Translate this page into:
Adenocarcinoma of the gall bladder presenting with a cutaneous metastasis
2 Departments of Radiotherapy, All India Institute of Medical Sciences, New Delhi, India
3 Departments of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India
4 Departments of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
M Ramam
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi 110029
India
| How to cite this article: Kaur J, Puri T, Julka P K, Gunabushanam G, Iyer VK, Singh MK, Ramam M. Adenocarcinoma of the gall bladder presenting with a cutaneous metastasis. Indian J Dermatol Venereol Leprol 2006;72:64-66 |
 |
 |
 |
 |
Sir,
Cutaneous metastasis is a relatively uncommon manifestation of visceral malignancy. It mostly occurs late in the course of disease, but in approximately 8% patients, it may be the presenting sign of underlying malignancy.[1] The most common tumors to metastasize to the skin are breast, lung, colorectal, renal, and ovarian carcinomas.[2] Occasionally, metastases may arise from other primary tumors. We report on a patient who presented with a cutaneous metastasis that was subsequently found to have arisen from adenocarcinoma of the gall bladder.
A 42-year-old man had his attention drawn to a small nodule on the right side of the neck by his barber 40 days before reporting to us. It had progressively enlarged to form a large hard plaque. Otherwise asymptomatic, it caused restriction in the movements of the neck by its size and induration. He also complained of episodes of abdominal pain mainly in the epigastric region for the past 1 year.
The plaque, on the anterior triangle of the neck, was skin-colored, roughly triangular, 10 x 8 x 12 cm3, and was well-defined. It was hard, indurated, and nontender. The surface showed a peau d′orange appearance. It was not fixed to the underlying structures [Figure - 1], nor was there any significant lymphadenopathy. The rest of the physical examination did not reveal any abnormality in other systems. The abdomen was soft, with no organomegaly. Rectal examination was normal. The cardiovascular system and lungs were normal.
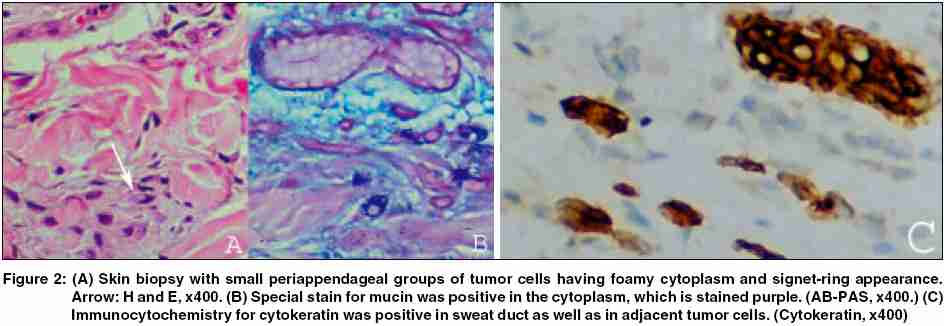
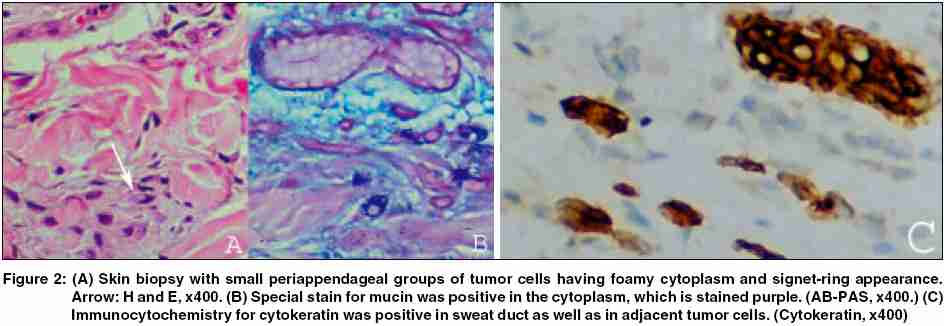
The hemogram and biochemical parameters were within normal limits, except for slightly raised serum alkaline phosphatase (315 IU; normal range, 80-240 IU). The chest radiograph was normal. Histopathologic examination of the plaque showed cells lying singly and in small groups in a periappendageal location. These cells had pleomorphic nuclei and a foamy cytoplasm. Some cells had a faintly hematoxyphilic tinge to the cytoplasm and occasionally, cells showed nuclear indentation [Figure - 2]A, arrow. There was mucin in the lower dermis which stained with Alcian blue-periodic-acid-Schiff (AB-PAS) [Figure - 2]B and mucicarmine stains. Immunohistochemistry for pan cytokeratin (DAKO Cytomation, Denmark) was positive in the atypical cells and the adjacent normal sweat duct [Figure - 2]C. These features suggested a metastatic mucin-producing adenocarcinoma with the primary tumor probably located in the gastrointestinal tract.
The patient was investigated for a primary neoplasm. Upper gastrointestinal endoscopy revealed a small superficial ulcer at one end of the stomach; a biopsy from it revealed no evidence of malignancy. Ultrasonography of the abdomen showed an echogenic sludge-filled distended gall bladder with a polypoidal growth in the fundus. Contrast-enhanced CT examination of the abdomen showed an enhancing polypoidal growth in the fundus of the gall bladder, which was extending to its anterior wall. There was no evidence of disease elsewhere within the abdomen. Ultrasonography-guided fine-needle aspiration cytology from the gall bladder mass showed predominantly necrotic cells admixed with mucin with a few viable malignant cells from an adenocarcinoma.
Based on the clinical, histopathological, cytological, and radiological features, a diagnosis of cutaneous metastasis with a primary neoplasm in the gall bladder was made. The patient was administered palliative combination chemotherapy with gemcitabine and carboplatin, with partial clinical response of the skin lesion.
Cutaneous metastases from internal carcinomas are relatively rare. An estimated 0.7-9% of these tumors metastasize to the skin. A recent meta-analysis found an overall incidence rate of approximately 5%.[2] The most frequent primary tumor to metastasize to the skin is breast carcinoma, forming 24% of all cutaneous metastases, followed by carcinoma of the lung, colorectal carcinoma, renal carcinoma, ovarian carcinoma, and bladder carcinoma, with rates of 3.4-4% each.[2] In men, carcinoma of the lung is the most common primary tumor, followed by carcinomas of the large intestine and oral cavity.[3] In women, the primary tumor is mostly carcinoma of the breast, followed by carcinomas of the large intestine and ovary.[3] The primary neoplasm is usually identified before the cutaneous metastases but in approximately 8% of cases, cutaneous metastasis is the presenting feature.[1] This occurs more commonly in men than in women.
The most common sites for metastases are the chest and abdomen, whereas other sites such as the extremities, neck, back, and scalp are involved only rarely.[2] Cutaneous metastases typically present as asymptomatic cutaneous or subcutaneous nodules.[1] Other morphologies have also been noted-an inflammatory pattern mimicking cellulitis and lesions masquerading as erythema annulare, condyloma, herpes zoster, epidermal inclusion cyst, and an ulcer.[1]
The most common histologic type of malignancy of the gall bladder is adenocarcinoma.[1] The occurrence of metastatic adenocarcinoma from the gall bladder to the skin is rare, with only nine reported cases, including four in the English language.[4],[5],[6],[7] In the latter reports, the cutaneous metastases were located on the preauricular area, upper lip, umbilicus, scalp, neck, upper arms, and back.[4],[5],[6],[7] The lesions were described as nodular, smooth, and red-brown. Only one case showed epidermal invasion with ulceration.[4] The presence of cutaneous metastases is a grave prognostic indicator, with an average survival time of 7.5 months.[1]
| 1. |
Saeed S, Keehn CA, Morgan MB. Cutaneous metastasis: a clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol 2004;31:419-30.
[Google Scholar]
|
| 2. |
Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: a meta-analysis of data. South Med J 2003;96:164-7.
[Google Scholar]
|
| 3. |
Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol 1972;105:862-8.
[Google Scholar]
|
| 4. |
Padilla RS, Jarmillo M, Dao A, Chapman W. Cutaneous metastatic adenocarcinoma of gallbladder origin. Arch Dermatol 1982;118:515-7.
[Google Scholar]
|
| 5. |
Krunic A, Martinovic N, Calonje E, Milinkovic M. Cutaneous metastatic adenocarcinoma of gallbladder origin presenting as carcinoma of unknown primary. Int J Dermatol 1995;34:360-2.
[Google Scholar]
|
| 6. |
Tongco RC. Unusual skin metastases from carcinoma of the gallbladder. Am J Surg 1961;102:90-3.
[Google Scholar]
|
| 7. |
Russell PW, Brown CH. Primary carcinoma of the gallbladder: report of 29 cases. Ann Surg 1950;132:121-8.
[Google Scholar]
|
Fulltext Views
2,810
PDF downloads
1,436





