.
7.If residual gastric aspirate volume is more than 50 ml, periodic feeding is to be withheld.
8.Overzealous fluid correction may precipitate high output heart failure in patients with compromised cardiovascular system, or may give rise to pulmonary edema.
9.Though serum concentration represents a normal value, occult hypokalemia may exist.
Conclusion
Acute skin failure constitutes a dermatological emergency that requires a multi-disciplinary, intensive care approach. Adequate knowledge about monitoring these patients and hospitalization in specialized units can reduce the high morbidity and mortality associated with this condition. Though many Indian institutes have facilities for advanced dermatological care like laser therapy, phototherapy and dermatosurgery, few have an intensive care unit for patients with acute skin failure.
| 1. |
Irvine C. "Skin failure"- a real entity: discussion paper. J R Soc Med 1991;84:412-3.
[Google Scholar]
|
| 2. |
Ryan TJ. Disability in dermatology. Br J Hosp Med 1991;46:33-6.
[Google Scholar]
|
| 3. |
Holden CA, Berth-Jones J. Eczema, lichenification, prurigo and erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of dermatology. 7th ed. Oxford: Blackwell-Science; 2004. p. 17.1-17.55.
[Google Scholar]
|
| 4. |
Kimgai-Asadi A, Freedberg IM. Exfoliative dermatitis. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's Dermatology in general medicine. 6th ed. New York: McGraw-Hill; 2003. p. 436-41.
[Google Scholar]
|
| 5. |
Luger TA, Stadler BM, Katz SI, Oppenheim JJ. Epidermal cell (keratinocyte) derived thymocyte activating factor (ETAF). J Immunol 1981;127:1493-8.
[Google Scholar]
|
| 6. |
Roujeau JC, Revuz J. Intensive care in dermatology. In: Champion RH, Pye RJ, editors. Recent advances in dermatology. Edinburgh: Churchill-Livingstone; 1990. p. 85-99.
[Google Scholar]
|
| 7. |
Langford RM, Mythen MC. Critical care; fluid, electrolyte and acid-base balance; blood transfusion. In: Russel RCG, Williams NS, Bulstrode CJK, editors. Bailey and Love's Short practice of surgery. 23rd ed. London: Arnold; 2000. p. 40-63.
[Google Scholar]
|
| 8. |
Revuz J, Roujeau JC, Guillaume JC, Penso D, Touraine R. Treatment of toxic epidermal necrolysis, Crιteil's experience. Arch Dermatol 1987;123:1156-58.
[Google Scholar]
|
| 9. |
Creamer D, Allen MH, Groves RW, Barker JN. Circulating vascular permeability factor/vascular endothelial growth factor in erythroderma. Lancet 1996;348:1101.
[Google Scholar]
|
| 10. |
Rothe MJ, Bialy TL, Grant-Kels JM. Erythroderma. Dermatol Clin 2000;18:405-15.
[Google Scholar]
|
| 11. |
Coleman DJ. Burns. In: Russel RCG, Williams NS, Bulstrode CJK, editors. Bailey and Love's Short practice of surgery. 23rd ed. London: Arnold; 2000. p.189-99.
[Google Scholar]
|
| 12. |
LeGall JR, Loirat P, Alperovitch A. A simplified acute physiologic score for intensive care unit patients. Crit Care Med 1984;12:975-77.
[Google Scholar]
|
| 13. |
Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol 2000;115:149-53.
[Google Scholar]
|
| 14. |
Trent JT, Kirsner RS, Romanelli P, Kerdel FA. Analysis of intravenous immunoglobulin for the treatment of toxic epidermal necrolysis using SCORTEN: The University of Miami experience. Arch Dermatol 2003;139:39-43.
[Google Scholar]
|
| 15. |
Breathnach SM. Erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of dermatology. 7th ed. Oxford: Blackwell-Science; 2004. p. 74.1-74.20.
[Google Scholar]
|
| 16. |
Elias PM, Feingold KR. Does the tail wag the dog? Role of the barrier in the pathogenesis of inflammatory dermatoses and therapeutic implications. Arch Dermatol 2001;137:1079-81.
[Google Scholar]
|
| 17. |
Ghislain PD, Roujeau JC. Treatment of severe drug reactions: Stevens-Johnson syndrome, toxic epidermal necrolysis and hypersensitivity syndrome. Dermatol Online J 2002;8:5.
[Google Scholar]
|
| 18. |
John T, Foulks GN, John ME, Cheng K, Hu D. Amniotic membrane in the surgical management of acute toxic epidermal necrolysis. Ophthalmology 2002;109:351-60.
[Google Scholar]
|
Fulltext Views
41,444
PDF downloads
9,758





