Translate this page into:
An asymptomatic erythematous plaque on the cheek
Corresponding author: Dr. Jing Xiao, Department of Dermatology, Wuhan No 1 Hospital, Wuhan, Hubei Province, People’s Republic of China. mickey9610@163.com
-
Received: ,
Accepted: ,
How to cite this article: Xiao J, Zhang L, Chen L. An asymptomatic erythematous plaque on the cheek. Indian J Dermatol Venereol Leprol 2023;89:606–8.
A woman in her 80s presented with an erythematous plaque on her left cheek of more than two years’ duration. The lesion was asymptomatic and slow-growing. Physical examination revealed an ill-demarcated, irregular erythematous plaque with slight scaling and crusting [Figure 1a]. Reflectance confocal microscopy image shows suspicious cells with dark cytoplasm and a mild bright nucleus; these cells were twice the size of normal keratinocytes or larger. A large number of cells merged into nests and formed dark glandular structures [Figure 1b]. Histopathologic examination revealed epidermal infiltration by large atypical cells that had eosinophilic cytoplasm and prominent nuclei [Figure 2a]. Immunohistochemically, the cells were strongly positive for cytokeratin stains cytokeratin 7 (CK7) and epithelial membrane antigen (EMA) [Figures 2b and 2c], but negative for CK20, S100 protein, human melanoma black 45 (HMB-45) and p63 (not shown).
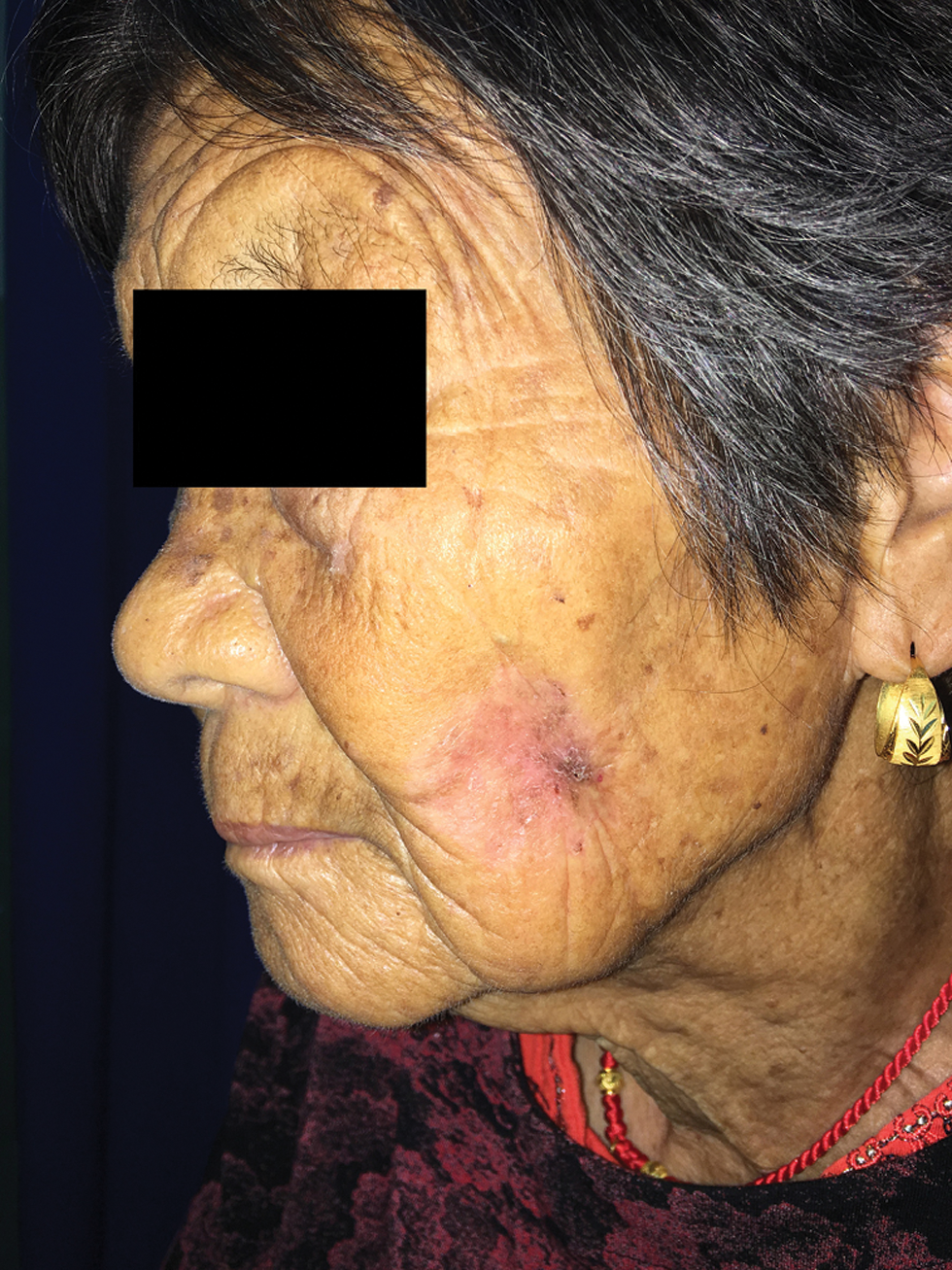
- An erythematous plaque on the cheek with ill-demarcated margins
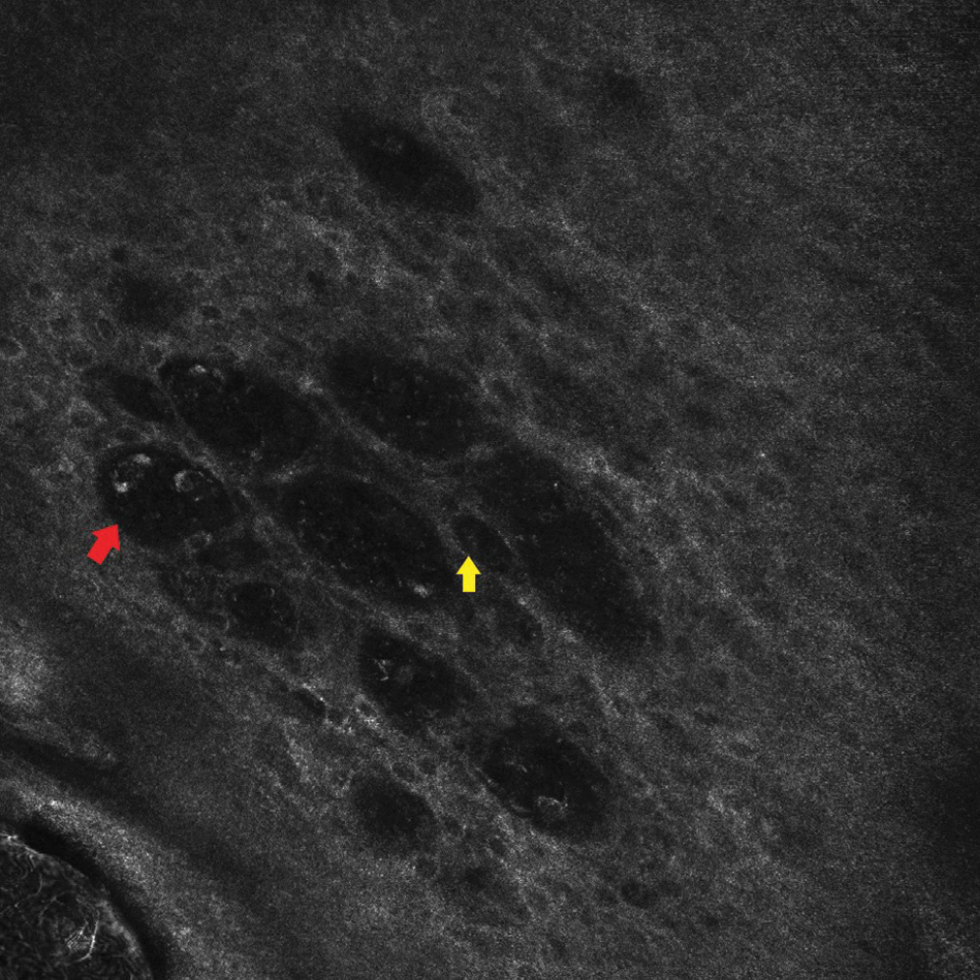
- Dark cytoplasm and mild bright nucleus (yellow arrows) and dark glandular nest structures in epidermal layer (red arrows) (750 ×750 μm)
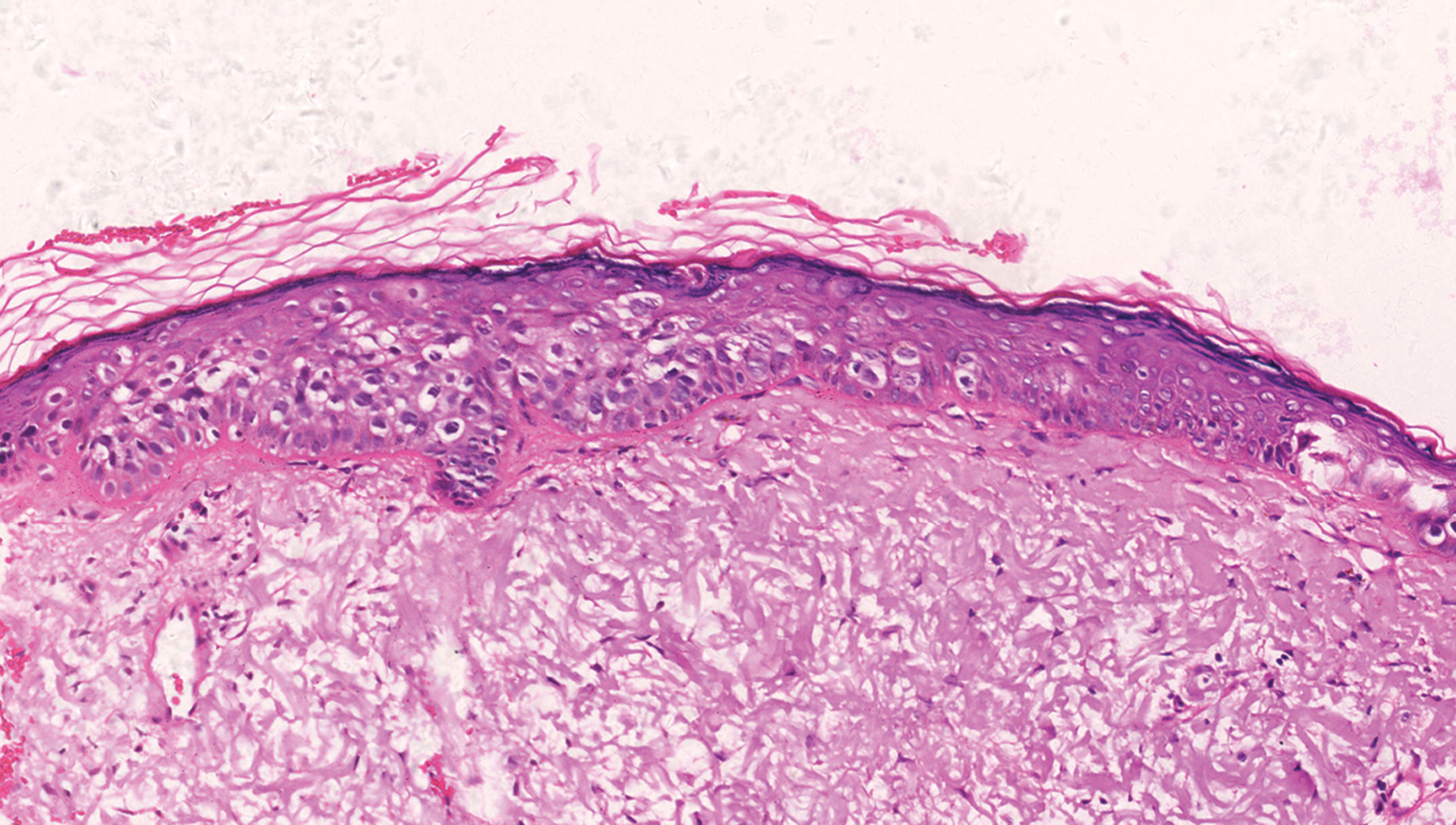
- Paget cells throughout epidermis (H&E, ×200)
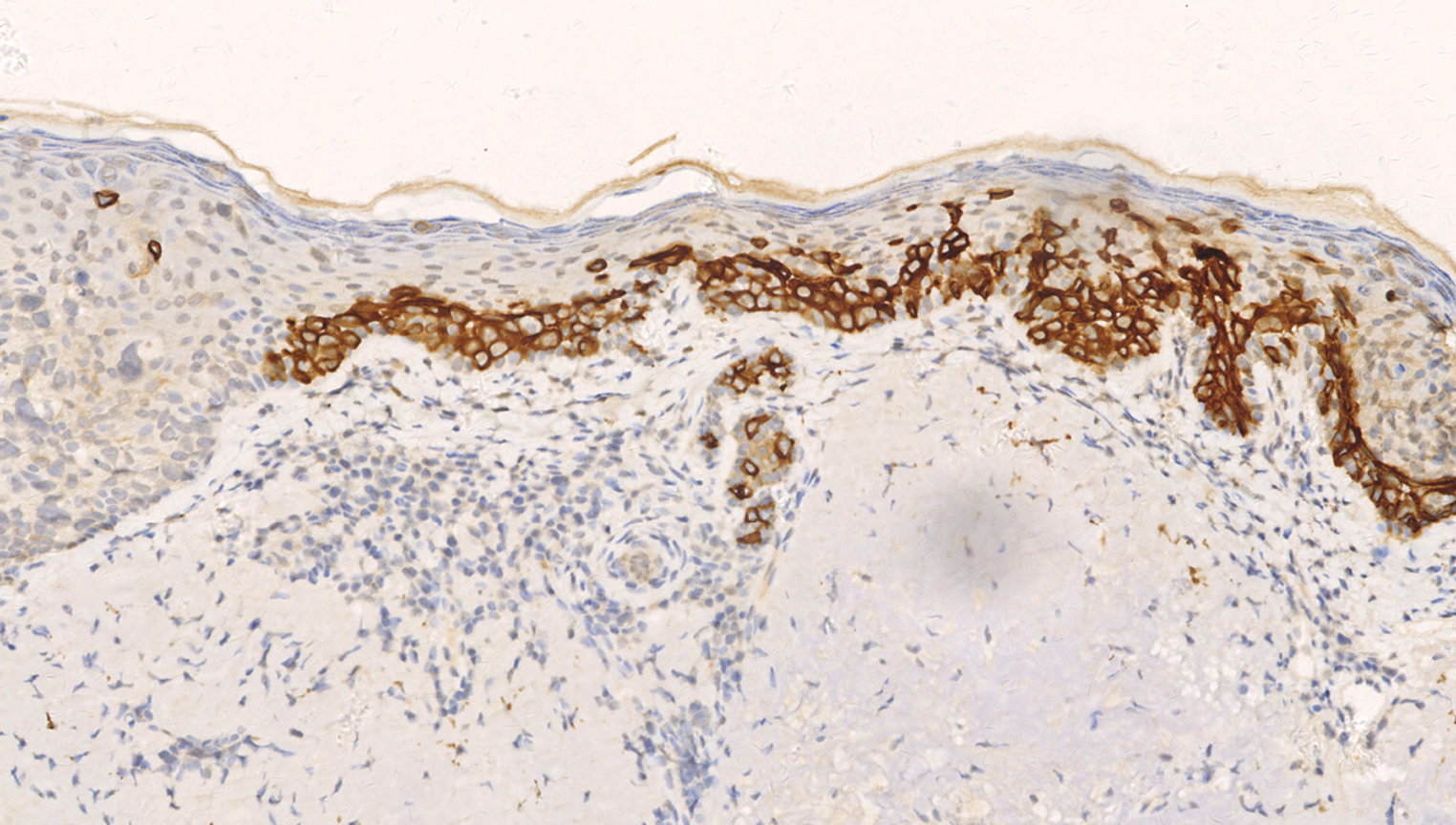
- The clear cells were positive for CK7 (Original magnification, ×200)
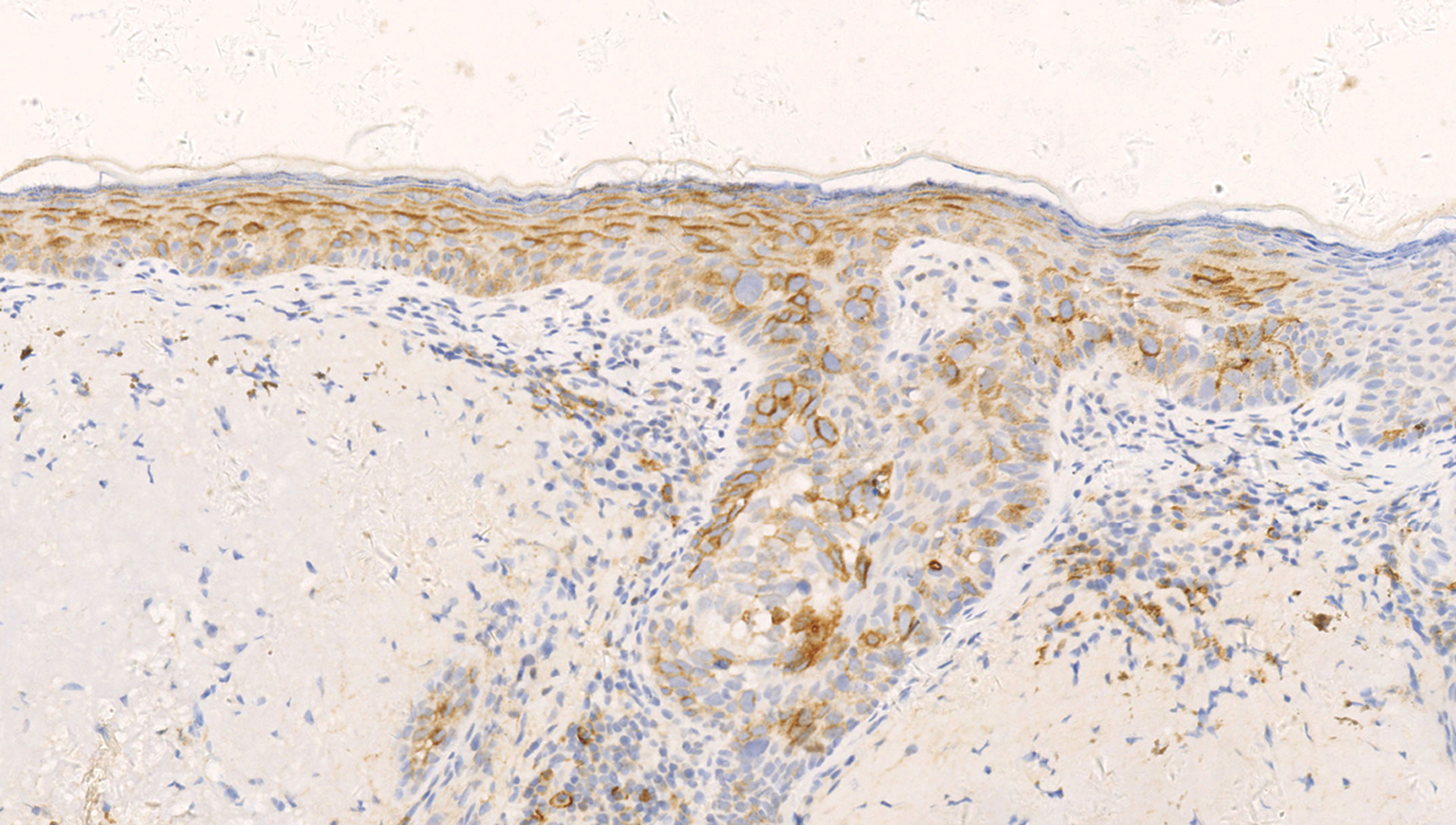
- Positive staining for epithelial membrane antigen (Original magnification, ×200)
What is Your Diagnosis?
Diagnosis
Ectopic extramammary Paget disease.
DISCUSSION
Extramammary Paget disease is a rare tumour that generally occurs in areas with a high density of apocrine glands.1 It presents with an erythematous spread in elderly patients, mainly in the anogenital region and in the axilla.1 In our study, we found that the disease occurred in apocrine-poor areas such as the cheek. Saida et al. proposed such cases to be called ectopic extramammary Paget disease, which are exceedingly rare, with more than 40 case reports on the buttock, back, chest, hypochondrium, abdomen, scalp and face, mostly in Asian patients (approximately 60%).2 The tumour location of ectopic extramammary Paget disease appears to be more common on the trunk.2 The risk of ectopic extramammary Paget disease-associated malignancy is not well known. There is only one case identified in the literature of association with underlying malignancy of adenocarcinoma of colon.3 Our patient did not reveal a concurrent malignancy.
Clinically and histologically, ectopic and “ordinary” extramammary Paget disease have similar manifestations except for the location of the disease,2 and in our study ectopic extramammary Paget disease also had a similar presentation on reflectance confocal microscopy. Researchers have proved the Paget cells present in reflectance confocal microscopy images, along with the characteristic nest structures at the dermo-epidermal junction, offer significant clues when it comes to identifying extramammary Paget disease.4 Reflectance confocal microscopy images of our patient correlating well with histopathology, contribute to the early diagnosis of extramammary Paget disease.
Immunohistochemistry has been used both to diagnose Paget disease and to differentiate it from other intraepidermal neoplasms with clear cells, such as pagetoid Bowen disease (CK7 negative/positive, EMA negative, p63 positive) and pagetoid melanoma (S100 positive, HMB-45 positive, CK7 negative).1 Especially for pagetoid Bowen’s disease, there are some in which it is difficult to make a definite histopathological differentiation from extramammary Paget disease; because there is considerable immunophenotypic overlap between pagetoid Bowen disease and extramammary Paget disease. CK7, especially, is an extremely sensitive marker of extramammary Paget disease, but occasional cases of pagetoid Bowen disease have been unexpectedly positive, limiting the value of this marker in this diagnostic scenario. In addition, there is a scarce report of pagetoid Bowen disease that expresses immunohistochemical markers of secretory cells like EMA. The presence of p63 in the neoplastic cells of pagetoid Bowen’s disease has been demonstrated, in contrast to its total absence in the Paget cells of extramammary Paget disease.1 The specific expression of p63 in pagetoid Bowen disease indicates that p63 constitutes a useful marker for its histopathological diagnosis.
Immunohistochemistry also helps to identify the likely cell of origin, as there are antigenic differences between primary intraepidermal Paget disease (CK7 positive, CK20 negative, gross cystic disease fluid protein (GCDFP-15) positive) and Paget disease that has spread from an associated internal carcinoma (CK7 positive, CK20 positive, GCDFP-15 negative).2
Surgical excision with wide margins and Mohs micrographic surgery remains the mainstay of treatment for extramammary Paget disease.1 In literature, there was only one case identified of lymph node metastasis in ectopic extramammary Paget disease.5 Our patient was treated with Mohs micrographic surgery and has been followed up for 5 years without recurrence, lymphadenopathy or metastasis. It seems that ectopic extramammary Paget disease appears to have a more benign biologic activity compared to “ordinary” extramammary Paget disease, and there is an associated malignancy in 20-30% of cases in “ordinary” extramammary Paget disease.2
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Mammary and extramammary Paget’s disease. J Eur Acad Dermatol Venereol. 2007;21:581-90.
- [CrossRef] [PubMed] [Google Scholar]
- Definition, association with malignancy, biologic behavior, and treatment of ectopic extramammary Paget’s disease: A review of the literature. J Clin Aesthet Dermatol. 2019;12:40-4.
- [PubMed] [Google Scholar]
- Pigmented extramammary Paget disease of the abdomen: A potential mimicker of melanoma. Dermatol Online J. 2011;17:13.
- [PubMed] [Google Scholar]
- In vivo reflectance confocal microscopy of extramammary Paget disease: Diagnostic evaluation and surgical management. J Am Acad Dermatol. 2012;66:e47-53.
- [CrossRef] [PubMed] [Google Scholar]





