Translate this page into:
Adult-onset Still's disease presenting as blotchy and flagellate pigmentation
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Neetu Bhari
Department of Dermatology and Venereology, All India Institute of Medical Sciences, Room No: 4070, 4th Floor Teaching Block, New Delhi
India
| How to cite this article: Patra S, Bhari N, Mohta P, Singh S, Ramam M, Agarwal S. Adult-onset Still's disease presenting as blotchy and flagellate pigmentation. Indian J Dermatol Venereol Leprol 2019;85:626-628 |
Sir,
A 17-year-old girl presented to the dermatology department with fever, moderately itchy rash on the trunk, lower limbs and hands associated with pain and swelling of joints of upper and lower limbs for the past 3 months. She also had history of loss of weight and appetite. However, there was no photosensitivity, malar rash or muscle weakness. Her previous investigations revealed anemia [hemoglobin (Hb) 6 g%] and neutrophilic leukocytosis (30,000/cmm with 85% neutrophils). She was treated with oral antibiotics and a transfusion of 2 units of packed red blood cells. Computed tomography scan of the abdomen at that time revealed mesenteric lymphadenopathy for which she was empirically treated with antitubercular therapy for 2 weeks. Her condition did not improve with antitubercular therapy. As fever and rash continued to progress, she presented to us. On examination, she was febrile (101°F) and had pallor. She had tenderness and mild swelling of interphalangeal joints of hands, right knee and right ankle joint. There was diffuse non-cicatricial alopecia on scalp. Cutaneous examination revealed symmetrical dusky erythematous plaques with central semi-adherent scaling on trunk, lower limbs, nape of neck and dorsum of hands [Figure - 1] and [Figure - 2]. There were linear streaks extending from the plaques in a flagellate pattern [Figure - 2]. There was no organomegaly or lymphadenopathy. She was found to have anemia (Hb 9.0 g%), high total leucocyte count (22,240/cmm, neutrophilia 88%), high erythrocyte sedimentation rate (150 mm) and a very high serum ferritin (30,879 ng/mL). Her rheumatoid arthritis factor and antinuclear antibodies were negative and liver function tests were within normal limits. Histopathology from a skin biopsy specimen showed many necrotic (dyskeratotic) keratinocytes in the superficial epidermis specifically in the stratum corneum and upper spinous layer with a moderate perivascular infiltrate of neutrophils, eosinophils and lymphocytes in the superficial dermis [Figure - 3]. Alcian blue–periodic acid–Schiff stain revealed moderate increase in dermal mucin.
 |
| Figure 1: Blotchy hyperpigmentation and dusky erythematous plaques on abdomen and hands |
 |
| Figure 2: Symmetrical hyperpigmented and dusky erythematous plaques on back with linear streaks extending in a flagellate pattern |
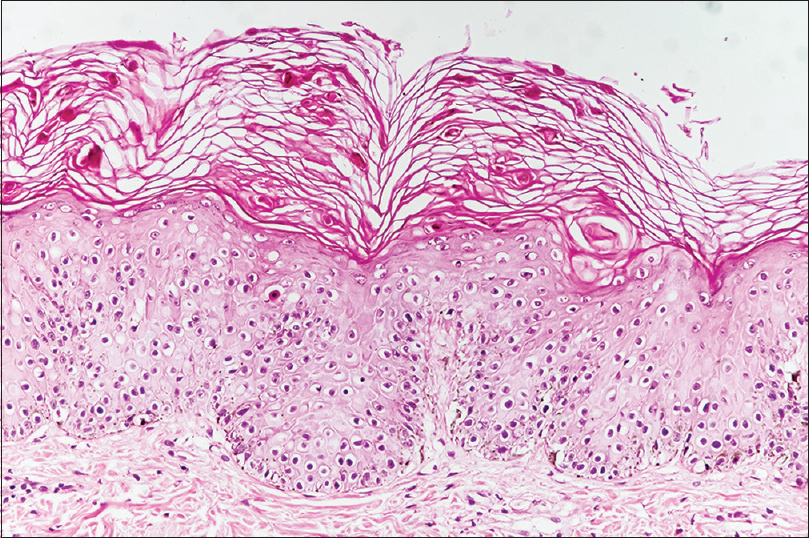 |
| Figure 3: Necrotic keratinocytes in the stratum corneum and spinous layer (H and E, ×400) |
A diagnosis of adult-onset Still's disease was considered in view of fever and polyarthritis without evidence of infection, autoimmune disease or malignancy. Her clinical and laboratory parameters fulfilled the Yamaguchi's diagnostic criteria (fulfilled three major and two minor criteria) for the disease.[1] Diagnosis was supported by very high serum ferritin level. She was started on oral steroids (prednisolone 1 mg/kg/day) and methotrexate 15mg weekly. Fever subsided in 5 days and joint pain improved with near-complete clearance of skin lesions in 1 month.
Adult-onset Still's disease is a rare systemic inflammatory disease of unknown etiology with an estimated prevalence of 1.5 cases per 100,000–1000,000 people. It has a bimodal age distribution with 2 peaks, the first peak affecting people within 15 to 25 years of age and the second peak affecting people within 36 to 46 years of age. The disease affects females more than males.[2] Severe joint pain is a prominent feature seen in all patients. The most commonly involved joints are the knees, wrists, ankles, elbows and distal interphalangeal joints of the hand. Adult-onset Still's disease is classically associated with an evanescent salmon colored rash that usually appears with the spikes of fever, but it can have atypical cutaneous manifestations in about 14% of cases. Persistent pruritic plaques some with a flagellate appearance resembling our patient have been described in various case series.[3] Other commonly reported cutaneous manifestations are nonpruritic persistant erythema,[4] urticarial papules, lichenoid papules, pigmented plaques, prurigo pigmentosa–like,[5] lichen amyloidosis like and dermatomyositis like rash with dusky red macules in photodistributed location.[3] The histopathological spectrum of cutaneous lesions of ASOD has been recently described and the characteristic histopathological features of persistent pruritic plaque have been identified as dyskeratotic keratinocytes in the upper epidermal layer in most of the cases with perivascular infiltrate of lymphocytes, neutrophils and eosinophils. Increase in dermal mucin deposition was noted in 50% of the cases.[6] This specific cutaneous feature has been found to be associated with worse prognosis and usually requires systemic treatment.[7] Management and further prognosis is determined by the extent of joint involvement. Systemic corticosteroid is the mainstay of treatment. Disease-modifying antirheumatic drugs such as methotrexate, azathioprine, cyclosporine and cyclophosphamide may be used for maintenance therapy when required.[8]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. Preliminary criteria for classification of adult Still's disease. J Rheumatol 1992;19:424-30.
[Google Scholar]
|
| 2. |
Owlia MB, Mehrpoor G. Adult-onset Still's disease: A review. Indian J Med Sci 2009;63:207-21.
[Google Scholar]
|
| 3. |
Narváez Garcia FJ, Pascual M, López de Recalde M, Juarez P, Morales-Ivorra I, Notario J, et al. Adult-onset Still's disease with atypical cutaneous manifestations. Medicine (Baltimore) 2017;96:e6318.
[Google Scholar]
|
| 4. |
Fujii K, Konishi K, Kanno Y, Ohgou N. Persistent generalized erythema in adult-onset Still's disease. Int J Dermatol 2003;42:824-5.
[Google Scholar]
|
| 5. |
Tomaru K, Nagai Y, Ohyama N, Hasegawa M, Endo Y, Tamura A, et al. Adult-onset Still's disease with prurigo pigmentosa-like skin eruption. J Dermatol 2006;33:55-8.
[Google Scholar]
|
| 6. |
Woods MT, Gavino AC, Burford HN, Hughey SL, Mercado P, Danila M, et al. The evolution of histopathologic findings in adult Still disease. Am J Dermatopathol 2011;33:736-9.
[Google Scholar]
|
| 7. |
Lee JY, Yang CC, Hsu MM. Histopathology of persistent papules and plaques in adult-onset Still's disease. J Am Acad Dermatol 2005;52:1003-8.
[Google Scholar]
|
| 8. |
Gopalarathinam R, Orlowsky E, Kesavalu R, Yelaminchili S. Adult onset Still's disease: A review on diagnostic workup and treatment options. Case Rep Rheumatol 2016;2016:6502373.
[Google Scholar]
|
Fulltext Views
4,200
PDF downloads
2,168





