Translate this page into:
Adult onset Langerhans cell histiocytosis: Report of two patients
2 Department of Pathology, Apollo Hospitals, Hyderabad, Andhra Pradesh, India
3 Deramatrendz, Himayat Nagar, Hyderabad, India
4 Dr. DBN Dermatology and Aesthetic Centre, Jubilee Hills, Hyderabad, India
Correspondence Address:
Indukooru Subrayalu Reddy
A-8 Anand Sheel Enclave, Nandi Nagar, Road Number 14, Banjara Hills, Hyderabad - 500 034, Andhra Pradesh
India
| How to cite this article: Reddy IS, Gowrishankar S, Somani VK, Murthy DN. Adult onset Langerhans cell histiocytosis: Report of two patients . Indian J Dermatol Venereol Leprol 2014;80:560-562 |
Sir,
Langerhans cell histiocytosis (LCH) comprises a spectrum of diseases ranging from an indolent and asymptomatic, localized form to an aggressive, systemic form involving multiple organs and producing significant symptoms. Although it can occur in individuals of any age, it is more common in children aged 1-3 years. Involvement of the skin is very common and may represent the earliest sign of the disease. Skin lesions vary from papules, vesicles, pustules and nodules to ulcers. Systemic lesions involve bones, lungs, liver, spleen and lymph nodes. We report two adult patients, one with extensive disease involving the skin and internal organs and the other with limited skin involvement.
Patient 1
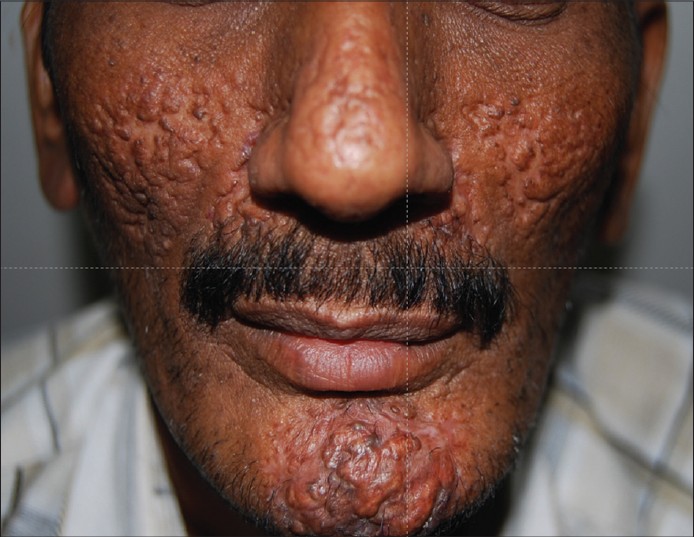
A 38-year-old male presented with well-defined, erythematous, indurated, fleshy plaques over the central face for 3 years [Figure - 1]. The vertex and occipital areas of the scalp showed crusted papules, pustules and erosions. The liver was palpable 2-3 cm below the right costal margin and non-tender. Lymph nodes in the supraclavicular area were enlarged, discrete and non-tender.
 |
| Figure 1: Erythematous, fleshy plaques over the face |
Investigations showed raised erythrocyte sedimentation rate (100 mm/hr) and elevated levels of serum bilirubin (2.5 mg/dl), aspartate amino transferase (90 IU/l), alanine amino transferase (125 IU/l) and alkaline phosphatase (1280 IU/l). Skin biopsy revealed a dense pandermal infiltrate of histiocytes with a few eosinophils [Figure - 2]. The histiocytes stained with ovoid shaped with abundant cytoplasm and a prominent indented and reniform nucleus. The histiocytes were CD1a and S100 immunohistochemical stains (left and right insets) [Figure - 2]. Correlating the history, cutaneous examination and skin biopsy, a diagnosis of LCH was made. Skeletal survey was within normal limits. Computerised tomography (CT) of the abdomen showed hepatomegaly and multiple nodular lesions in both lobes, along the portal vein and in the porta hepatis. CT scan of the chest showed multiple cystic lesions in the parenchyma of both lungs. In view of multi-system involvement, the patient was treated with vinblastine 7.8 mg intravenously, once a week along with prednisolone 60 mg daily. After the second cycle of chemotherapy, the patient had fracture neck of left femur due to an accidental fall and could not continue the treatment. Subsequent follow up at 3 months after the second cycle of chemotherapy showed complete resolution of all skin lesions with deep scars [Figure - 3].
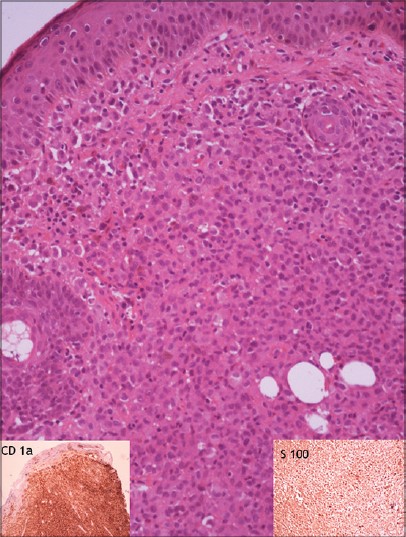 |
| Figure 2: Normal epidermis with diffuse pandermal infiltrate of histiocytes and eosinophils: First patient (H and E, ×100). The inset on the left shows CD1a positivity and on the right shows S100 positivity |
 |
| Figure 3: Complete resolution of all skin lesions after second cycle chemotherapy |
Patient 2
A 28-year-old male presented with a two- year history of pain in the perianal area and blood stained stools on and off. He also complained of excessive thirst and frequent urination and purulent discharge from both ears. Clinical examination showed erythema, edema, erosions and excoriations of the perianal area [Figure - 4]. The rest of the skin, mucous membranes and nails were normal. Hemogram, blood sugar, renal and liver function tests were within normal limits. Rectal ultrasound showed subcutaneous edema on the right side of the anal canal. Sigmoidoscopy and magnetic resonance imaging of the pelvis were within normal limits. A skin biopsy from the perianal area showed large round cells with reniform nuclei through the entire thickness of the dermis. A few eosinophils and neutrophils were present amidst the histiocytes. The large, round infiltrating cells showed CD1a and S100 confirming the diagnosis of LCH. Further work up could not be done as the patient was lost to follow up.
 |
| Figure 4: Erythema and erosions over the perianal area: Second patient |
Langerhans cell histiocytoses is a rare disease, seen among children under the age of 10 years, with an annual incidence of 1 in 200,000. [1] In adults, the condition is even rarer, with an annual incidence of 1 in 560,000. [2] The term LCH includes a spectrum of diseases that are characterized by an etiologically unknown localized or generalized proliferation of histiocytes that belong to the cells of the monocyte-macrophage lineage. [3]
Skin lesions are common and are often the presenting manifestation of LCH. [4] They involve the scalp, trunk and intertriginous areas. Morphologically, skin lesions present as subtle, translucent papules, scaly and crusted papules, vesicles and pustules mimicking seborrheic dermatitis. In the flexures, papules and vesicles coalesce to form superficial erosions and weeping lesions. Fissures are seen behind the ears, and in the axillary and inguinal folds, resembling atopic dermatitis. Oral manifestations in the form of gingival bleeding and necrotic and ulcerative lesions over the gums resulting in premature loss of teeth have been described.
The lung is the most common systemic organ involved in LCH [3] .This is seen more commonly in adult onset LCH, especially in smokers. [5] It presents as dyspnea, tachypnea, cough, cyanosis and chest pain. Chest radiographs show a typical honey-comb appearance. Involvement of liver and spleen result in hepatosplenomegaly, jaundice, ascites and cirrhosis. Skeletal involvement results in osteolytic lesions affecting skull bones, maxilla and mandible that present as localized pain, soft tissue swelling and spontaneous fractures. Diabetes insipidus is the most common endocrine manifestation.
The histopathology of LCH is characterized by clusters or sheets of large ovoid cells with abundant cytoplasm and a prominent nucleus which is indented or reniform. The histiocytes are admixed with other inflammatory cells such as eosinophils, neutrophils and lymphocytes. Langerhans cells possess characteristic organelles called Birbeck granules, which under electron microscopy appear as tennis racquet-shaped structures with a variable length and a constant width of 33 nm.
The treatment of LCH is determined by the extent of disease. [6] Isolated skin lesions may resolve spontaneously or may respond to topical steroids and nitrogen mustard. Disseminated disease may respond to various chemotherapeutic agents such as vinblastine, vincristine, methotrexate and etoposide. A combination of vinblastine and steroids is often used.
Fleshy, vegetating plaques over the central face as seen in our first patient is an uncommon feature as is the exclusive involvement of perianal skin as observed in the second patient. LCH was not among the list of clinical differential diagnoses in both. The systemic involvement in the first patient was also clinically silent. It is possible that the second patient also had systemic involvement; this, however, could not be confirmed as he was lost to follow up. It is important that the correct diagnosis be made on biopsy as appropriate chemotherapy can result in a prompt and spectacular response as seen in our first patient.
ACKNOWLEDGEMENTS
Dr. Srinivas Chakravarty, Consultant Haematologist and Medical Oncologist, Apollo Hospital, Hyderabad.
| 1. |
Alston RD, Tatevossian RG, McNally RJ, Kelsey A, Birch JM, Eden TO. Incidence and survival of childhood langerhans cell histiocytosis in Northwest England from 1954 to1998. Pediatr Blood Cancer 2007; 48:555-60.
[Google Scholar]
|
| 2. |
Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans'- cell histiocytosis in adults. Med Pediatr Oncol 1997; 28:9-14.
[Google Scholar]
|
| 3. |
Götz G, Fichter J. Langerhans'- cell histiocytosis in 58 adults. Eur J Med Res 2004; 9:510-4.
[Google Scholar]
|
| 4. |
Magaña-Garcia M. Pure cutaneous histiocytosis X. Int J Dermatol 1986; 25:106-8.
[Google Scholar]
|
| 5. |
Aricò M. Langerhans cell histiocytosis in adults: More questions than answers? Eur J Cancer 2004; 40:1467-73.
[Google Scholar]
|
| 6. |
Cambazard F, Louis Stephan J. The histiocytosis, langerhans cell and non-langerhans cell histiocytosis. In: Harper J, Orange A, Prose N, editors. Text Book of Paediatric Dermatology. 2 nd ed. Oxford: Blackwell Publishing; 2006. p. 1699-721.
[Google Scholar]
|
Fulltext Views
3,417
PDF downloads
1,908





