Translate this page into:
An erythematous plaque on the leg of a female
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3 Department of Nuclear Medicine and PET, Postgraduate Institute of Medical Education and Research, Chandigarh, India
4 Department of Hematology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Sanjeev Handa
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh - 160 012
India
| How to cite this article: Bishnoi A, Handa S, Vishwajeet V, Saikia UN, Singh B, Mittal BR, Prakash G, Malhotra P. An erythematous plaque on the leg of a female. Indian J Dermatol Venereol Leprol 2019;85:666-673 |
A 43-year-old lady presented for evaluation of a gradually enlarging, mildly painful, non-pruritic, reddish raised scaly lesion of 5-months duration on her right leg. She was a known case of hypothyroidism on treatment and had accompanying high-grade fever and night sweats. She had no history of ulceration, local trauma, joint pains, weight loss, cough with expectoration, sore throat, oral/genital ulcers or photosensitivity. She was previously treated with oral and intravenous antibiotics and oral steroids for presumed cellulitis and erythema nodosum, respectively. Though she experienced transient improvement with corticosteroids, there was no improvement with antibiotics.
Inspection revealed an ill-defined, slightly depressed, annular erythematous plaque, approximately 18 × 16 cm in size, with minimal central hyperpigmentation and peripheral scaling on the medial aspect of the upper right leg [Figure - 1]a and b]. The plaque was warm, slightly tender and firm on palpation. Lymph nodes, liver and spleen were not enlarged. Clinical diagnoses of chronic erythema nodosum and cutaneous lymphoma were considered.
 |
| Figure 1: |
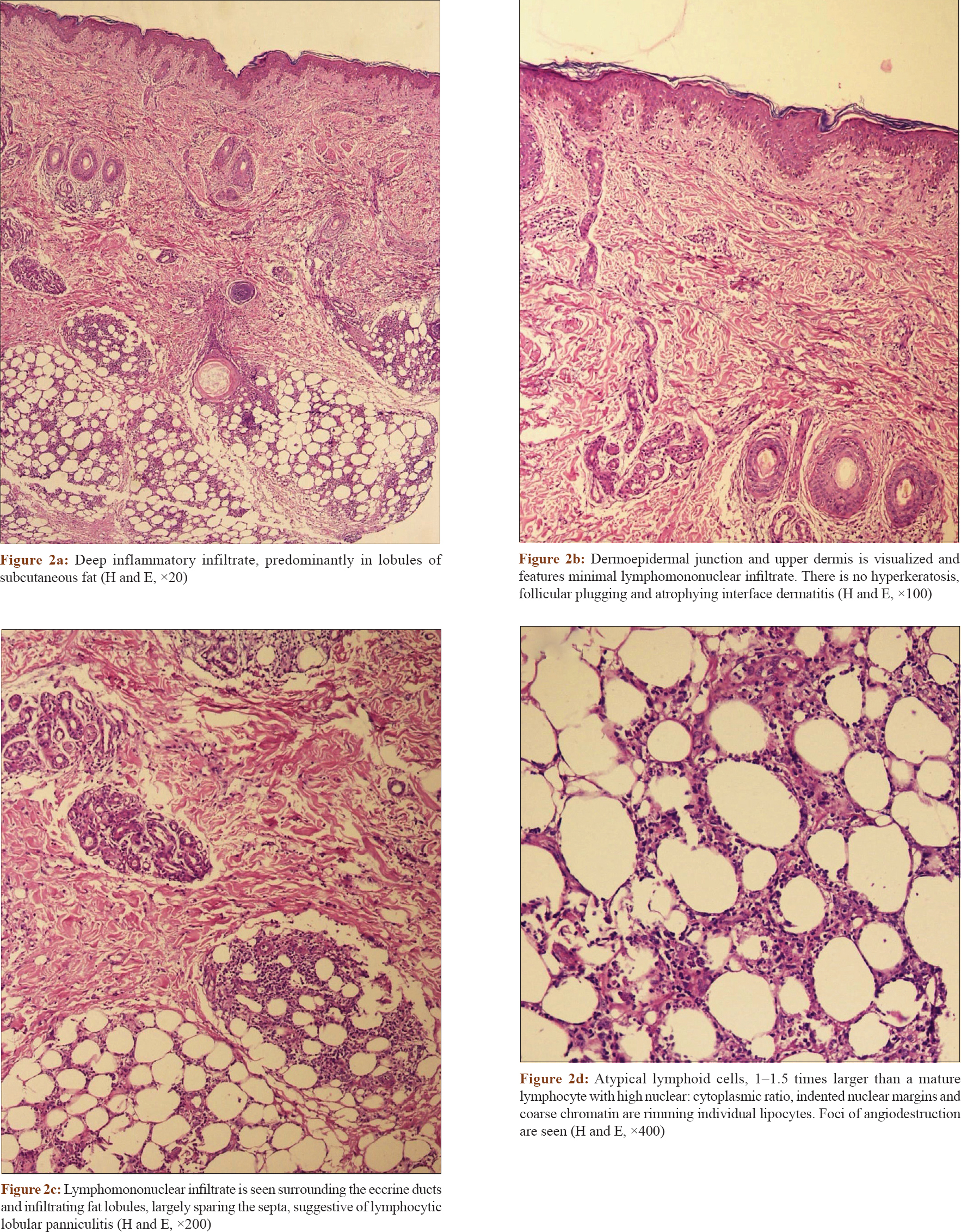
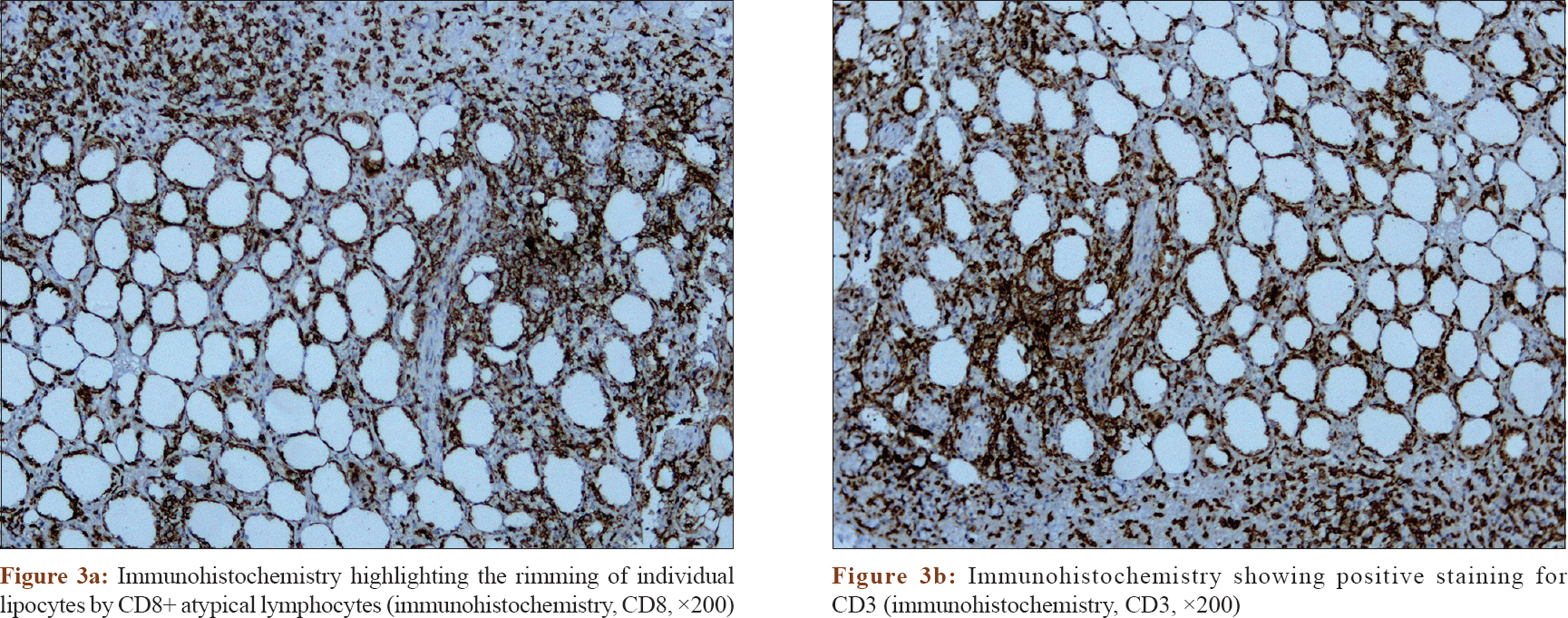
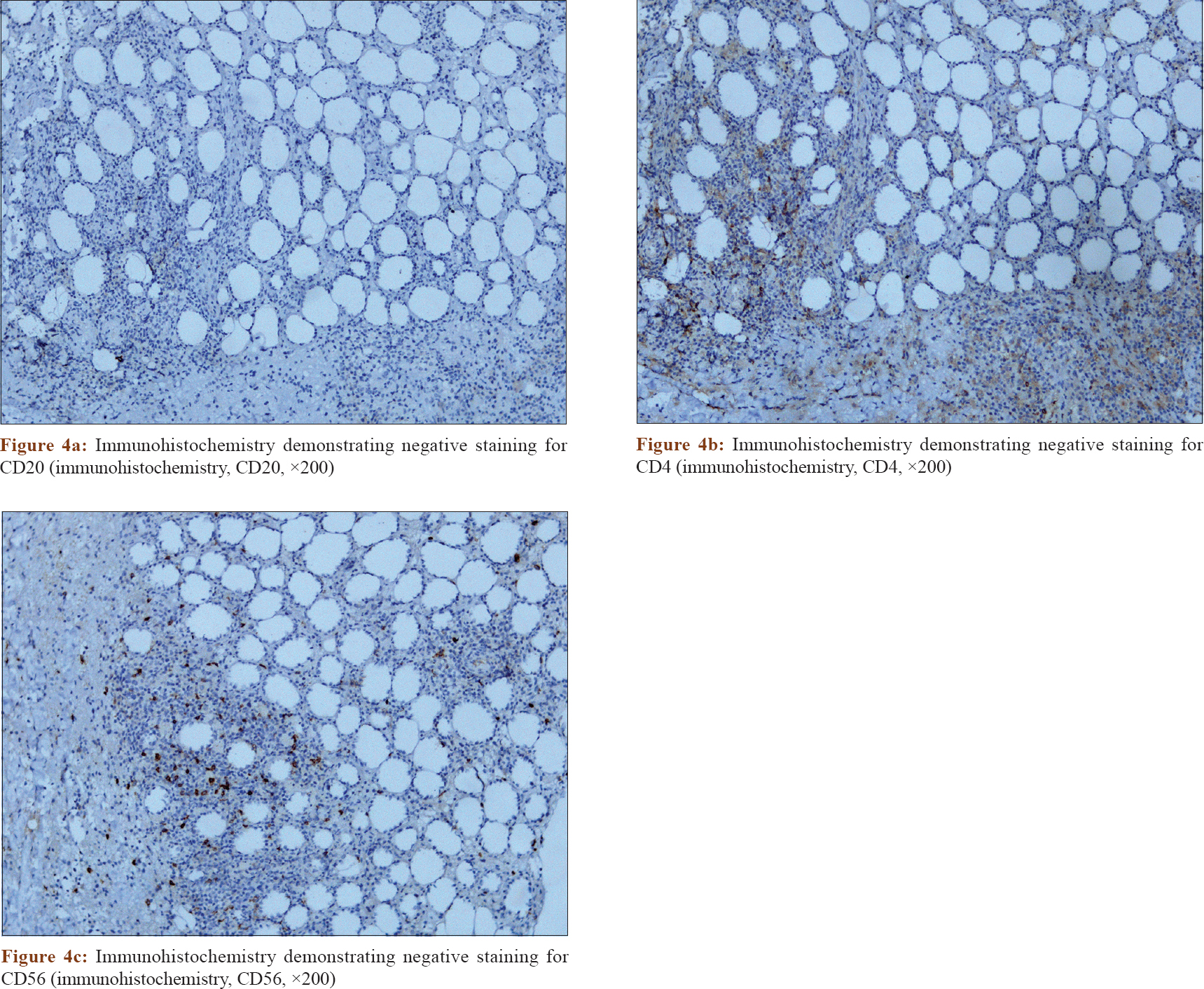
Total leucocyte count was 3300/cm [3]. Titers of antistreptolysin O antibodies, antinuclear antibodies (performed by indirect immunofluorescence) and anti-double-stranded DNA antibodies were not elevated. Mantoux test was negative. Blood and urine cultures were sterile. Chest X-ray was normal. Serum ferritin was 460 ng/ml. Histopathological examination and immunohistochemistry were performed on a deep incisional skin biopsy and findings are demonstrated [Figure - 2], [Figure - 3], [Figure - 4].
 |
| Figure 2: |
 |
| Figure 3: |
 |
| Figure 4: |
What Is Your Diagnosis?
Diagnosis
Subcutaneous panniculitis-like T-cell lymphoma.
Microscopic Findings
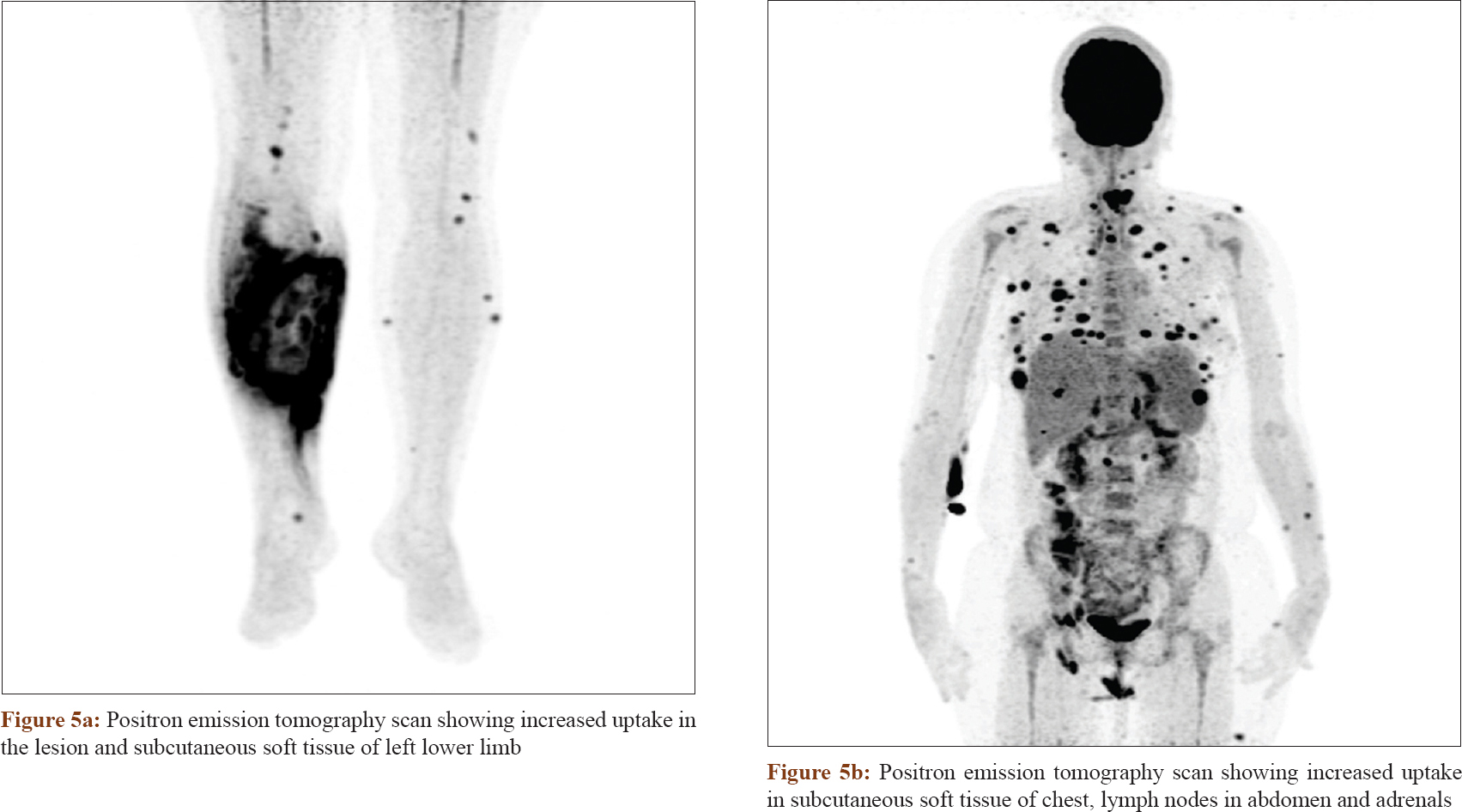
Histopathology demonstrated deep inflammatory infiltrate, predominantly in the subcutaneous fat [Figure - 2]a and [Figure - 2]b. On higher power, the infiltrate was chiefly composed of atypical lymphoid cells, which were 1–1.5 times larger than a mature lymphocyte with high nuclear: cytoplasmic ratio, indented nuclear margins and coarse chromatin [Figure - 2]c and [Figure - 2]d. There were scattered histiocytes and rare plasma cells. On immunohistochemistry, atypical lymphocytes were positive for CD3 and CD8 [Figure - 3]a and [Figure - 3]b and negative for CD20, CD4 and CD56 [Figure - 4]a, [Figure - 4]b, [Figure - 4]c. Immunohistochemistry highlighted the rimming of individual lipocytes by CD8+ atypical lymphocytes. Features were consistent with subcutaneous panniculitis like T-cell lymphoma (alpha beta type). She was started on prednisolone 60 mg/day. Meanwhile, positron emission tomography scan revealed multiple avid uptakes in the subcutaneous soft tissue (lesion, left leg, neck and chest), abdominal and pelvic lymph nodes and adrenals [Figure - 5]a and [Figure - 5]b. By the time of completion of staging investigations, the patient had developed multiple new erythematous plaques and skin-colored nodules on her neck and upper chest [Figure - 1]c and [Figure - 1]d.
 |
| Figure 5: |
She was subsequently administered cyclophosphamide, hydroxydaunorubicin, vincristine and prednisolone chemotherapy regimen. She attained partial remission after 8 cycles of chemotherapy. Subsequently, she was given local-site radiotherapy, after which she attained complete remission. The plaque resolved leaving behind lipoatrophy [Figure - 6]. She is following regularly with us.
 |
| Figure 6: Plaque has regressed leaving behind lipoatrophy |
Discussion
Subcutaneous panniculitis like T-cell lymphoma accounts for less than 1% of all non-Hodgkin's lymphomas.[1] Patients often present with subcutaneous nodules and plaques on extremities and trunk, which usually resolve with lipoatrophy. Systemic symptoms and cytopenias are common. Hemophagolymphohistiocytosis develops in approximately 15–20% of the patients.[2] Bone marrow biopsy was performed and our patient did not have evidence of hemophagolymphohistiocytosis or malignant infiltration of bone marrow.
Histologically, atypical lymphocytes with irregular hyperchromatic nuclei infiltrate fat lobules causing lobular panniculitis with relative sparing of dermis and epidermis. Rimming of individual lipocytes by these atypical cells is characteristic, though not specific, for subcutaneous panniculitis-like T-cell lymphoma.[3] Repeated skin biopsies are often required before a definitive diagnosis is made, and a sincere effort should be made to include ample subcutaneous fat while procuring skin biopsy. The index patient had to be biopsied twice before a diagnosis of subcutaneous panniculitis-like T-cell lymphoma was made. Reactive histiocytes are frequently seen but are usually present singly and do not form granulomas.[4] Erythrophagocytosis by histiocytes has been ascribed as a defining feature of subcutaneous panniculitis-like T-cell lymphoma.[4]
T-cell lymphomas causing panniculitis can have alpha-beta or gamma-delta T-cell-receptor phenotype. Subcutaneous panniculitis-like T-cell lymphoma shows alpha-beta phenotype with simultaneous expression of CD3, CD8 and betaF1. Expression of CD56 is usually absent. Presence of CD56 and gamma-delta T-cell phenotype and absence of CD8 is seen in primary cutaneous gamma-delta T-cell lymphoma involving subcutis, which has a poor 5-year survival of just 20% compared to the classic subcutaneous panniculitis-like T-cell lymphoma, where it exceeds 80% in the absence of hemophagolymphohistiocytosis and is approximately 50% in the presence of hemophagolymphohistiocytosis.[1] Another entity that can manifest as panniculitis is extranodal natural killer-T cell lymphoma, which stains positively for Epstein–Barr virus.[5] Our patient showed positive beta F1, and negative Epstein–Barr virus and gamma T-cell receptor staining, confirming the diagnosis of subcutaneous panniculitis-like T-cell lymphoma.
Diffuse large B-cell lymphoma leg-type presents with erythematous-bluish nodules on the legs of elderly females. Immunohistochemistry helps to differentiate subcutaneous panniculitis-like T-cell lymphoma from diffuse large B-cell lymphoma leg-type, where infiltrate is dense dermal and composed of malignant centroblasts that stain positively with CD20 and Bcl2.
CD8+ lymphoproliferative disorders primarily involving the skin include subcutaneous panniculitis-like T-cell lymphoma, primary cutaneous aggressive epidermotropic cytotoxic T-cell lymphoma and type D lymphomatoid papulosis. Subcutaneous panniculitis-like T-cell lymphoma primarily involves panniculus, whereas the other two potentially cause epidermal invasion by CD8+ and CD30+ atypical lymphocytes respectively.[6]
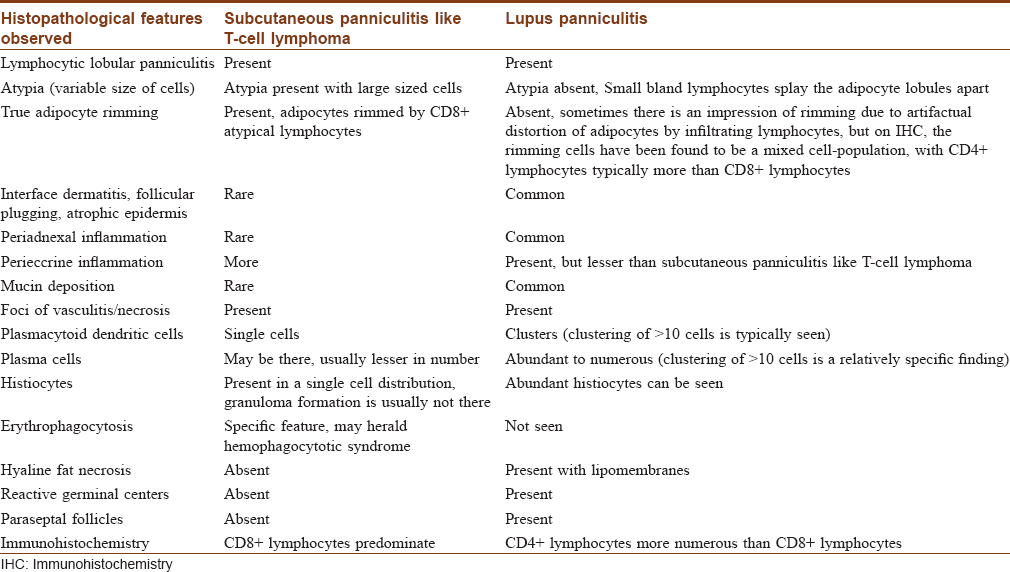
Lupus erythematosus panniculitis/lupus panniculitis is a potential histopathological mimicker of subcutaneous panniculitis like T-cell lymphoma. It usually involves face, breast and proximal extremities, though lesions have also been described on legs. Histopathology is characterized by presence of numerous plasma cells, eosinophilic hyaline fat necrosis and infiltration by small, bland lymphocytes forming lymphoid follicles with germinal centers consisting of CD20+ B lymphocytes.[7] Lymphocytic vasculitis and karyorrhexis can be seen in both subcutaneous panniculitis like T-cell lymphoma and lupus panniculitis. Perieccrine infiltrates could be seen in both, though more characteristically and commonly observed in subcutaneous panniculitis-like T-cell lymphoma.[4] Rarely, lupus panniculitis can focally simulate adipocyte rimming due to splaying of adipocyte lobules and resultant artifactual distortion, but immunohistochemistry demonstrates rimming cells to be of mixed population with CD4+ lymphocytes outnumbering CD8+ lymphocytes, which are the predominant cells in subcutaneous panniculitis-like T-cell lymphoma.[8] Magro et al. have described minimal epitheliotropism with mild basal vacuolopathy, a classical Grenz zone and subjacent heavy infiltrate in deeper dermis and panniculus in subcutaneous panniculitis-like T-cell lymphoma.[4] LeBlanc et al. proposed that the presence of plasma cells, interface dermatitis and mucin neither negates nor exemplifies either diagnosis, though absence of plasma cells supports a diagnosis of subcutaneous panniculitis-like T-cell lymphoma.[9] Bosisio et al. recently proposed that clusters of plasmacytoid dendritic cells, if identified, are specific for lupus panniculitis.[8]
Magro et al. highlighted few lupus panniculitis cases having similar immunohistological features as subcutaneous panniculitis like T-cell lymphoma and rightfully proposed the term “subcuticular T-cell lymphoid dyscrasia/indeterminate lymphocytic lobular panniculitis” to define the cases that have clinicopathological features suggestive of a phenomenon intermediate between a reactive polyclonal process classical of lupus panniculitis and a malignant process defining subcutaneous panniculitis-like T-cell lymphoma. Such patients should be closely followed up to see whether they develop overt lymphoma over time.[4] Subcutaneous panniculitis-like T-cell lymphoma has been associated with concomitant systemic lupus erythematosus in 20% of the cases.[10] Our patient did not have any evidence of systemic lupus erythematosus after thorough investigations. Dermal inflammation was minimal, and panniculus showed infiltration by malignant pleomorphic lymphocytes showing significant atypia and a conspicuous rimming of adipocytes, which on further characterization by immunohistochemistry, revealed these cells to be CD8+, CD3+ and CD4- as well as CD20- that strongly supports the diagnosis of subcutaneous panniculitis-like T-cell lymphoma. Magro et al. suggest that absence of hyperkeratosis, follicular plugging, atrophying interface dermatitis and presence of significant constitutional symptoms with lesion progression and nonresponse to hydroxychloroquine/corticosteroids, as seen in the index patient, favors the diagnosis of subcutaneous panniculitis-like T-cell lymphoma.[4] [Table - 1] further highlights the salient histopathological differences between subcutaneous panniculitis-like T-cell lymphoma and lupus panniculitis.
Treatment of subcutaneous panniculitis-like T-cell lymphoma consists of cyclophosphamide, hydroxydaunorubicin, vincristine and prednisolone chemotherapy regimen. Radiotherapy has been used in localized lesions. Cyclosporine has been used in refractory cases as well as the primary treatment option with good outcomes and exerts significant inhibitory effect on the cytokine storm and systemic symptoms associated with subcutaneous panniculitis-like T-cell lymphoma.[11] Extracutaneous dissemination is quite rare in subcutaneous panniculitis-like T-cell lymphoma. To conclude, we emphasize on performing deep incisional skin biopsy for any suspicious deep-seated leg plaques associated with systemic symptoms so that subcutaneous panniculitis-like T-cell lymphoma is not missed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Jansen PM, Cerroni L, Berti E, Santucci M, Assaf C, et al. Subcutaneous panniculitis-like T-cell lymphoma: Definition, classification, and prognostic factors: An EORTC Cutaneous Lymphoma Group Study of 83 cases. Blood 2008;111:838-45.
[Google Scholar]
|
| 2. |
Gonzalez CL, Medeiros LJ, Braziel RM, Jaffe ES. T-cell lymphoma involving subcutaneous tissue. A clinicopathologic entity commonly associated with hemophagocytic syndrome. Am J Surg Pathol 1991;15:17-27.
[Google Scholar]
|
| 3. |
Salhany KE, Macon WR, Choi JK, Elenitsas R, Lessin SR, Felgar RE, et al. Subcutaneous panniculitis-like T-cell lymphoma: Clinicopathologic, immunophenotypic, and genotypic analysis of alpha/beta and gamma/delta subtypes. Am J Surg Pathol 1998;22:881-93.
[Google Scholar]
|
| 4. |
Magro CM, Crowson AN, Kovatich AJ, Burns F. Lupus profundus, indeterminate lymphocytic lobular panniculitis and subcutaneous T-cell lymphoma: A spectrum of subcuticular T-cell lymphoid dyscrasia. J Cutan Pathol 2001;28:235-47.
[Google Scholar]
|
| 5. |
Gallardo F, Pujol RM. Subcutaneous panniculitic-like T-cell lymphoma and other primary cutaneous lymphomas with prominent subcutaneous tissue involvement. Dermatol Clin 2008;26:529-40, viii.
[Google Scholar]
|
| 6. |
Davick JJ, Mutgi KAJ, Wanat KA, Link BK, Liu V. Disseminated CD8-positive, CD30-positive cutaneous lymphoproliferative eruption with overlapping features of mycosis fungoides and primary cutaneous anaplastic large cell lymphoma following remote solitary lesional presentation. J Cutan Pathol 2017;44:703-12.
[Google Scholar]
|
| 7. |
Fraga J, García-Díez A. Lupus erythematosus panniculitis. Dermatol Clin 2008;26:453-63, vi.
[Google Scholar]
|
| 8. |
Bosisio F, Boi S, Caputo V, Chiarelli C, Oliver F, Ricci R, et al. Lobular panniculitic infiltrates with overlapping histopathologic features of lupus panniculitis (lupus profundus) and subcutaneous T-cell lymphoma: A conceptual and practical dilemma. Am J Surg Pathol 2015;39:206-11.
[Google Scholar]
|
| 9. |
LeBlanc RE, Tavallaee M, Kim YH, Kim J. Useful parameters for distinguishing subcutaneous panniculitis-like T-cell lymphoma from lupus erythematosus panniculitis. Am J Surg Pathol 2016;40:745-54.
[Google Scholar]
|
| 10. |
Shiau CJ, Abi Daoud MS, Wong SM, Crawford RI. Lymphocytic panniculitis: An algorithmic approach to lymphocytes in subcutaneous tissue. J Clin Pathol 2015;68:954-62.
[Google Scholar]
|
| 11. |
Iqbal N, Raina V. Successful treatment of disseminated subcutaneous panniculitis-like T-cell lymphoma with single agent oral cyclosporine as a first line therapy. Case Rep Dermatol Med 2014;2014:201836.
[Google Scholar]
|
Fulltext Views
4,633
PDF downloads
2,929





