Translate this page into:
An observational study to describe dermoscopic features of sweat dermatitis and assess the treatment outcome
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, PGIMER, Sector-12, Chandigarh, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mustari A, Garg D, Thind A, Narayan RV, Parkhi M, Vinay K. An observational study to describe dermoscopic features of sweat dermatitis and assess the treatment outcome. Indian J Dermatol Venereol Leprol. 2024;90:226–9. doi: 10.25259/IJDVL_1119_2022
Dear Editor,
Sweat dermatitis was first described by Ramam et al.1 in 1998, as an irritant dermatitis caused due to excessive stagnant sweat produced due to high temperature and low humidity.2 Risk factors include tight clothing, friction, and synthetic clothing that do not absorb sweat.3 It is seen both over convex areas such as lateral back, chest, and abdomen as well as concave areas such as lower back, cubital fossa, axilla, inter and submammary area, neck, and midline groove of the back.4 Clinically, it presents as dry, fissured, crinkled, hyperpigmented plaques with well-defined borders.5
This was a single-center observational study of 10 patients with sweat dermatitis diagnosed at the tertiary care center in North India, from April 2022 to September 2022. The study was done in summer where the daytime temperature reaches up to 49°C due to the prevailing heat wave.6 The diagnosis of sweat dermatitis was made based on the acute onset pruritic papules and scaly plaques on the classical sites (back, axillae, and inframammary areas), preceding history of increased sweating and rapid response to treatment. Written informed consent was taken from all patients/guardians. Clinical (age, sex, occupation, duration, relationship with sweating, use of synthetic clothing, sites involved, and morphology) and dermoscopic data was collected from all the patients and histopathological evaluation was done on two patients. Patients were contacted through telephone to enquire regarding recurrence of the symptoms.
A total of 10 patients were enrolled in this study. The mean age of presentation was 26.4 ± 8 (range; 10–38) years with male–female ratio of four and mean duration of disease was 8.1 ± 9.4 (range; 2–20, median; 8.5) days. The mean follow-up period was 2.5 ± 1.5 (range; 0.3–5) months. Two patients had history of similar lesions on the same sites in the previous year in summer, which resolved in 2–3 weeks. Use of synthetic clothes was present in 2 (20%) patients. The most common site of involvement was back (9/10; 90%) and other sites were infra-axillary area (2/10; 20%), inframammary area (1/10; 10%) and forehead (1/10; 10%). Patients presented with multiple erythematous to skin-colored tiny pinhead-sized papules on background of erythema (active stage; Figures 1a and 1b) in 40% (4/10) and greyish-brown scaling on background of dry hyperpigmented skin (resolving stage; Figure 2a) in 60% (6/10) of the patients and mean duration of disease in these patients was 3.2 and 11.3 days, respectively (p = 0.002). Pruritus was present in all the patients (100%; 10/10). Nine (9/10; 90%) patients reported history of excessive sweating prior to the development of skin lesions [Table 1].

- Clinical presentation (active stage) - Erythematous pinhead-sized papules on a background of erythema over the midline of the back

- Clinical presentation (active stage) - Scaling on the background of erythema over forehead due to excessive sweat and occlusion due to the use of turban

- Dermoscopy image of the active stage showing multiple linear erosions with brownish crusting in a hexagonal pattern on the background of erythema. Prominent eccrine gland openings can also be appreciated

- Clinical presentation (active stage) - Complete improvement after 7 days of treatment.
| Age/Sex | Occupation/Factors contributing to increased sweating | Duration (days) | Sites/Symmetry | Past history | History of excessive sweating | Presentation | Improvement after 7 days |
|---|---|---|---|---|---|---|---|
| 25/M | Horticulturist | 2 | Back/Symmetrical | No | Yes | Active stage* | Complete |
| 30/M | Cycling | 3 | Back/Symmetrical | Yes | Yes | Active stage* | Complete |
| 35/M | Farmer | 4 | Back, forehead and infra-axillary area/Symmetrical except over forehead | Yes | Yes | Active stage* | Partial |
| 21/F | Student | 4 | Back/Symmetrical | No | No | Active stage* | Partial |
| 38/M | Physical exercise | 10 | Back/Symmetrical | No | Yes | Resolving stage# | Complete |
| 26/M | Driver | 9 | Back/Symmetrical | No | Yes | Resolving stage# | Complete |
| 10/M | Student/Physical activity | 20 | Back/Symmetrical | No | Yes | Resolving stage# | Complete |
| 26/F | Homemaker | 12 | Inframammary/Symmetrical | No | Yes | Resolving stage# | Complete |
| 32/M | Security guard | 8 | Back and infra-axillary area/Symmetrical | No | Yes | Resolving stage# | Complete |
| 21/M | Student | 9 | Back/Asymmetrical | No | Yes | Resolving stage# | Complete |

- Clinical presentation (resolving stage) showing greyish-brown scaling on midline over back (concave area) and medial scapular margins (convex area)
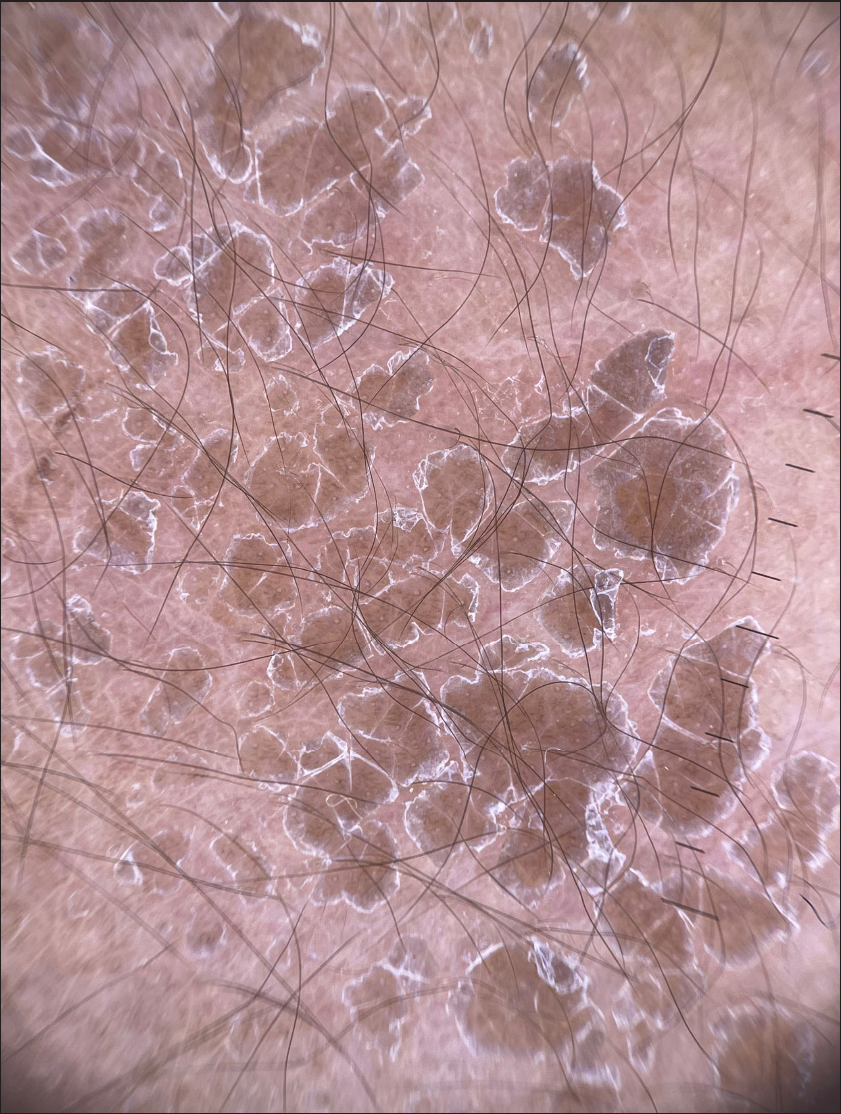
- Dermoscopy image of resolving stage showing greyish-brown oval to polygonal scaling on background of erythema
Dermoscopy of the active stage revealed multiple erosions surrounded by brownish crust in a linear (4/10; 40%) and hexagonal pattern (2/10; 20%) with surrounding greyish-white semi-adherent scaling on the background of erythema [Figure 1c]. Dermoscopic evaluation of the resolving stage showed greyish-brown oval to polygonal scaling on background of erythema in 60% (6/10) of the patients with prominent eccrine openings and none of the patients had erosions [Figure 2b and Table 2]. Histopathological examination done in 2 patients revealed eroded epithelium, spongiosis, papillary dermal edema and mild superficial dermal perivascular infiltrate of lymphocytes and histiocytes [Figure 3]. All patients were treated with a once-daily application of mometasone furoate 0.1% cream and anti-histamine. There was complete resolution of the lesions and symptoms within 7 days in 90% (9/10) of the patients and lesions resolved after 12 days in one (1/10; 10%) patient. None of the patients had any residual changes [Figure 1d]. All patients were advised to avoid strenuous activity in hot and low humid environment to prevent recurrence.
| Dermoscopic features | Number (percentage) |
|---|---|
| Active stage | |
| Multiple erosions with brown crusting | 4 (40) |
| Linear pattern | 4 (40) |
| hexagonal pattern | 2 (20%) |
| Background erythema | 4 (40) |
| Prominent eccrine openings | 4 (40) |
| Resolving stage | |
| Greyish-brown oval to polygonal scaling | 6 (60) |
| Background of erythema | 6 (60) |
| Prominent eccrine openings | 6 (60) |
| Erosions | 0 (0) |
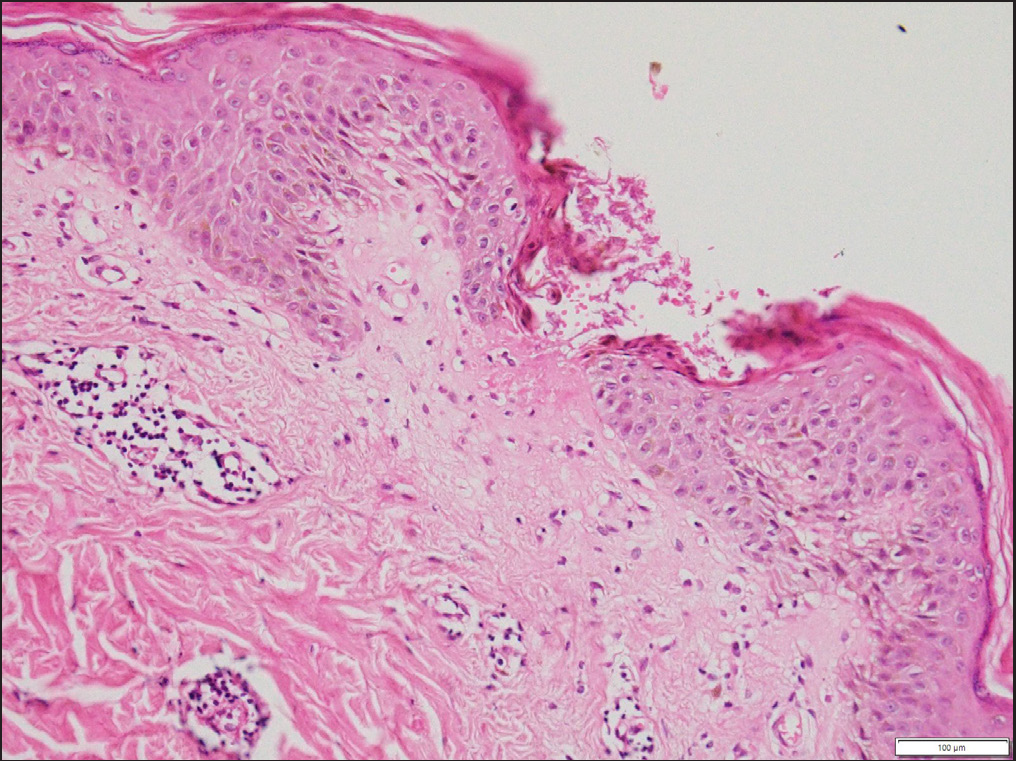
- The skin biopsy shows eroded epithelium, spongiosis, and superficial dermal mild perivascular infiltrate of lymphocytes and histiocytes (Hematoxylin and eosin, x400)
Sweat dermatitis is one of the important causes of morbidity in tropical countries and is commonly seen in the 3rd–4th decade in the summer season. The prolonged exposure to sweat under occlusion causes cumulative damage to stratum corneum and facilitates delivery of other irritants leading to dermatitis. Use of synthetic clothes increases risk of sweat dermatitis as they do not absorb sweat.7 Two morphological types were observed in our patients, acute and resolving stage. This classification was done based on the morphology (erythematous papules and background of erythema in active stage and only scaling on background of hyperpigmentation in resolving stage) and mean duration of disease (3.2 days in active stage and 11.3 days in resolving stage; P = 0.02).
Soni et al. described dermoscopy of sweat dermatitis as brown, fissured plaque, which showed deep brown pigmentation with superimposed scaling at some places, along with increased skin markings. Another case of maculopapular sweat dermatitis showed focal areas of necrosis and yellow-white lacunar areas giving rise to starry sky appearance.5,7 Our patients also showed greyish-brown scaling on the background of erythema in lesions in resolving stage. Multiple linear erosions with brownish crusting in a hexagonal pattern seen in active stage was a novel finding in our case series. Multiple linear erosions and crusting in a patterned distribution are caused due to extravasated sweat-induced irritant reaction and correspond to the epidermal erosions seen histologically. Interestingly, this feature was observed only in patients who presented early in the course of the disease (active stage). Exaggerated reticular network and background erythema surrounding the dilated eccrine openings depicts eccrine gland inflammation.
Differential diagnosis of sweat dermatitis is miliaria rubra, which also presents with multiple erythematous non-follicular papules over back. Dermoscopy of miliaria rubra is distinct and is characterized by central white area surrounded by a darker halo resembling bull’s-eye which differentiates it from sweat dermatitis.8 Skin biopsy could be helpful in doubtful cases to rule out other differential diagnoses such as miliaria rubra.
Sweat dermatitis has an acute onset of presentation and has spectrum of clinical manifestations depending on the timing of presentation with a rapid response to treatment. Dermoscopy can be a good adjunct in the diagnosis that helps in better management of patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interests.
References
- Frictional sweat dermatitis. Contact Dermatitis. 1998;38:49-50.
- [CrossRef] [PubMed] [Google Scholar]
- A study of desert dermatoses in the Thar Desert region. Indian J Dermatol. 2015;60:21-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A cross-sectional study of sweat-induced dermatitis during a South Indian summer: a glimpse of sweat gland-mediated cutaneous inflammation. Int J Dermatol 2019:86-90.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical presentation of sweat dermatitis with review of literature. Indian Dermatol Online J. 2019;10:698-703.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Delhi suffers at 49C as heatwave sweeps India. BBC News, May 16, 2022, https://www.bbc.com/news/world-asia-india-61242341.
- Descriptive study of sweat dermatitis: A rare dermatoses not so rare in tropics, Medical Journal Armed Forces India. Available at: https://doi.org/10.1016/j.mjafi.2022.11.004
- [Google Scholar]
- Bull’s-eye pattern in miliaria rubra. Australas J Dermatol. 2014;55:263-5.
- [CrossRef] [PubMed] [Google Scholar]






