Translate this page into:
Amoebiasis cutis in HIV positive patient
Correspondence Address:
R A Bumb
H-3, Hospital campus, P. B. M. Hospital, Bikaner 334 003, Rajasthan
India
| How to cite this article: Bumb R A, Mehta R D. Amoebiasis cutis in HIV positive patient. Indian J Dermatol Venereol Leprol 2006;72:224-226 |
Abstract
Protozoan infections of the skin, particularly cutaneous amoebiasis, are rare in HIV-positive patients. We report a case of amoebiasis cutis in an HIV-positive truck driver with a history of frequent unprotected sexual exposures. He presented with multiple painful ulcers and sinuses with purulent discharge, necrotic slough and scarring in the perianal and gluteal region for the last 2 years. He was positive for HIV-1 and -2. Cutaneous biopsy revealed numerous Entamoeba histolytica in the trophozoite form, in addition to an inflammatory infiltrate and necrotic debris. He responded well to oral metronidazole and chloroquine. Amoebiasis cutis should be considered in the differential diagnosis of perianal ulcers, particularly in HIV-positive patients.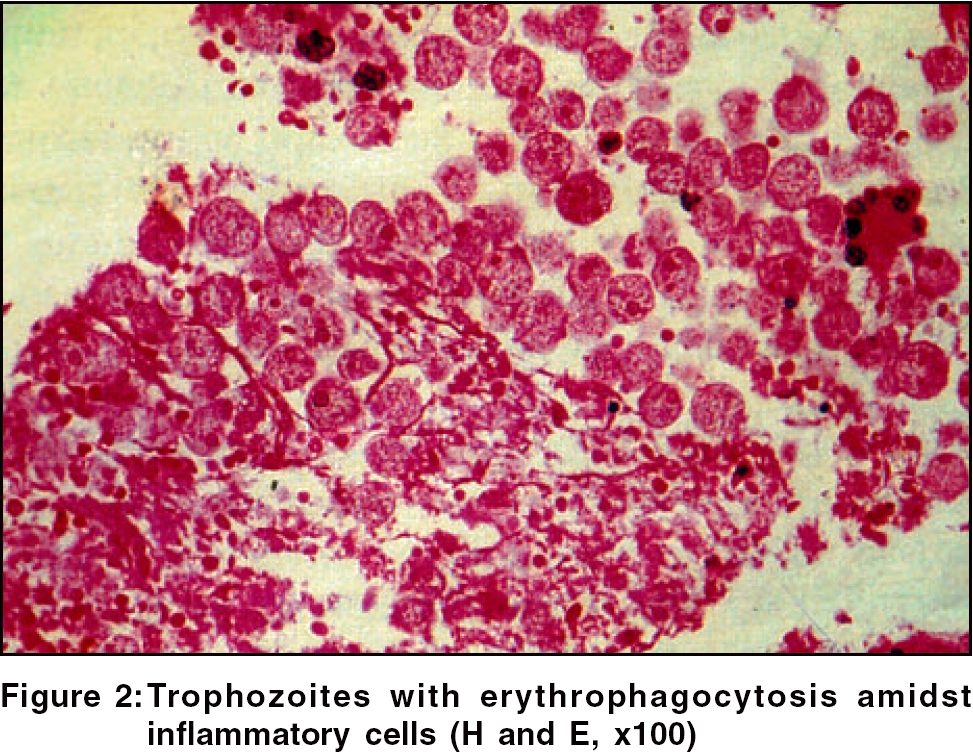 |
 |
 |
 |
Introduction
Protozoan opportunistic infections in HIV-positive patients usually manifest as gastrointestinal disease. Entamoeba histolytica infection of the large intestine is common in patients suffering from HIV infection, particularly in a tropical climate, but cutaneous involvement is very rare.[1],[2] The infection can be sexually transmitted or can be caused by spread from the large intestine in immunocompromised patients. Cutaneous amoebiasis occurs when the invasive amoebae escape from the large gut and stick to adjacent skin, usually the perianal and perigenital area. They cause lysis of the skin and subcutaneous tissue, leading to ulceration and necrosis.[2] There are only scattered reports of cutaneous amoebiasis in immunocompetent patients[3],[4] and none in HIV-positive patients in India. This prompted us to report this interesting case.
Case report
A 35-year-old married male truck driver came to the skin outpatient department with complaints of multiple painful perianal ulcers. To start with, there were only two painful ulcers, with a purulent discharge, but they had gradually increased in number and size for the last 2 years to the present dimension.
He gave a history of heterosexual extramarital contact with sex workers on multiple occasions but not of homosexuality. He was a chronic alcoholic and smoker. He used to take meals at roadside restaurants frequently and had diarrhea off and on, for which he had never sought treatment. He had been treated by general practitioners with oral antibiotics, antifungals, anti-inflammatory drugs and a variety of topical agents for his perianal ulcers with only partial relief in symptoms.
On examination, the patient was fairly built, poorly nourished, grossly anemic, emaciated and lethargic. He was afebrile with normal pulse, blood pressure and respiration. Systemic examination revealed mild hepatomegaly.
On the perianal and gluteal region, he had multiple tender ulcers varying in size from 4 to 6 cm in diameter with ragged irregular margins and covered with necrotic slough [Figure - 1]. On removal of the slough, unhealthy granulation tissue was seen. On pressing the skin between the ulcers, pus oozed out from many sinuses. Old scars were also present. Proctoscopy demonstrated only hyperemic mucous membrane. No growth or ulceration was seen. The regional lymph nodes were not enlarged.
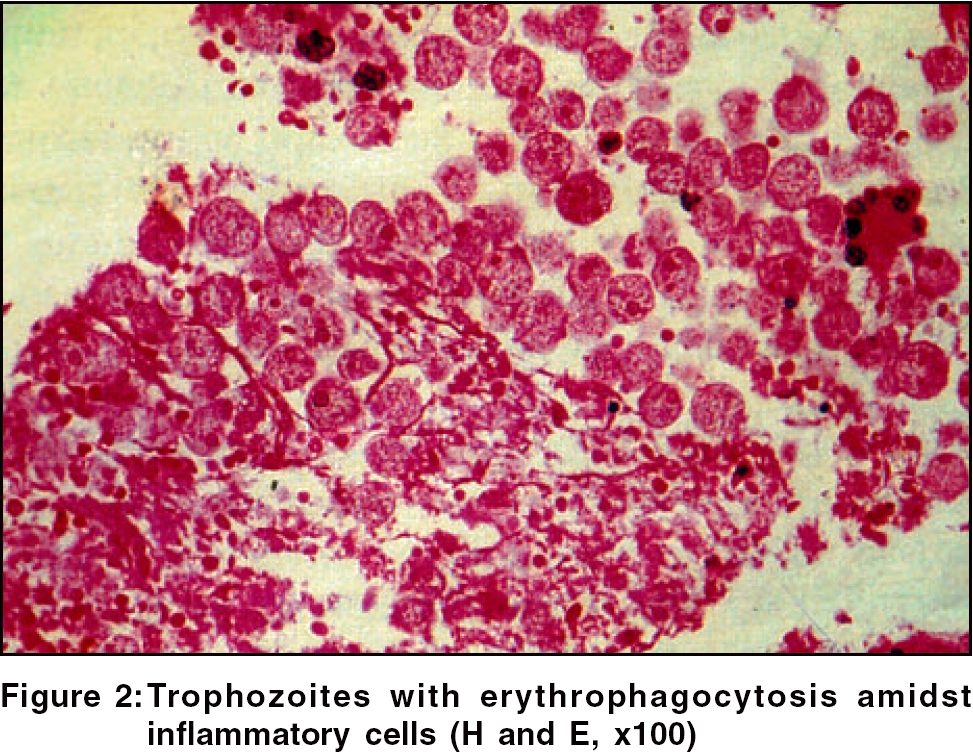
Investigation showed anemia (Hb, 9.5 gm%), leukocytosis (12500/cmm) with lymphocytosis (lymphocytes, 65%) and raised ESR (68 mm/hour). The VDRL test was nonreactive. The patient was positive for HIV-1 and -2 by the Rapid Card test and by ELISA. Viral load and CD+4 counts were not done because of lack of facilities. The urine examination was normal. Stool examination, performed on three consecutive days, showed cysts and trophozoites of amoebae. Ultrasonography of the abdomen showed mild hepatomegaly. Pus culture from the ulcer was sterile. A biopsy from the margin of ulcer stained with H and E showed amoebae in the trophozoite form with phagocytosed RBCs [Figure - 2] in addition to necrotic debris and infiltration with lymphocytes and plasma cells. The chest X-ray PA view was normal. The Mantoux test was negative.
The history and findings of the stool examination and tissue biopsy led us to arrive at a provisional diagnosis of cutaneous amoebiasis. He was prescribed oral metronidazole 800 mg thrice daily for 10 days and then chloroquine 250 mg twice daily for 21 days. In 2 months there was complete healing with scarring. The patient was asymptomatic at 12 weeks′ follow-up.
Discussion
Diagnosis of cutaneous amebiasis is commonly missed. In our patient, the history of unprotected sexual exposure on multiple occasions led us to suspect an unusual presentation of late stage lymphogranuloma venereum. Although the history of recurrent diarrhea and the presence of E. histolytica in the stools should have made us suspect cutaneous amoebiasis, we did not do so because intestinal amoebiasis is common in our region. We did not perform a wet smear from the ulcers because we never suspected amoebiasis. Cutaneous amoebiasis was finally diagnosed on the basis of the histopathological findings.
Cutaneous amoebiasis develops when amoebae escape to the contiguous skin from bowel. It presents as ulcerated granulomatous lesions with necrotic slough around anus and gluteal region. The ulcers have thickened and undermined margins with seropurulent discharge and necrotic debris. The findings of our case are corroborative with the previous reports. The recommended treatment is metronidazole 800 mg three times a day for 10 days. We gave chloroquine in addition to metronidazole because this case was HIV-positive.
Cutaneous amoebiasis may be under-diagnosed because it is rare. Although cutaneous amoebiasis is uncommon even in immunocompromised patients, including those with AIDS,[1],[2] the association of cutaneous amoebiasis and HIV infection is likely to be more than just a coincidence. However, there are only two Indian reports of cutaneous amoebiasis in immunocompetent patients;[3],[4] as in our case, amoebiasis was not suspected on clinical grounds.
Regional lymph nodes are enlarged in perianal amebic ulcer, usually because of secondary bacterial infection. However, in our patient, the regional lymph nodes were not enlarged. This may be because of frequent antibiotic use by the patient.
Paltiel et al .[5] and Torno et al .[6] reported cutaneous acanthamoebiasis with a similar clinical picture in AIDS patients. In their patients, cutaneous involvement was one of the manifestations of disseminated disease, while in our patient it was purely a cutaneous disease. In our patient, a biopsy showed erythrophagocytosed trophozoites, which is a finding specific to amoebiasis. In amoebiasis, there is a mixed scattered infiltrate, while acanthamoebiasis produces granulomatous inflammation. We excluded lymphogranuloma venereum, Crohn′s disease, tuberculosis, malignancy and perianal herpes on the basis of the clinical features, investigations and treatment.
The aim of reporting this case is that in the era of HIV infection, we should consider cutaneous amoebiasis in the differential diagnosis of perianal ulcers.
| 1. |
Maniar JK. Clinical presentation of HIV infection. In : Sharma VK, editor. Sexually Transmitted Disease and AIDS. 1st ed. Viva Books Pvt Ltd; 2003. p. 82-3.
[Google Scholar]
|
| 2. |
Bryceson AD, Hay RJ. Parasitic worms and protozoa. In: Champion RH, Burton JL, Burns DA. Breathnach SM, editors. Rook/ Wilkinson/ Ebling Textbook of dermatology. 6th ed. Blackwell Science: Oxford; 1998. p. 1404-6.
[Google Scholar]
|
| 3. |
Chandrasekhar HR, Shashikala P, Kumar P. Cutaneous amoebiasis masquerading as epithelioma. Indian J Dermatol Venereol Leprol 1993;59:254-5.
[Google Scholar]
|
| 4. |
Prasad S, Grover PS, Sharma A, Verma DK, Sharma A. Primary cutaneous amoebiasis. Case report with review of literature. Int J Dermatol 2002;41:676-80.
[Google Scholar]
|
| 5. |
Paltiel M, Powell E, Lynch J, Baranowski B, Martin C. Disseminated cutaneous acanthamoebiasis. A case report and review of literature. Cutis 2004;73:241-8.
[Google Scholar]
|
| 6. |
Torno MS Jr, Badapour R, Gurevitch A, Witt MD. Cutaneous acanthamoebiasis in AIDS. J Am Acad Dermatol 2000;42:351-4.
[Google Scholar]
|
Fulltext Views
3,697
PDF downloads
1,975





