Translate this page into:
An annoying mass of the nail bed
Correspondence Address:
Marco Adriano Chessa
Department of Experimental, Diagnostic and Specialty Medicine, University of Bologna, Via Massarenti, 1 – 40138 Bologna
Italy
| How to cite this article: Dika E, Chessa MA, Fanti PA, Alessandrini A, Starace M, Piraccini BM. An annoying mass of the nail bed. Indian J Dermatol Venereol Leprol 2018;84:244-246 |
A 56-year-old patient was referred to our unit for a bothersome, mass located under the left thumb nail, of 3 years duration [Figure - 1]a. The patient reported that the lesion was painful. Over time, multiple cultures were done from the lesion and it was diagnosed as bacterial infection, onychomycosis etc. Many topical antiseptics, systemic antibiotics and antifungals were prescribed which would induce a temporary reduction in the pain and other symptoms, but without complete resolution. On clinical examination, the nail plate appeared detached with an underlying bleeding mass; lymphadenopathy was not detected on axillary palpation. Onychoscopy showed a wide area of onycholysis with a homogeneous, mainly violaceous blotchy area beneath [Figure - 1]b. X-ray of the digit did not reveal any bony erosions. Finally, removal of the detached part of the nail plate revealed a pinkish-red nodule originating from the nail bed, 2.5 mm in width [Figure - 1]c. A punch biopsy was performed from the nodule, histopathologic examination of which showed proliferation of atypical epithelial cells infiltrating the nail bed stroma [Figure - 2]a.
 |
| Figure 1a: Frontal clinical view shows a hyperkeratotic mass under the nail plate |
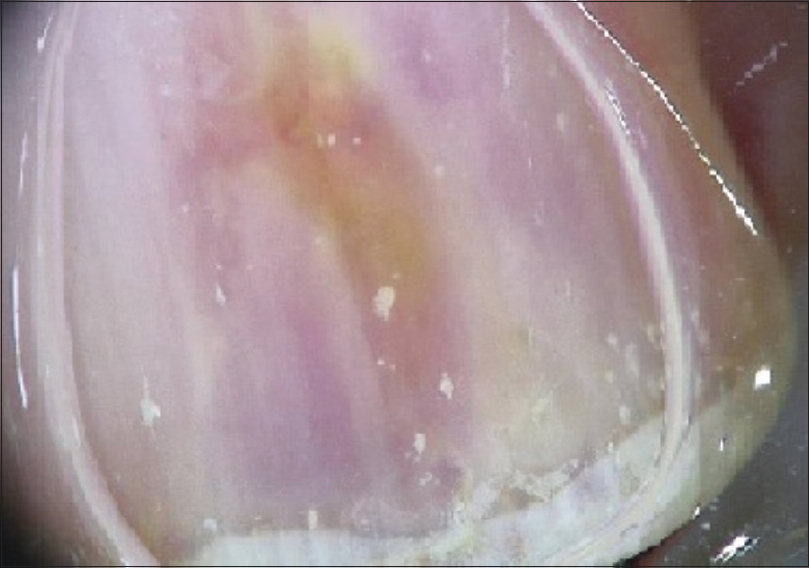 |
| Figure 1b: Onychoscopy shows a violaceus longitudinal band with a modest yellow discolaration |
 |
| Figure 1c: Removal of the detached nail plate shows an ulcerated bleeding nodule |
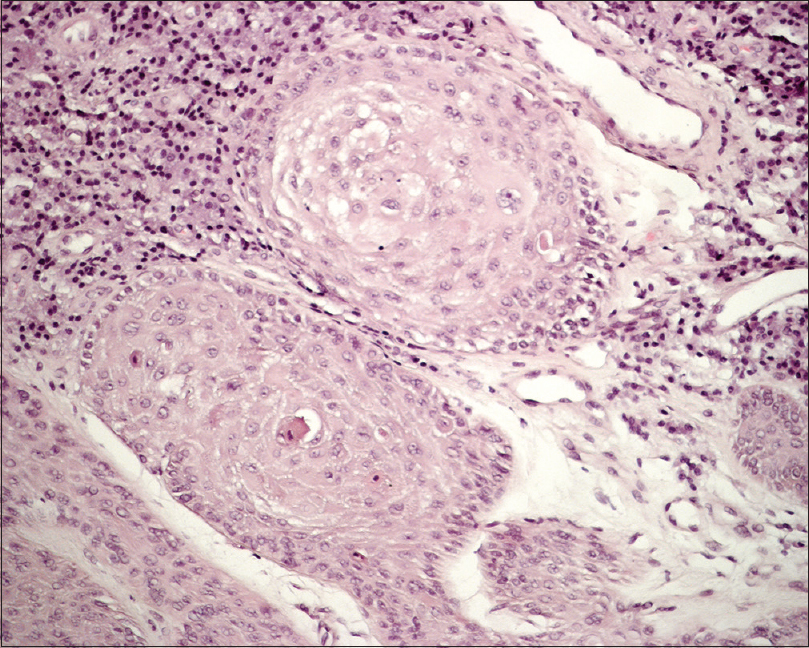 |
| Figure 2a: Proliferation af atypical epithelial cells infiltrating the stroma (H and E, ×40) |
What Is Your Diagnosis?
Answer
The diagnosis was an invasive squamous cell carcinoma of the nail bed with a moderate cellular differentiation (G2) and 2 mm of Breslow thickness.
Discussion
Squamous cell carcinoma is the most frequent malignant tumor of the nail unit.[1] It most commonly affects the fingernails, particularly the thumb and the index finger. It is also more common among men, in their sixties.[2] Two predisposing factors are mainly associated with the development of squamous cell carcinoma of the nail unit: (1) A reduction in the local immunity and (2) human papilloma virus infection.[3] In our sample real time polymerase chain reaction investigation revealed the presence of human papillomavirus-16.
The tumor usually has a prolonged course, with slow growth and late invasion. In addition, nail bed squamous cell carcinomas do not usually affect the nail matrix, allowing a normal growth of the nail plate which covers the tumor in the early stages. Invasive squamous cell carcinoma has a greater tendency to invade the underlying bone.
Nail bed squamous cell carcinoma is a great simulator in its initial clinical presentation. In its early stages, squamous cell carcinoma may present with nonspecific clinical signs characterized by subungual and periungual hyperkeratosis, oozing from the nail bed and longitudinal leukonychia, melanonychia or erythronychia.[4]
Nail plate detachment, induced by the tumor mass in the nail bed, could predispose to the development of superinfections and mislead the clinician to a wrong diagnosis such as onychomycosis.[1] Superinfections may also induce pain sensation, frequently reported by the patients with subungual squamous cell carcinoma. A misdiagnosis of human papillomavirus induced wart could also be made, but the repeated nonresponsiveness to medical therapy, such as salicylic acid, or physical therapy such as cryotherapy, should arouse suspicion.[4] Subungual keratoacanthoma and Bowen disease are also other rare entities affecting the nail bed. Nodular amelanotic melanoma usually destroys the nail plate in the initial stages itself, contrary to nail bed squamous cell carcinoma. On the other hand, pyogenic granuloma is often localized at the nail fold with associated ingrowing nail. Finally, X-ray examination could be used to differentiate nail bed squamous cell carcinoma from exostosis.[4]
Dermoscopic findings of subungual squamous cell carcinoma aren't specific or standardized and there is a lack of large-scale studies in the literature. For this reason, biopsy examination, as in our case, is mandatory for establishing the diagnosis.
In our patient, the involvement of a single finger by a long-standing bleeding erosion under the nail plate was considered suggestive of a nail tumor. Removal of the detached nail plate allowed the visualization of the ulcerated nodule.
Mohs surgery was performed for obtaining the clearance of the neoplasm, following three steps. In the first two steps, the tumor specimens were excised following an accurate diagram in the context of the nail unit and were subsequently transported to the laboratory, where they were processed and examined [Figure - 2]b. In the third step, an initial periosteal invasion was treated with deep curettage, reaching the underlying bone. Finally, a skin substitute based on hyaluronic acid was applied on the nail bed wound to achieve healing by second intention. The use of Mohs surgery allowed the removal of only those parts of the nail bed invaded by the tumor, with a large part of the nail bed being preserved.
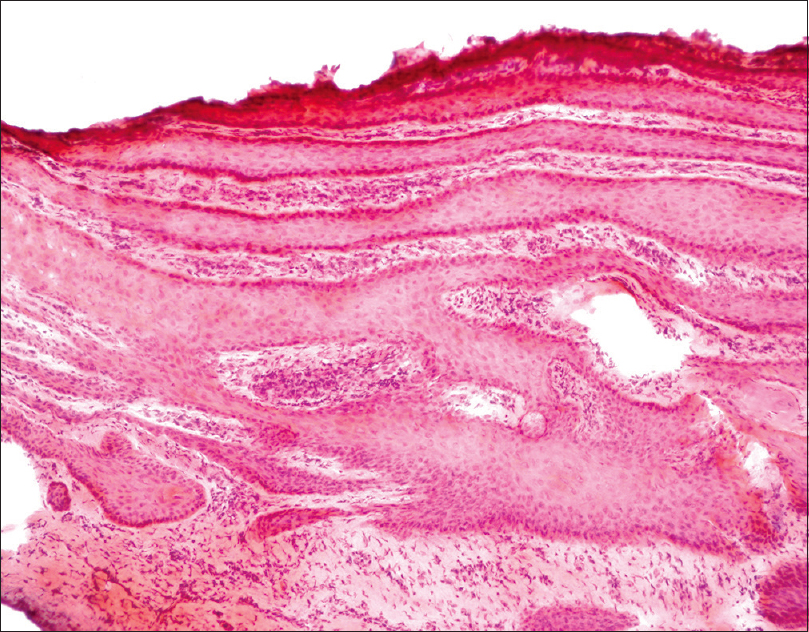 |
| Figure 2b: Mohs section of the tumor showing the persistence of neoplastic cells -Step 2( H and E, ×15) |
Mohs surgery is the elective treatment in squamous cell carcinoma, offering the highest cure and lowest disease recurrence rates.[4] Disarticulation of the distal phalanx is necessary when bone involvement is present and proved by a histopathologic or/and radiographic examination.[4] Photodynamic therapy, curettage with or without fluorouracil 5% or imiquimod 5% cream, electrochemotherapy with bleomycin and bleopuncture with imiquimod cream have also been reported as effective treatments, but recurrences are more frequent.[2]
Metastases and death from squamous cell carcinoma of the nail have been rarely reported with <10 cases worldwide.[5] Follow-up for at least 5 years is recommended, including clinical and instrumental investigations. After 3 years of follow-up, our patient has remained free of disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Dalle S, Depape L, Phan A, Balme B, Ronger-Savle S, Thomas L. Squamous cell carcinoma of the nail apparatus: Clinicopathological study of 35 cases. Br J Dermatol 2007;156:871-4.
[Google Scholar]
|
| 2. |
Lecerf P, Richert B, Theunis A, André J. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol 2013;69:253-61.
[Google Scholar]
|
| 3. |
The detection of human papillomavirus-16 in squamous cell carcinoma of the nail unit: A case series. J Am Acad Dermatol. 2017;76:354-356.
[Google Scholar]
|
| 4. |
Dika E, Piraccini BM, Balestri R, Vaccari S, Misciali C, Patrizi A, et al. Mohs surgery for squamous cell carcinoma of the nail: Report of 15 cases. Our experience and a long-term follow-up. Br J Dermatol 2012;167:1310-4.
[Google Scholar]
|
| 5. |
McHugh RW, Hazen P, Eliezri YD, Nuovo GJ. Metastatic periungual squamous cell carcinoma: Detection of human papillomavirus type 35 RNA in the digital tumor and axillary lymph node metastases. J Am Acad Dermatol 1996;34:1080-2.
[Google Scholar]
|
Fulltext Views
15,651
PDF downloads
3,268





