Translate this page into:
Aggressive erosive lichen planus associated with hepatitis C responding to sofosbuvir/ledipasvir treatment
Correspondence Address:
Pilar Iranzo
Department of Dermatology, Hospital Clínic de Barcelona, Universitat de Barcelona, Calle Villarroel 170, Barcelona 08036
Spain
| How to cite this article: Morgado-Carrasco D, Combalia A, Fustà-Novell X, Mascaró Jr JM, Iranzo P. Aggressive erosive lichen planus associated with hepatitis C responding to sofosbuvir/ledipasvir treatment. Indian J Dermatol Venereol Leprol 2019;85:326-329 |
Sir,
Hepatitis C virus infection can induce several extrahepatic manifestations including dermatologic conditions such as lichen planus, porphyria cutanea tarda and cryoglobulinemia.[1] Here we present a patient with chronic hepatitis C virus infection who developed an aggressive form of lichen planus and achieved clinical resolution after therapy with direct-acting antivirals.
A woman in her 80s presented with painful ulcers in her mouth, legs, feet and genitalia [Figure - 1]a of 8 weeks duration. Severe paronychia with erosions leading to loss of her first, second and third toenails was also observed since 4 weeks [Figure - 1]b. She had well-controlled type 2 diabetes mellitus with chronic renal failure and was on insulin glargine therapy. The patient also suffered from chronic hepatitis C virus infection which she developed secondary to a transfusion performed 60 years previously. Histologic examination of a punch biopsy from the ulcer on the right foot showed acanthosis with hyperkeratosis, hypergranulosis, saw-tooth appearance and subepidermal clefting. A band-like inflammatory infiltrate and vacuolar basal layer degeneration was observed in the superficial dermis. Direct immunofluorescence examination revealed shaggy linear basement membrane deposition of fibrinogen and abundant colloid bodies in the papillary dermis (IgM) [Figure - 2]. These findings ruled out an autoimmune blistering disease and inflammatory dermatoses such as parakeratosis pustulosa, acrodermatitis continua of Hallopeau and necrolytic acral erythema. On the basis of the clinical and pathological features, a diagnosis of erosive lichen planus was made. Considering the co-existing diabetes and chronic renal failure, oral corticosteroids or cyclosporine were not prescribed and the patient was also reluctant to take hydroxychloroquine. Though mycophenolate mofetil tablets were initiated in a dose of 500 mg twice daily with mild clinical response, it had to be discontinued subsequently due to pancytopenia. Laboratory work-up revealed transaminitis (γ-glutamyl transpeptidase 233 U/L, aspartate aminotransferase 53 U/L; reference value 5–40 U/L), reactive hepatitis C virus antibodies and a hepatitis C virus viral load of 1,053,000 copies/mL. Hepatitis C virus genotype was 1b. Serologies ruled out hepatitis B viral infection and HIV. Zinc levels were not measured as the patient did not seem to be at increased risk for nutritional deficiency (alcoholism, poor diet, malabsorptive disorders or malignancies). As we suspected that the hepatitis C viral infection was contributing to aggressive course of her disease, the patient was sent to Hepatology Department, where hepatic cirrhosis was confirmed by ultrasonography. Direct-acting antiviral therapy with sofosbuvir 90 mg/day and ledipasvir 400 mg/day for 24 weeks was initiated. No treatment with oral or topical corticosteroids or immunosuppressants was given at this point. Four weeks later, transaminases had normalized and she had an undetectable viral load and cutaneous and mucosal lesions started to heal. There was complete resolution of the cutaneous, oral and genital mucosal erosions in the following 2 months [Figure - 3]. The patient remained asymptomatic, maintained an undetectable viral load and achieved sustained virological response 24 weeks (SVR24) after completion of antiviral therapy. Hepatitis C virus infection was declared cured and the patient has been asymptomatic with no mucocutaneous lesions at 12 months follow-up after direct-acting antiviral withdrawal.
 |
| Figure 1: |
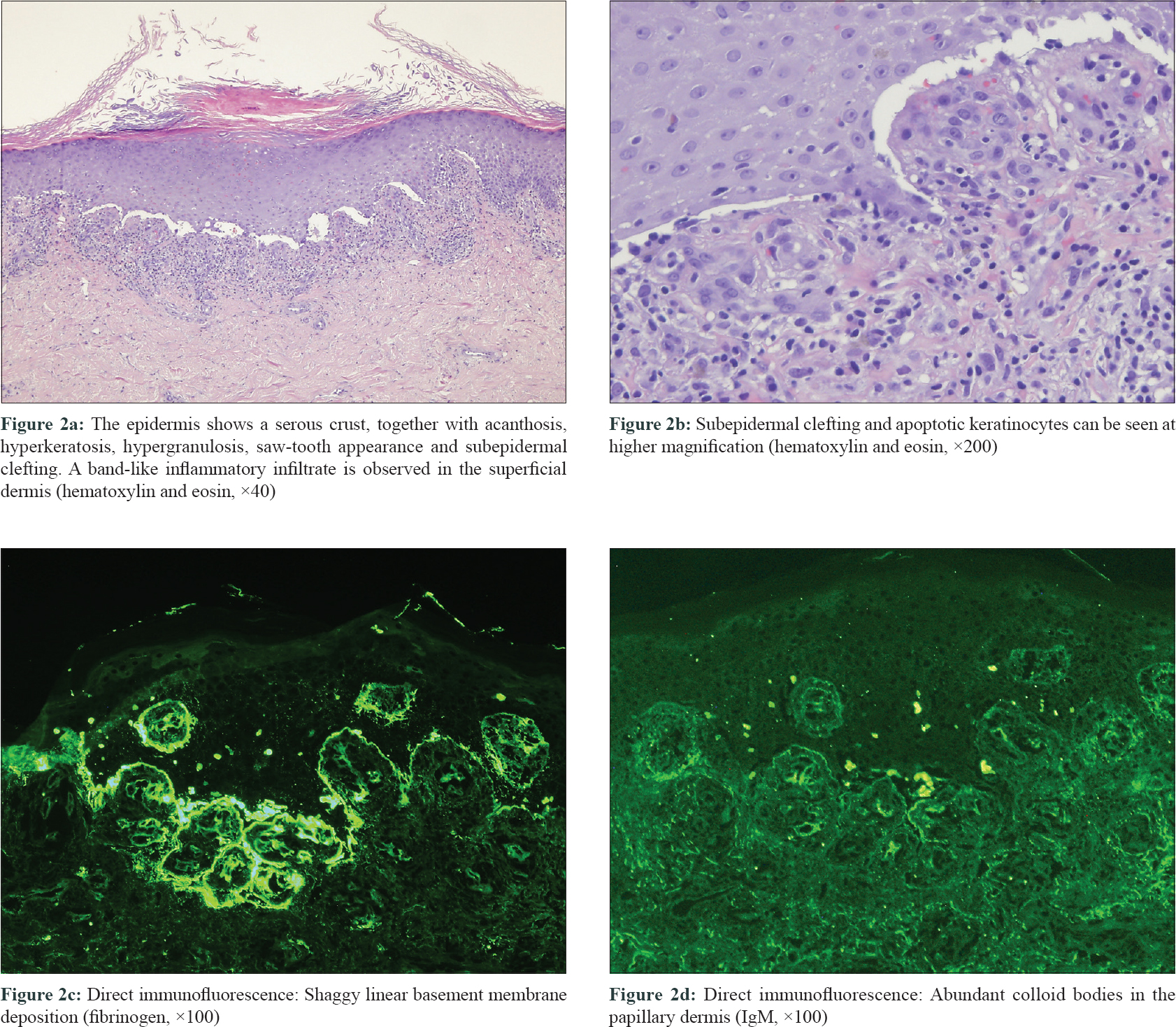 |
| Figure 2: |
 |
| Figure 3: Resolution of cutaneous erosions in feet after treatment of hepatitis C viral infection with sofosbuvir/ledipasvir |
Studies have shown that introduction of direct-acting antiviral agents has dramatically improved the management of hepatitis C virus infection with sustained virologic response in more than 90% of cases.[2],[3]
The etiology of lichen planus is not fully understood. Lichen planus is an autoimmune disease that can affect the oral and genital mucosa, skin, scalp and nails. Hepatitis C virus-associated lichen planus tends to be chronic and is characterized by a higher prevalence of erosive-ulcerative lesions and poorer treatment outcomes compared to idiopathic lichen planus.[1]
Another dermatosis that has been associated with hepatitis C virus infection is necrolytic acral erythema, and is a differential diagnosis to consider in this scenario. Necrolytic acral erythema is characterized by erythematous plaques and papules most commonly affecting the dorsal aspect of the feet and hands. It also occurs on the shins. Necrolytic acral erythema does not affect the nail bed, nail plate or mucous membranes.[4],[5],[6] Our patient presented with lesions on mucous membranes (oral, genital and anal), cutaneous lesions on the legs and severe nail involvement. Furthermore, histologic findings reported in necrolytic acral erythema are epidermal pallor, necrotic keratinocytes and pigment incontinence, among others[4],[6] while the histologic findings and direct immunofluorescence findings from our patient were highly consistent with lichen planus.
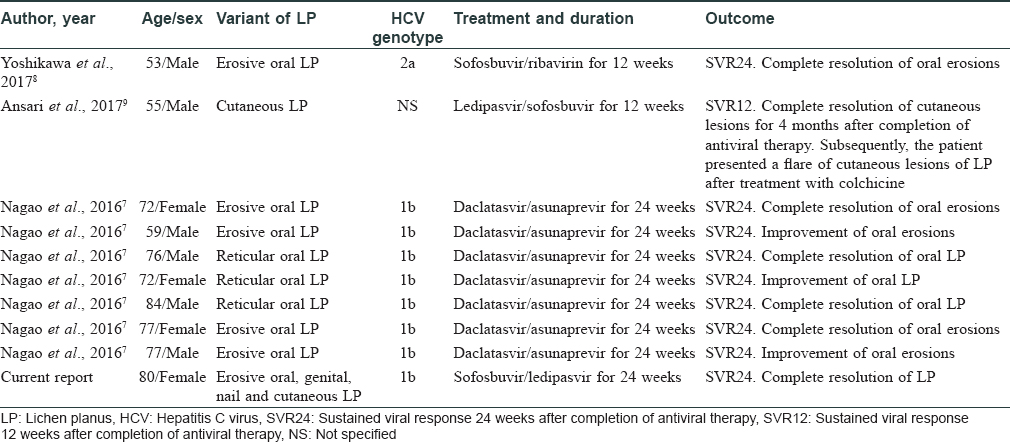
Improvement of skin disorders associated with hepatitis C virus after successful treatment with direct-acting antiviral has been recently reported. Nagao et al. described a series of seven patients diagnosed with oral lichen planus treated with daclatasvir/asunaprevir with complete clinical resolution in four patients and improvement in the other three [Table - 1].[7] In addition, two patients (one case with cutaneous lichen planus and another with erosive oral lichen planus) who had complete resolution of their cutaneous or oral lesions after direct-acting antiviral therapy have recently been described.[8],[9] However, there is also a report of a 55-year-old male with hepatitis C virus and a 30-year history of oral lichen planus developing widespread cutaneous lichen planus lesions following treatment with ledipasvir/sofosbuvir though the treatment had cured the Hepatitis C.[10] To date, there are no reported cases of patients with severe nail lichen planus and hepatitis C virus healing with direct-acting antiviral agents.
Other dermatoses associated with hepatitis C virus have also benefited from direct-acting antiviral therapy: remission of porphyria cutanea tarda secondary to hepatitis C virus infection was observed in 16 patients after treatment with direct-acting antiviral agents.[11] In a study of 35 patients with symptomatic cryoglobulinemia where 23 of them presented as cutaneous purpura, more than 90% achieved clinical remission after treatment with different combinations of direct-acting antiviral agents.[2]
Multiple studies have reported an association between diabetes mellitus and lichen planus,[12] although it is not well established if poor glycemic control can lead to a more aggressive course of lichen planus.[13] In our case, it is unlikely that diabetes mellitus had played a role in the aggressive course of lichen planus, since the patient presented with good glycemic control.
We have presented a case where a direct-acting antiviral regime, with no concomitant use of corticosteroids or immunosuppressants, has cured an aggressive cutaneous variant of lichen planus. Direct-acting antivirals are safe and highly effective against hepatitis C virus infection and could lead to remission of hepatitis C virus-associated dermatologic conditions. Lichen planus is a common dermatosis; we recommend screening for hepatitis C virus in all cases of severe or refractory lichen planus and initiating treatment with direct-acting antiviral agents in patients with associated hepatitis C virus infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Garcovich S, Garcovich M, Capizzi R, Gasbarrini A, Zocco MA. Cutaneous manifestations of hepatitis C in the era of new antiviral agents. World J Hepatol 2015;7:2740-8.
[Google Scholar]
|
| 2. |
Bonacci M, Lens S, Londoño MC, Mariño Z, Cid MC, Ramos-Casals M, et al. Virologic, clinical, and immune response outcomes of patients with hepatitis C virus-associated cryoglobulinemia treated with direct-acting antivirals. Clin Gastroenterol Hepatol 2017;15:575-830.
[Google Scholar]
|
| 3. |
Tamori A, Enomoto M, Kawada N. Recent advances in antiviral therapy for chronic hepatitis C. Mediators Inflamm 2016;2016. Article ID: 6841628.
[Google Scholar]
|
| 4. |
Nofal AA, Nofal E, Attwa E, El-Assar O, Assaf M. Necrolytic acral erythema: A variant of necrolytic migratory erythema or a distinct entity? Int J Dermatol 2005;44:916-21.
[Google Scholar]
|
| 5. |
Patel U, Loyd A, Patel R, Meehan S, Kundu R. Necrolytic acral erythema. Dermatol Online J 2010;16:15.
[Google Scholar]
|
| 6. |
Abdallah MA, Ghozzi MY, Monib HA, Hafez AM, Hiatt KM, Smoller BR, et al. Necrolytic acral erythema: A cutaneous sign of hepatitis C virus infection. J Am Acad Dermatol 2005;53:247-51.
[Google Scholar]
|
| 7. |
Nagao Y, Kimura K, Kawahigashi Y, Sata M. Successful treatment of hepatitis C virus-associated oral lichen planus by interferon-free therapy with direct-acting antivirals. Clin Transl Gastroenterol 2016;7:e179.
[Google Scholar]
|
| 8. |
Yoshikawa A, Terashita K, Morikawa K, Matsuda S, Yamamura T, Sarashina K, et al. Interferon-free therapy with sofosbuvir plus ribavirin for successful treatment of genotype 2 hepatitis C virus with lichen planus: A case report. Clin J Gastroenterol 2017;10:270-3.
[Google Scholar]
|
| 9. |
Ansari U, Henderson LI, Stott G, Parr K. Treatment with ledipasvir-sofosbuvir for hepatitis C resulting in improvement of lichen planus. JAAD Case Rep 2017;3:67-9.
[Google Scholar]
|
| 10. |
Scott GD, Rieger KE. New-onset cutaneous lichen planus following therapy for hepatitis C with ledipasvir-sofosbuvir. J Cutan Pathol 2016;43:408-9.
[Google Scholar]
|
| 11. |
Combalia A, To-Figueras J, Laguno M, Martínez-Rebollar M, Aguilera P. Direct-acting antivirals for hepatitis C virus induce a rapid clinical and biochemical remission of porphyria cutanea tarda. Br J Dermatol 2017;177:e183-4.
[Google Scholar]
|
| 12. |
Mozaffari HR, Sharifi R, Sadeghi M. Prevalence of oral lichen planus in diabetes mellitus: A meta-analysis study. Acta Inform Med 2016;24:390-3.
[Google Scholar]
|
| 13. |
Romero MA, Seoane J, Varela-Centelles P, Diz-Dios P, Garcia-Pola MJ. Prevalence of diabetes mellitus amongst oral lichen planus patients. Clinical and pathological characteristics. Med Oral 2002;7:121-9.
[Google Scholar]
|
Fulltext Views
4,311
PDF downloads
2,445





