Translate this page into:
Acute syndrome of apoptotic panepidermolysis: Series of three cases
Corresponding Author: Dr. Sonal Jain, 15, Ashok colony, Malviya Nagar, Jaipur, Rajasthan, India. sonalreachesout@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohapatra L, Jain S, Mohanty P, Mohanty J, Mohanty M. Acute syndrome of apoptotic panepidermolysis: Series of three cases. Indian J Dermatol Venereol Leprol 2022;88:873.
Sir,
Toxic epidermal necrolysis-like presentation of acute cutaneous lupus can be clinically indistinguishable from drug-induced toxic epidermal necrolysis. Only less than 50 cases have been reported worldwide.1 We describe three such cases with a brief review of literature.
A 35-year-old woman presented with a 12-week history of progressive development of painful haemorrhagic blisters with sheet-like desquamation on bilateral upper arms, legs, chest, face and back, involving about 60% of the body surface area [Figures 1 and 2]. She also had erythema over the malar area & painful targetoid lesions over the palms and soles. There were erosions on the hard palate and lips. Eye and genital mucosae examination were unremarkable. There was no history of any drug intake prior to the appearance of lesions. Haematological parameters revealed microcytic anaemia (haemoglobin- 7 gm%) and leucopoenia (total leucocyte count- 3,400/cu.mm, normal- 4000–11000 per mm3). Anti-nuclear antibodies, anti-SSA/Ro and anti-Smith antibodies were positive. There was hypoalbuminaemia and proteinuria. Skin biopsy revealed a detached epidermis with full-thickness necrosis and dyskeratotic cells, with lymphocytic infiltrate in the upper dermis [Figure 3]. A direct immunofluorescence study showed positive immunoglobulin IgG and IgA deposition along the basement membrane zone in a granular pattern [Figure 4]. Based on clinical, histological and laboratory findings, a diagnosis of systemic lupus erythematosus with toxic epidermal necrolysis-like presentation was made. The patient responded to intravenous corticosteroids, with re-epithelialization occurring in the next 10 days, and was discharged on prednisolone (40 mg/day) and hydroxychloroquine (400 mg/day).

- Haemorrhagic crusting with peeling of skin over back in case 1

- Malar rash with typical sparing of nasolabial fold over the face in case 1
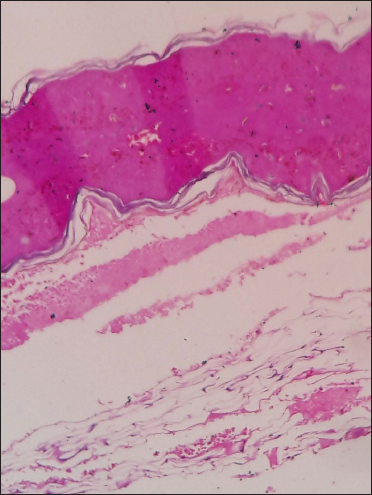
- (H&E ×40)–Detached epidermis with full-thickness necrosis and dyskeratotic cells
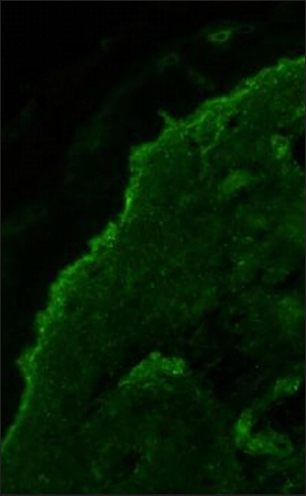
- Direct immunofluorescence showing granular deposits of IgG and IgA along the dermo-epidermal junction
A 25-year-old woman presented with an erythematous rash over the entire body with multiple haemorrhagic bullae and vesicles over the chest, neck, back and face since 1 week. Nasal mucosa showed haemorrhagic crusting. Eye and genital mucosal examinations were unremarkable. Palatal erosions were present. There was no history of antecedent drug intake. Laboratory investigations revealed Hb% -8gm/dl and TLC- 3900 per mm3. Full-thickness epidermal necrosis with sub-epidermal cleft and upper dermal lymphocytic infiltrate was seen in histopathology. Antinuclear antibody (ANA) titre & anti-Ribonucleoprotein/Smith were positive. She had hypoalbuminaemia and proteinuria. She was admitted and showed improvement with injection dexamethasone 12 mg/day with oral hydroxychloroquine (400 mg/day) and general care of the wounds. The patient recovered within a week and was discharged on prednisolone (20 mg/day) and hydroxychloroquine (400 mg/day).
The third case was a 19-year-old female presenting with a 10-week history of painful haemorrhagic bullae, with sheet-like peeling of skin starting from photo-exposed areas to involve 40% of BSA. Erosions with curdy white deposits were present in the oral cavity. Other mucosae were spared. There was no history of drug intake prior to the appearance of lesions. Laboratory investigations showed microcytic anaemia. ANA and anti-Smith antibodies were positive. Urinalysis showed proteinuria and red blood cells. Lesions healed with depigmentation over two weeks. The patient was treated with prednisolone (40 mg/day).
Ting et al.2 proposed the term ‘acute syndrome of apoptotic pan-epidermolysis’ to designate clinical entities characterized by acute and massive cleavage of the epidermis, resulting from hyperacute epidermal basal cell apoptotic injury. It is most commonly seen in drug-induced toxic epidermal necrolysis but rarely may be seen in lupus erythematosus, pseudoporphyria and graft vs host disease. Acute cutaneous lupus erythematosus can present as toxic epidermal necrolysis, thus adding to the diagnostic dilemma of the physician. Differentiating toxic epidermal necrolysis-like acute cutaneous lupus erythematosus and drug-induced toxic epidermal necrolysis can be difficult as both share clinical and histological findings such as diffuse desquamation, mucosal erosions and keratinocyte necrosis [Table 1].2 Insidious onset, lack of drug causality, absence of genital/ocular mucosal erosions, positive ANA and other autoimmune profiles, an initial photodistribution and a prolonged disease course characterise toxic epidermal necrolysis-like acute cutaneous lupus erythematosus, while an identifiable trigger and more acute onset (less than 9 days) favour toxic epidermal necrolysis. In our three cases, the onset was insidious, with the absence of genital/ocular involvement, and the absence of drug history with positive autoimmune markers, thus favouring a diagnosis of toxic epidermal necrolysis-like presentation of acute cutaneous lupus erythematosus. This absence of drug causality was also evident in previous reports of lupus erythematosus-associated toxic epidermal necrolysis.2-4 Mandelcorn et al.5 described two cases of systemic lupus erythematosus with toxic epidermal necrolysis-like presentation with positive ANA and positive Ro/La serology. Both toxic epidermal necrolysis and systemic lupus erythematosus are inflammatory dermatoses, with keratinocyte apoptosis as a hallmark. In toxic epidermal necrolysis, the postulated mechanism is complex, involving keratinocyte apoptosis mediated by cytotoxic T cells via soluble mediators such as granulysin, granzyme and perforin and the interaction of Fas–Fas ligands.4 Similar molecular mediators have also been described in systemic lupus erythematosus. In the reported cases of toxic epidermal necrolysis-like systemic lupus erythematosus, corticosteroids, intravenous immunoglobulin and wound care are described as the cornerstones of treatment. Most of these reported patients survive and enter remission. Positive associations of anti-Sm antibodies with renal involvement like proteinuria, haematuria, urinary cellular casts, nephrotic syndrome, renal insufficiency and end-stage renal disease are well-documented and were also seen in our cases.6 The purpose of the report is to highlight this atypical presentation of the disease and hence increase awareness among treating dermatologists.
| Toxic epidermal necrolysis | TEN- like ACLE | |
|---|---|---|
| Trigger | Drug hypersensitivity | SLE predisposition, UV light |
| Distribution | Diffuse | Photodistribution |
| Mucous membrane | +++++ | ++ |
| Palms/ soles | ++++ | + |
| Multiorgan involvement | Systemic toxicity (e.g., pulmonary, liver) | Systemic toxicity and organ system pattern of SLE (e.g., lupus nephritis) |
| Hypercoagulable state | No | May be at risk |
| Laboratories | Eosinophilia | ANA, a-Ro, a-dsDNA |
| Treatment (besides burn unit placement) | IVIG, D/C inciting drug, wound care, corticosteroids | Corticosteroids,?IVIG, sun protection, wound care |
TEN: Toxic epidermal necrolysis, ACLE: Acute cutaneous lupus erythematosus, SLE: Systemic lupus erythematosus, UV: Ultraviolet, ANA: Anti-nuclear antibodies, a-dsDNA: Anti-double stranded DNA, IVIg: Intravenous immunoglobulin
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Erythema multiforme and Stevens-Johnson syndrome/toxic epidermal necrolysis associated with lupus erythematosus. J Am Acad Dermatol. 2012;67:417-21.
- [CrossRef] [PubMed] [Google Scholar]
- Toxic epidermal necrolysis–like acute cutaneous lupus erythematosus and the spectrum of the acute syndrome of apoptotic pan–epidermolysis (ASAP): A case report, concept review and proposal for new classification of lupus erythematosus vesiculobullous skin lesions. Lupus. 2004;13:941-50.
- [CrossRef] [PubMed] [Google Scholar]
- Toxic epidermal necrolysis–like rash of lupus: A dermatologist’s dilemma. Indian J Dermatol. 2014;59:401-2.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic lupus erythematosus presenting as steven–johnson syndrome and toxic epidermal necrolysis. Lupus. 2011;20:647-52.
- [CrossRef] [PubMed] [Google Scholar]
- Lupus-associated toxic epidermal necrolysis: A novel manifestation of lupus? J Am Acad Dermatol. 2003;48:525-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical associations of anti–Smith antibodies in PROFILE: A multi–ethnic lupus cohort. Clin Rheumatol. 2015;34:1217-23.
- [CrossRef] [PubMed] [Google Scholar]





