Translate this page into:
An exophytic friable plaque on a verrucous epidermal naevus
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Ahuja R, Najeeb A, Agarwal S, Khandpur S. An exophytic friable plaque on a verrucous epidermal naevus. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_942_2024
Dear Editor,
A 27-year-old woman presented with multiple non-itchy hyperpigmented and hyperkeratotic plaques extending from the chest to the lower limb in a Blaschko-linear arrangement on the left side of her body with some extension to the right side since early childhood. Over the past three years, she developed erythematous, exuberant, verrucous, and friable outgrowths with foul-smelling serous discharge and overlying crusting on these lesions, predominantly on the left lower limb, calf region [Figures 1a and 1b]. On oral examination, well-defined white plaques were observed on both the upper and lower gingivae. She also exhibited flexion deformities of the left hip and knee joints, along with scoliosis of the spine. A chest X-ray revealed cardiomegaly although the patient remained asymptomatic. There were no neurological or ophthalmological issues and no family history of similar illnesses. There was no history of loss of weight or any other general symptoms. Biopsies were taken from both the hyperkeratotic, hyperpigmented lesion and the overlying friable plaque.

- Unilateral involvement of the left side in the form of multiple hyperpigmented and hyperkeratotic plaques in a blaschkolinear pattern.

- Erythematous, exophytic, oozy, and friable growth on the left leg, overlying the hyperpigmented linear plaque.
Histological evaluation of the hyperkeratotic hyperpigmented lesion on the back showed signs of papillomatosis, parakeratosis, and mild acanthosis which is consistent with a diagnosis of verrucous epidermal naevus. Additionally, a biopsy of the erythematous friable discharging lesions on the lower limb showed neutrophils in the stratum corneum along with hyperkeratosis, parakeratosis, papillomatosis and irregular acanthosis of the epidermis [Figure 2a]. The papillary dermis exhibited abundant foamy histiocytes mixed with plasma cells. Overall, these histological features were suggestive of verruciform xanthoma [Figures 2b and 2c]. Furthermore, a biopsy from the lower gingiva also indicated verruciform xanthoma.
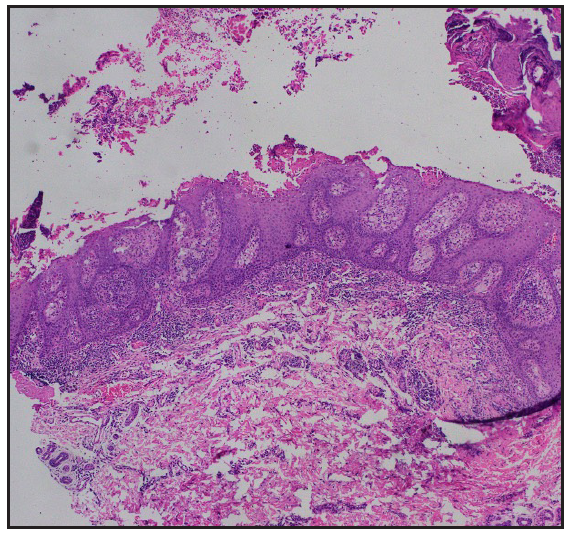
- Biopsy from the erythematous friable growth on the left leg showed neutrophils with fibrin in the stratum corneum, along with hyperkeratosis, parakeratosis, papillomatosis and irregular acanthosis of the epidermis (Haematoxylin and eosin, 40x).
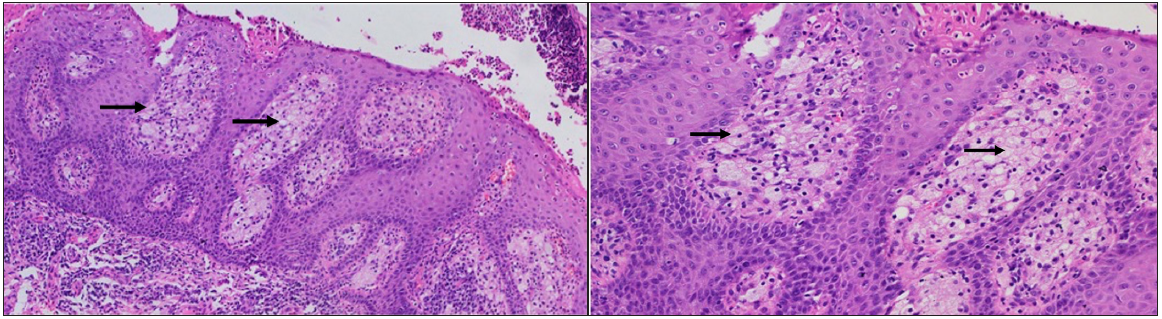
- On higher magnification, foamy histiocytes (black arrows) are appreciated in the dermal papillae (Haematoxylin and eosin, 2b- 100x and 2c-200x).
Verruciform xanthomas appear as papillomatous or cauliflower-like growths, usually in the oral mucosa, and are often misdiagnosed as papillomas.1 They can also affect the genital mucosa, where they are referred to as Verruciform Genital-Associated (VEGAS) xanthomas and may resemble condyloma acuminata, bowenoid papulosis, and giant molluscum contagiosum.2 Extraoral and extragenital involvement is infrequently reported on the skin and has been associated with lymphedema, epidermolysis bullosa, pemphigus, discoid lupus erythematosus, graft-versus-host disease, epidermal naevi and congenital haemidysplasia with ichthyosiform erythroderma and limb defects syndrome.1
In our case, we observed a segmental verruciform xanthoma along with a verrucous epidermal naevus. The patient also had scoliosis and cardiomegaly. Syndromic epidermal naevi can exhibit associations with neurological, ophthalmological, skeletal, and endocrinological abnormalities. While epidermal naevi with verruciform xanthomas are typically associated with CHILD syndrome, our case did not show the characteristic linear ichthyosiform lesions and haemidysplasia of this syndrome.3
Extramucosal verruciform xanthoma overlying non-syndromic inflammatory linear verrucous epidermal naevus (ILVEN/VEN) has been reported in a few previous case studies. In these reports, the lower limbs were the most commonly affected sites, followed by the trunk.4 The morphology of the lesions described ranged from skin-coloured to erythematous to yellowish verrucous exophytic growths. In contrast, the lesions in our patient appeared friable, with foul-smelling exudation, resembling squamous cell carcinoma or syringocystadenoma papilliferum (SCAP) arising in a naevus sebaceous. Both of these conditions are known to develop on existing verrucous epidermal naevi.5,6 While malignant transformation is rare, neoplasms such as basal cell carcinoma, squamous cell carcinoma, malignant eccrine poroma, and keratoacanthoma have been reported to occur on a verrucous epidermal naevus.7 However, histopathological examination helped us in diagnosing verruciform xanthomas.
The characteristic histological features include an acanthotic epidermis with parakeratosis that extends deeply into the epithelium, uniformly elongated rete ridges, a neutrophilic infiltrate in the dermis, and foamy histiocytes dispersed throughout the dermal papillae. The foam cells stain positively for Periodic Acid Schiff and express the CD68 antigen, indicating the presence of glycogen granules in monocyte-macrophage lineage cells.1
The precise pathogenesis remains unclear. It is hypothesised that a cutaneous reaction triggered by local trauma, irritation, or chronic inflammation may have resulted in epithelial degeneration and a subsequent local inflammatory response within the epithelium, characterised by the presence of neutrophils. The series of events lead to the release of lipids from degenerated keratinocytes which are subsequently scavenged by recruited macrophages, thereby presenting as foamy cells in the dermal papillae.1
The treatment usually involves wide surgical excision with no documented recurrences noted during a follow-up of six months.8 Dermatologists should keep in mind this rare association between verruciform xanthoma and verrucous epidermal naevus, as the xanthoma may sometimes exhibit a friable and exudative appearance and may resemble a carcinoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Verruciform xanthoma: A view on the concepts of its etiopathogenesis. J Oral Maxillofac Pathol. 2013;17:392-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vegas (verruciform genital-associated) xanthoma: A comprehensive literature review. Dermatol Ther (Heidelb). 2017;7:65-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Congenital hemidysplasia with ichthyosiform naevus and limb defects (CHILD) syndrome without hemidysplasia. Br J Dermatol. 2015;173:304-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Linear verruciform xanthoma of lower limb. Indian Dermatol Online J. 2023;14:876-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Squamous cell carcinoma arising in a multiple verrucous epidermal nevus. An Bras Dermatol. 2016;91:166-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Syringocystadenoma papilliferum and eccrine poroma arising in verrucous epidermal nevus: A case report and multidimensional skin imaging evaluation. Dermatol Pract Concept. 2022;12:e2022087.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Squamous cell carcinoma arising in a multiple verrucous epidermal nevus. An Bras Dermatol. 2016;91:166-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Verruciform xanthoma overlying inflammatory linear verrucous epidermal nevus and in broad segmental distribution. BMJ Case Rep. 2018;2018:bcr2018225964.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





