Translate this page into:
An intriguing case of persistent facial swelling
Corresponding author: Dr. Hua-Liang Joel Lim, National Skin Centre, Singapore. joellimhl@nsc.com.sg
-
Received: ,
Accepted: ,
How to cite this article: Chan SY, Tan CH, Tee SI, Lim HL. An instructive case of persistent facial swelling. Indian J Dermatol Venereol Leprol 2022;88:566-8.
A 69-year-old Malay man was admitted for persistent and slowly progressive facial swelling of 4 months duration, without any other constitutional symptoms. Clinical examination showed prominent, non-pitting edema involving the face, including peri-orbital areas [Figure 1a] and ear lobes [Figure 1b], giving a peau d’orange appearance [Figure 1b]. Closer examination also revealed barely perceptible non-blanchable erythema on the glabellum, nose and cheeks [Figure 1a]. A punch biopsy from the infiltrated plaque on the left cheek was obtained and sent for histopathological examination [Figures 2a-d].
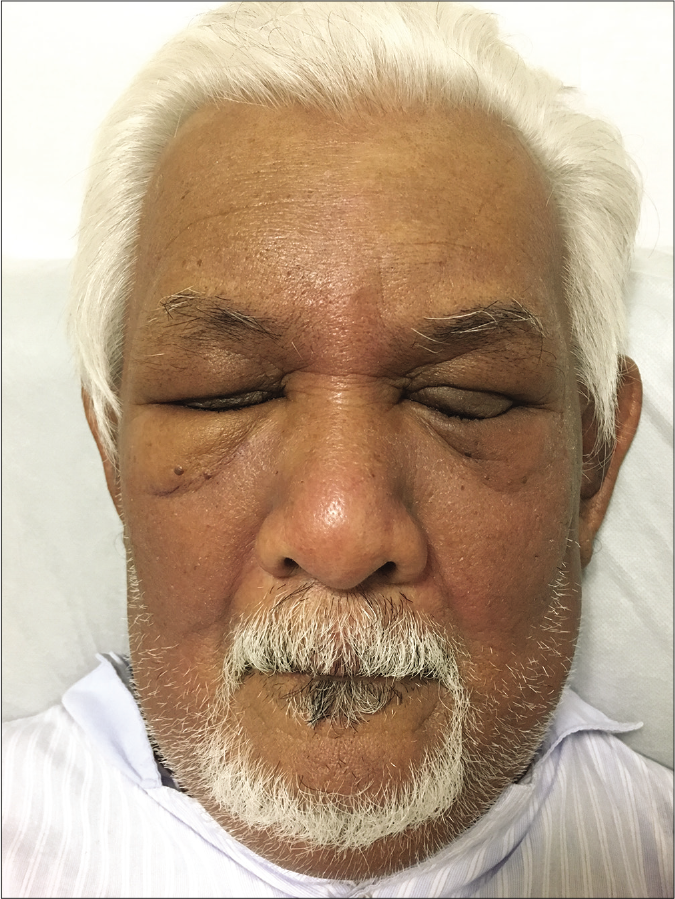
- Generalized symmetrical swelling affected periorbital region, nose and cheeks, and barely perceptible violaceous erythematous patches on the glabella and nose
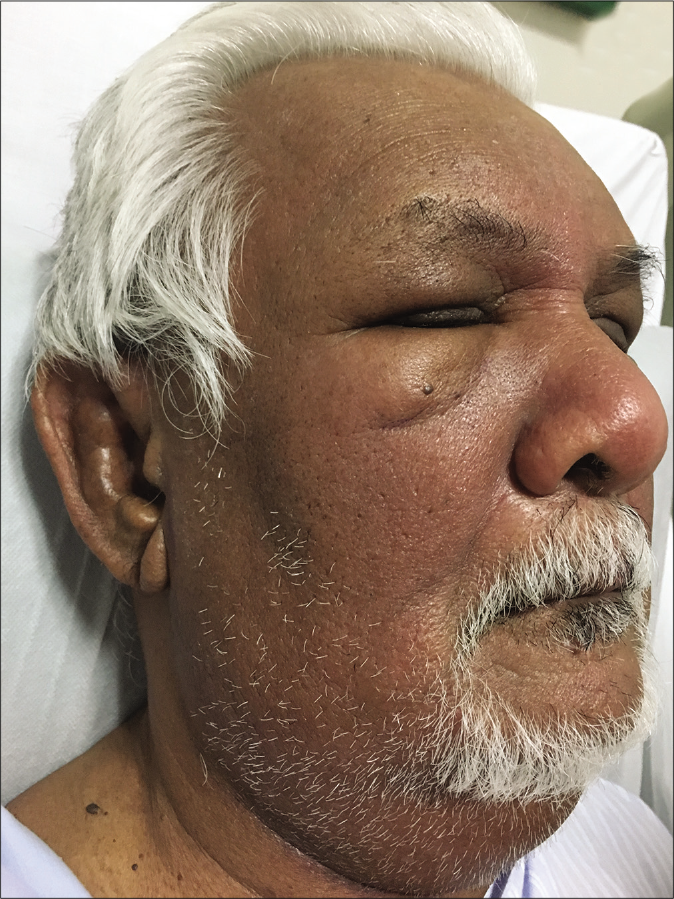
- Oedematous swelling of the auricle of the right ear, and peau d’orange appearance on the right cheek
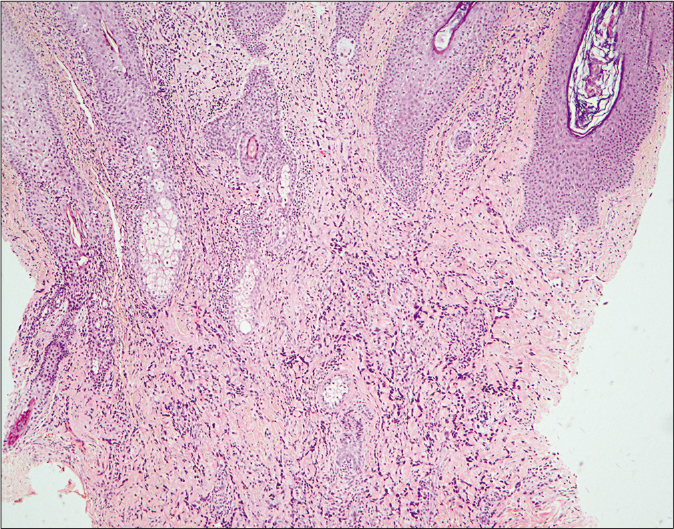
- Histopathological examination of a skin biopsy specimen taken from the left cheek. The dermis is extensively infiltrated by spindle cell proliferation, extending deeply and surrounding adnexal structures (H and E, ×40)
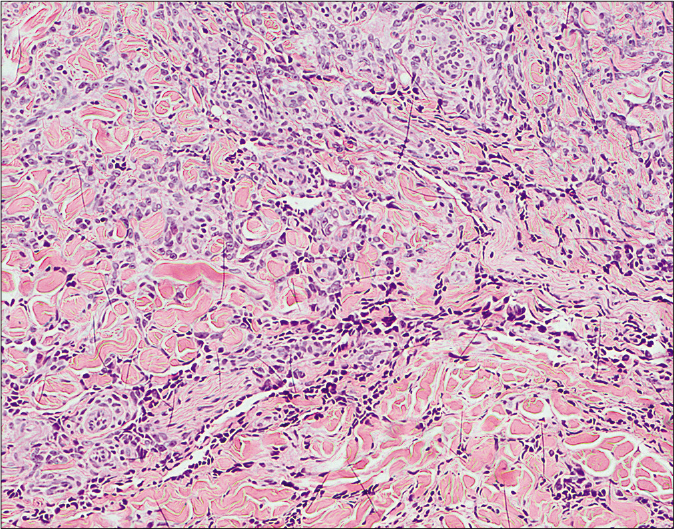
- Histopathological examination of a skin biopsy specimen taken from the left cheek. Spindle cells contain pleomorphic and hyperchromatic nuclei. They enclose numerous irregular slit-like vessels that dissect between collagen bundles (H and E, ×100)
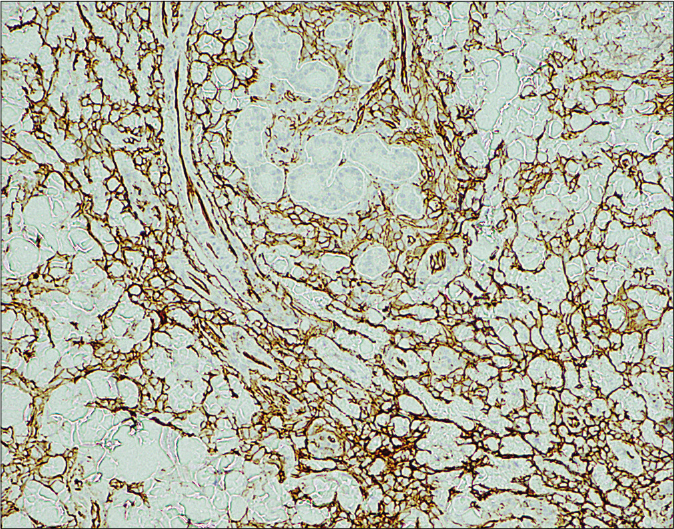
- Histopathological examination of a skin biopsy specimen taken from the left cheek. Neoplastic cells are positive for CD31 (×100)
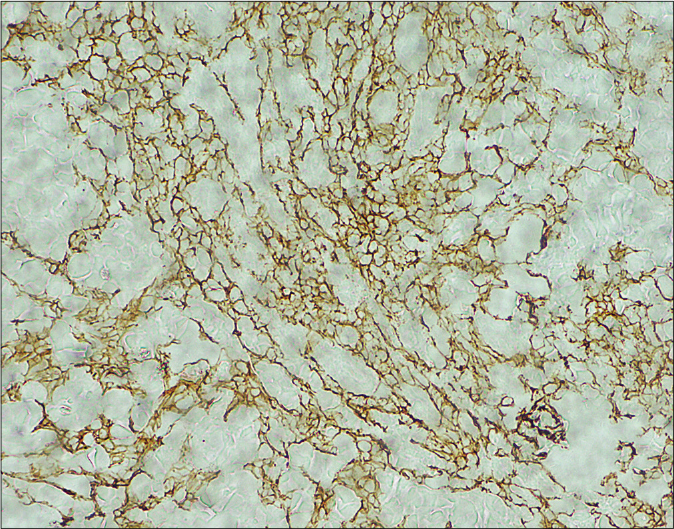
- Histopathological examination of a skin biopsy specimen taken from the left cheek. Neoplastic cells are positive for podoplanin (×100)
What is the diagnosis?
Diagnosis
Cutaneous angiosarcoma
Discussion
Histopathological examination showed a diffuse proliferation of spindle cells with pleomorphic, hyperchromatic nuclei infiltrating into the deep dermis. Cells demonstrated mild cytological atypia, showing pleomorphic, hyperchromatic nuclei as well as occasional abnormal mitotic figures (1–2 per 10 high-power fields). Numerous small, slit-like vessels were present, many noted to dissect between collagen bundles [Figures 2a and b]. The spindle cells were strongly positive for CD31 [Figure 2c], CD34 and podoplanin [Figure 2d]. Tissue necrosis was absent. Immunohistochemical stain for human herpes virus-8 came out negative. Computed tomography scan with contrast of the head, neck, thorax, abdomen and pelvis revealed extensive disease involvement of the scalp, face, neck and left sternocleidomastoid muscle, upper chest and multiple cervical lymph nodes with no evidence of pulmonary or liver metastases. He was not deemed suitable for surgery or radiotherapy in view of extensive disease, and was instead treated with monthly paclitaxel. Repeat imaging after 3 cycles of chemotherapy showed improvement with reduction in lesion thickness over the the scalp, face and neck.
Angiosarcoma is an aggressive malignancy of vascular endothelial cells, accounting for <2% of soft tissue sarcomas.1 The skin is the most common primary site with a predilection for the head and neck region.1 Cutaneous angiosarcoma may arise de novo, over previous sites of ionizing radiation or in association with chronic lymphedema.1,2 The clinical presentations are variable, ranging from subtle purpuric patches to diffuse purpuric plaques with ulceration.1
This case of extensive cutaneous angiosarcoma is remarkable for its unusual presentation as a persistent, non-pitting oedematous facial swelling. This appears to be a rare phenomenon with only few reports describing similar presentations such as generalized facial edema,2 unilateral facial or orbital oedema.3 Typical lesions of cutaneous angiosarcoma are erythematous to violaceous macules, patches, nodules or plaques,4 which may be solitary or multiple. The diagnosis can be confounded in people with darker skin tones as the violaceous erythema may not be clinically apparent as illustrated in this case.
Given the potential for airway obstruction, superior vena cava obstruction should be excluded in acute fixed non-pitting edema of the head and neck. Owing to the presence of non-blanchable erythema, a vascular neoplasm such as angiosarcoma was considered. Other differential diagnoses include Morbihan disease, allergic contact dermatitis or photodermatoses such as chronic actinic dermatitis or dermatomyositis. Conditions causing episodic facial swelling such as angioedema, carcinoid syndrome or Ascher syndrome were effectively excluded given the persistent and progressive nature of our patient’s dermatosis.
Angiosarcoma has a very poor prognosis1, 5 especially at late stages, hence early diagnosis is crucial. Poor prognostic factors include age >70 years, tumor >5 centimetres, location of the tumor on the scalp and positive post-resection margins.1 Scalp location, nodular morphology and multiplicity of skin lesions also affect survival outcomes in Asians.5 The mainstay of treatment for cutaneous angiosarcoma is surgery with adjuvant radiotherapy.1 Chemotherapy with paclitaxel or targeted immunotherapy (pazopanib or bevacizumab) are available options for patients with an extensive disease.1
We hope to underscore the presentation of extensive cutaneous angiosarcoma as a fixed, solid, persistent non-pitting edema of the face. The presence of non-blanchable erythema is a helpful clue to prompt further workup, so as to minimize delay in the treatment of this devastating disease.
Declaration of Patient Consent
Taking consent from the patient was not possible as he had passed away during the publication process due to complication of chemotherapy used as part of the treatment for his extensive disease.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous angiosarcoma: update on biology and latest treatment. Curr Opin Oncol. 2018;30:107-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma presenting as recurrent angio-oedema of the face. Br J Dermatol. 2000;143:1346-8.
- [CrossRef] [PubMed] [Google Scholar]
- Worsening solid facial edema: An unusual case of angiosarcoma. JAAD Case Rep. 2018;4:794-6.
- [CrossRef] [PubMed] [Google Scholar]
- Angiosarcoma of the scalp and face associated with kasabach-meritt syndrome and disseminated intravascular coagulation. Indian J Dermatol Venereol Leprol. 2016;82:96-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological and survival analyses of primary cutaneous angiosarcoma in an Asian population: prognostic value of the clinical features of skin lesions. Int J Dermatol. 2020;59:582-9.
- [CrossRef] [PubMed] [Google Scholar]





