Translate this page into:
Adult orbital xanthogranulomatous disease: A case report and brief discussion of the terminology
2 Ophthalmology Clinic, Istanbul Medicine Hospital, Istanbul, Turkey
3 Department of Pathology, Cerrahpaşa Medical Faculty, Istanbul University, Istanbul, Turkey
4 Department of Pathology, Acıbadem University School of Medicine, Istanbul, Turkey
Correspondence Address:
Burak Tekin
Department of Dermatology, Goztepe Research and Training Hospital, Istanbul Medeniyet University, Doktor Erkin Street, Kadikoy, 34722 Istanbul
Turkey
| How to cite this article: Tekin B, Simsek IB, Akpinar R, Demirkesen C. Adult orbital xanthogranulomatous disease: A case report and brief discussion of the terminology. Indian J Dermatol Venereol Leprol 2016;82:547-550 |
Sir,
Adult orbital xanthogranulomatous disease represents an umbrella term encompassing four distinct entities with partially overlapping clinicopathological features: adult-onset xanthogranuloma, adult-onset asthma with periocular xanthogranuloma, Erdheim–Chester disease and necrobiotic xanthogranuloma [Table - 1].[1],[2],[3],[4],[5] Among them, necrobiotic xanthogranuloma is reported to be the most common subtype. In a large series studying this spectrum of disorders, the least common type has been found to be adult-onset xanthogranuloma, and it has been largely overshadowed by necrobiotic xanthogranuloma in the existing dermatology literature.[1],[3],[4],[5] Herein, we present a further case of adult-onset xanthogranuloma and briefly discuss the spectrum of adult orbital xanthogranulomatous disease.

A 44-year-old woman presented with a 2-year-history of painless swellings first noted in the right peri-orbital region, slowly growing in size and later developing around the other eye. Her past medical history was non-contributory. Physical examination revealed yellowish plaques and papulo-nodules encircling the right eye; similar, but less conspicuous lesions were also noted around the medial canthus and on the upper eyelid of the left eye [Figure - 1]. Her vision was not affected. On palpation, the lesions were non-tender, firm and accompanied by a subcutaneous component. Incisional biopsies from the infiltrated plaques on the upper and lower eyelids on the right side revealed a diffuse infiltrate of histiocytes with xanthomatous or polygonal cytoplasm extending towards the periorbital soft tissue. The histiocytes were intermingled with aggregates of lymphocytes, plasmacytes, eosinophils and scattered Touton giant cells [Figure - 2]a. Within the infiltrate small areas of necrosis and necrobiosis were detected [Figure - 2]b. Mitotic figures were scarce. Immunohistochemical staining demonstrated the expression of CD68 in the histiocytes while S100 protein was negative. Magnetic resonance imaging demonstrated lesions protruding into the retro-orbital area as well as periorbital masses corresponding to the skin lesions [Figure - 3]. Laboratory evaluation revealed iron deficiency anemia (red blood cell: 3.94 × 106/mm 3, normal: 4.0–5.1; hemoglobin: 10.2 g/dl, normal: 11.7–15.5; ferritin: 6.75 ng/ml, normal: 15–150). Serum lipids, immunoglobulin E and protein electrophoresis were within the normal range. Based on the clinical and histopathological findings, the patient was diagnosed with adult-onset orbital xanthogranuloma. Conservative multi-step surgical excision combined with intralesional corticosteroid injections into the residual lesions were planned as treatment. No clinical or biochemical signs of asthma or hematologic abnormalities were noted during the follow-up.
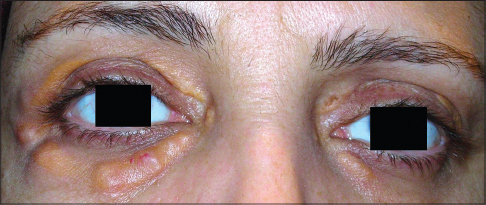 |
| Figure 1: Plaques and papulonodules with a yellow hue around both eyes, demonstrating a more prominent involvement of the upper and lower eyelids of the right eye |
 |
| Figure 2: (a) Diffuse infiltration of mostly xanthomatous histiocytes, intermingled with aggregates of lymphocytes and eosinophils. Touton giant cell is seen in the inset (H and E, ×400). (b) A small area of necrosis surrounded by palisading histiocytes (H and E, ×200) |
 |
| Figure 3: T2-weighted coronal magnetic resonance image showing a poorly delineated hyperintense mass in the right lower eyelid (indicated by the blue arrow) |
Adult orbital xanthogranulomatous diseases are collectively considered within the broader group of non-Langerhans histiocytic disorders. Although the four subtypes share clinical and histopathological findings such as the presence of S100 and CD1a negative, CD68 positive foamy histiocytes, Touton giant cells, varying degrees of fibrosis, necrosis and/or lymphocytic infiltration, they have subtle morphological differences and distinctive systemic associations [Table - 1].[1],[2] Necrobiotic xanthogranuloma typically presents with ulcerated nodules which are histopathologically characterized by the presence of necrobiosis surrounded by palisading epithelioid histiocytes, more numerous Touton giant cells and cholesterol clefts.[3] It is commonly associated with paraproteinemia and multiple myeloma.[1],[5] Erdheim–Chester disease is notable for the progressive fibrosclerosis of the orbit and carries the worst prognosis within this spectrum due to the frequent impairment of visual acuity and fibrotic involvement of internal organs.[1],[2] Adult-onset asthma with periocular xanthogranuloma, on the other hand, is frequently associated with lymphadenopathy and elevated levels of polyclonal IgG in addition to its hallmark feature of adult-onset asthma.[1] The distinctive histopathological finding in this disorder is the presence of large lymphoid aggregates with reactive germinal centers.[1],[2] Adult-onset orbital xanthogranuloma presents with isolated orbital involvement without accompanying immune dysfunction, asthma or paraproteinemia; however, hematological abnormalities such as thrombocytopenia, eosinophilia, anemia and lymphopenia have been anecdotally reported.[1],[3],[4]
Several features in the present case of adult-onset orbital xanthogranuloma deserve further mention. Clinically, the absence of paraproteinemia, asthma, lymphadenopathy or internal organ involvement was consistent with adult-onset xanthogranuloma. The iron deficiency anemia seen in this case may be an independent finding or related to the xanthogranulomatous disease, similar to previously reported cases accompanied by hematological abnormalities.[3],[4] Histopathologically, the absence of well-formed lymphoid aggregates, cholesterol clefts or prominent fibrosclerosis further supported the diagnosis of adult-onset xanthogranuloma. Differentiating it from the other subtypes of adult orbital xanthogranulomatous disease, necrobiosis is a more salient feature of necrobiotic xanthogranuloma. However, small necrobiotic foci have also been described in adult-onset xanthogranuloma, as in our case.[3] Tang et al. speculated that adult-onset xanthogranuloma and necrobiotic xanthogranuloma possibly represent two poles of a spectrum with the latter representing the severe form. Our case may be considered to lie between these two poles due to the presence of necrobiosis and anemia. Although progression to necrobiotic xanthogranuloma has not been documented in a small case series of adult-onset xanthogranuloma, we think that long-term follow-up for paraproteinemia appears prudent in cases such as ours.[3]
Depending on the subtype and severity of involvement, a number of treatment modalities have been used in adult orbital xanthogranulomatous disease with varying success including surgery, intralesional corticosteroid injections, systemic corticosteroids, chemotherapeutic agents and/or radiation.[1],[2],[3],[4] Ocular symptoms should also be addressed, emphasizing the importance of co-operation between the dermatologist and the ophthalmologist.
In conclusion, adult orbital xanthogranulomatous disease is a heterogeneous entity that should prompt a thorough evaluation for potential systemic associations. Clinicopathological correlation is important for the diagnosis and sub-classification of this rare condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sivak-Callcott JA, Rootman J, Rasmussen SL, Nugent RA, White VA, Paridaens D, et al. Adult xanthogranulomatous disease of the orbit and ocular adnexa: New immunohistochemical findings and clinical review. Br J Ophthalmol 2006;90:602-8.
[Google Scholar]
|
| 2. |
Guo J, Wang J. Adult orbital xanthogranulomatous disease: Review of the literature. Arch Pathol Lab Med 2009;133:1994-7.
[Google Scholar]
|
| 3. |
Tang WK, Lee KC, Chong LY. Three patients with orbital xanthogranuloma and non-progressive haematological abnormalities. Australas J Dermatol 2003;44:185-9.
[Google Scholar]
|
| 4. |
Shimizu F, Taneda H, Sato H, Kato A, Takeo N, Fujiwara S. A Case of orbital xanthogranuloma treated by surgical excision. Case Rep Dermatol 2010;2:110-5.
[Google Scholar]
|
| 5. |
Minami-Hori M, Takahashi I, Honma M, Ito Y, Takahashi H, Ishida-Yamamoto A, et al. Adult orbital xanthogranulomatous disease: Adult-onset xanthogranuloma of periorbital location. Clin Exp Dermatol 2011;36:628-31.
[Google Scholar]
|
Fulltext Views
4,729
PDF downloads
1,626





