Translate this page into:
Alopecia areata progressing to totalis/universalis in non-insulin dependent diabetes mellitus (type II): Failure of dexamethasone-cyclophosphamide pulse therapy
Correspondence Address:
Virendra N Sehgal
Sehgal Nursing Home, A/6, Panchwati, Azadpur, Delhi - 110 033
India
| How to cite this article: Sehgal VN, Bhattacharya SN, Sharma S, Srivastava G, Aggarwal AK. Alopecia areata progressing to totalis/universalis in non-insulin dependent diabetes mellitus (type II): Failure of dexamethasone-cyclophosphamide pulse therapy. Indian J Dermatol Venereol Leprol 2008;74:171-173 |
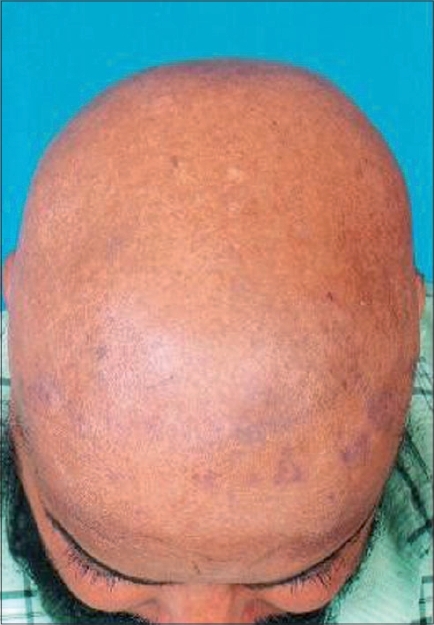 |
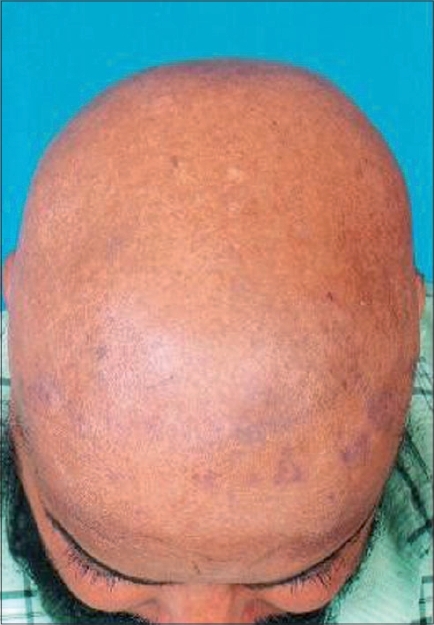
| Figure 1: Alopecia areata progressing to totalis/universalis: Complete loss of hair over the scalp |
 |
| Figure 1: Alopecia areata progressing to totalis/universalis: Complete loss of hair over the scalp |
Sir,
The development of alopecia areata (AA) progressing to totalis/universalis in well-established non-insulin-dependent diabetes mellitus (NIDDM, type II) is an exclusive phenomenon, an indirect circumstantial evidence favoring it as an autoimmune disease. Dexamethasone-cyclophosphamide pulse was initiated but failed to produce a response.
A 47-year-old man, apparently well until a year ago had a few recalcitrant multiple boils on the nape of the neck. His fasting and postprandial blood sugar levels were markedly elevated pointing to a diagnosis of NIDDM, for which oral anti-diabetics (metformin 500 mg + glipizide 5 mg), along with dietary advice and appropriate oral and topical antibiotics were started. The preceding treatment ensured complete healing of the boils within 2 weeks. Four months later, he experienced spontaneous loss of hair over the legs progressing to involve other sites. In a short period of time, hair loss was noticed over the trunk, scalp and the beard area. It was accompanied by mild to moderate itching. However, hair loss was not preceded by any perifollicular papular or pustular lesions. The loss of hair over the scalp was total and was a source of embarrassment, which brought him for consultation. Examination of the skin was marked by loss of hair over the whole of the skin surface of the trunk, upper and lower extremities with patches of hair loss over the beard area. Hair pull test was positive. The complete loss of hair over the scalp was without any evidence of scarring or any skin lesion [Figure - 1], which was characteristic of AA. Routine total and differential leukocyte count, complete hemogram and blood biochemical parameters were within normal limits. However, his random blood sugar was 197 mg (normal up to 140) and glycosylated hemoglobin (HbA1c) was 9.6 percent (normal 9%-10% fair glycemic control). The hematoxylin eosin stained biopsy section from the area of hair loss showed dense lymphocytic infiltrate in the dermis involving the receding remnant of hair follicles.
Dexamethasone cyclophosphamide pulse (DCP) therapy was opted for the treatment of extensive AA as it has successfully been used for bullous autoimmune dermatoses, [1],[2] including pemphigus vulgaris. Moreover, side-effect profile is considered to be less severe with the pulse form than the conventional daily dosing of corticosteroids. It comprised 100 mg of dexamethasone dissolved in 5% dextrose administered intravenously over 3-4 h on three consecutive days plus intravenous 500 mg of cyclophosphamide administered on day 2 only, followed by daily oral 50 mg cyclophosphamide. The effect of administration of dextrose and concomitant NIDDM was neutralized by simultaneous administration of 16 units of human mono-component regular insulin. About three such doses (cycles) were contemplated at intervals of 1 month each. Besides, he was maintained on oral anti-diabetics comprising metformin and glipizide. The patient was advised to come for follow-up every month till the completion of 1 year. A thorough examination of the scalp and rest of the skin surface was conspicuous by the absence of any hair growth, signaling the failure of dexamethasone-cyclophosphamide pulse therapy.
Alopecia areata is a well-recognized clinical entity characterized by non-scarring round and/or oval patches of hair loss. However, an exclamation mark at the active hair margin is its diagnostic hallmark. The lesions are largely asymptomatic, which may manifest either as alopecia areata (classic, reticulate AA, alopecia totalis/universalis or ophiasis and ophiasis in versa). [3]
A number of associations have been reported with diabetes mellitus, including a series of cutaneous disorders like candida endocrinopathy syndrome, lichen planus, lupus erythematosus and vitiligo. [4] While AA and vitiligo are markers of auto-immunity in insulin-dependent diabetes mellitus (Type I), [5],[6],[7] the association of AA and NIDDM type II is extraordinary and hitherto has never been emphasized.
Most effective therapies for AA have immunosuppression as a common denominator. However, the failure of DCP pulse therapy in our patient supports equivocal outcome reported following prednisolone as a single 2 g dose intravenously (i.v.)/0.5 g daily for 5 days orally. [8] Nonetheless, the proposed role of DCP as a treatment option in the management of AA per se or in association with other auto-immune disease needs to be evaluated in a larger number of patients. This is particularly because its efficacy in auto-immune diseases like systemic sclerosis/scleroderma, [9],[10],[11] paraneoplastic pemphigus [12] and discoid lupus erythematosus [13] was admirably established.
| 1. |
Raman M. Dexamethasone pulse therapy in dermatology. Indian J Dermatol Venereol Leprol 2003;69:319-22.
[Google Scholar]
|
| 2. |
Appelhans M, Monsmann G, Orge, Brocker EB. Dexamethasone-cyclophosphamide pulse therapy in bullous autoimmune dermatoses. Hautarzt 1993;44:143-7.
[Google Scholar]
|
| 3. |
Sehgal VN, Srivastava G, Aggarwal AK, Sethi G, Adhikari T. Alopecia areata in the Indian subcontinent. Skinmed 2007;6:63-9
[Google Scholar]
|
| 4. |
Sehgal VN, Jain S. Alopecia areata: Clinical perspective and an insight into pathogenesis. J Dermatol (Tokyo) 2003;30:271-89.
[Google Scholar]
|
| 5. |
Sipetic S, Vlajinac H, Kocev N, Marinkovic J, Radmanovic S, Denic L. Family history and risk of type 1 diabetes mellitus. Acta Diabetol 2002;39:111-5.
[Google Scholar]
|
| 6. |
Flagothier C, Quatresooz P, Bourguignon R, Pierard-Franchimont C, Pierard GE. CHR hutois: Cutaneous stigmata of diabetes mellitus. Rev Med Liege 2005;60:553-9.
[Google Scholar]
|
| 7. |
Wong J, Shohat T, Vadheim C, Shellow W, Edwards J, Rotter JI. Increased risk of type-I (insulin dependent) diabetes in relatives of patients with alopecia areata. Am J Med Genet 1994;51:234.
[Google Scholar]
|
| 8. |
Burton JL, Shuster S. Large doses of glucocorticoid in the treatment of alopecia areata. Acta Derm Venereol 1975;55:493-6.
[Google Scholar]
|
| 9. |
Sharda B, Kumar A, Kakkar R, Adya CM, Pande I, Uppal SS, et al . Intervenous dexamethasone pulse therapy in diffuse systemic scleroses: A randomized placebo-controlled study. Rheumatol Internal 1994;14:91-4.
[Google Scholar]
|
| 10. |
Pai BS, Srinivas CR, Sabitha L, Shenoi SD, Balachandran CN, Acharya S. Efficacy of dexamethasone pulse therapy in progressive systemic sclerosis. Int J Dermatol 1995;34:726-8.
[Google Scholar]
|
| 11. |
Vatwani V, Palta SC, Verma N, Pathak PR, Singh RP. Pulse therapy in scleroderma. Indian Pediatr 1994;31:993-5.
[Google Scholar]
|
| 12. |
Becker LR, Bastian BC, WEsselmann U, Karl S, Hamm H, Brocker EB. Paraneoplastic pemphigus treated with dexamethasone / cyclopho: Asphamide pulse therapy. Eur J Dermatol 1998;8: 551-3.
[Google Scholar]
|
| 13. |
Singh OP, Vema KK. Discoid lupus erythematosus treated with dexamethasone pulse therapy. Indian J Dermatol Venereol Leprol 1991;57:311.
[Google Scholar]
|
Fulltext Views
2,965
PDF downloads
1,765





