Translate this page into:
An uncommon presentation of a common disease – Pure neural Hansen’s disease with sinus on skin
Corresponding author: Dr. Ritu Gujarati Vishwanath, Department of Dermatology, Venereology and Leprology, RiVa Skin and Plastic Surgery Clinic, Hanamkonda, Warangal, India. drrituvarun@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vishwanath RG. An uncommon presentation of a common disease – Pure neural Hansen’s disease with sinus on skin. Indian J Dermatol Venereol Leprol. 2025;91:S52-S54. doi: 10.25259/IJDVL_1177_2023
Dear Editor,
Leprosy/Hansen’s disease is a chronic granulomatous infection caused by Mycobacterium leprae and Mycobacterium lepromatosis. It commonly involves peripheral nerves and skin. Occasionally, isolated nerves are involved without skin lesions, called pure neuritic Hansen’s disease. The original defination of pure neural leprosy according to the Indian Association of Leprologists (IAL) five type classification (1982) is absence of any skin lesions. Single or multiple larger nerve trunks/branches may be enlarged and there is sensory loss along the distribution of affected nerves. Slit skin smears are negative. Lepromin reaction is generally positive. Nerve histology could be of tuberculoid, borderline or non-specific type.1 Neuritis in leprosy is a sub-acute, demyelinating and non-remitting event involving cutaneous nerves and larger peripheral nerve trunks. This presents as dryness, hypoaesthesia, tingling and numbness in the area supplied by the involved nerve, atrophy of the involved muscle, abscess of the nerve and neuralgic pain. Diagnosing such cases is challenging and needs exclusion of other common diseases like tuberculosis, diabetes mellitus, hypertension-induced peripheral neuropathy and neural tumours.2 We present a rare case of pure neural Hansen’s disease with sinuses on the skin. A 13-year-old boy presented to our clinic with oozing from the lower arm for 4 months and occasional pain. He complained of tingling in the left hand and weakness of fingers. There was no history of preceding trauma, fever, weight loss or cough. The general condition of the child was good. There was no epitrochlear or axillary lymphadenopathy. Systemic examination was normal. Cutaneous examination revealed puckered plaques with seropurulent discharge and crusting on the medial aspect of the left lower arm [Figure 1]. The left ulnar nerve was beaded and thickened with grade 1 tenderness. There was hypoaesthesia, partial/ulnar claw hand with decreased power and atrophy of hypothenar muscles. Pure neural Hansen’s disease with ulnar nerve abscess and ulnar nerve tuberculoma were the differentials considered. Complete blood picture, erythrocyte sedimentation rate and G6PD levels were normal. Slit skin smear, Mantoux test, Tb Quantiferon gold and pus for culture sensitivity was negative. Patient’s parents didn’t consent for nerve biopsy. A nerve conduction study showed decreased amplitude and increased latency of the ulnar nerve. High Resolution Ultrasound (HRUS) of the left ulnar nerve revealed multiple linear hypoechoic tracts (maximum 10 × 3 mm) extending into the adjacent perineural space and sinus on skin [Figures 2 and 3]. Diagnosis of pure neural Hansen’s disease with sinus was considered and treatment was initiated with paucibacillary multi-drug regimen for 6 months. Claw hand improved, discharge subsided and plaques healed with scarring [Figure 4].

- Puckered plaques with crust on the medial aspect of the left lower arm.
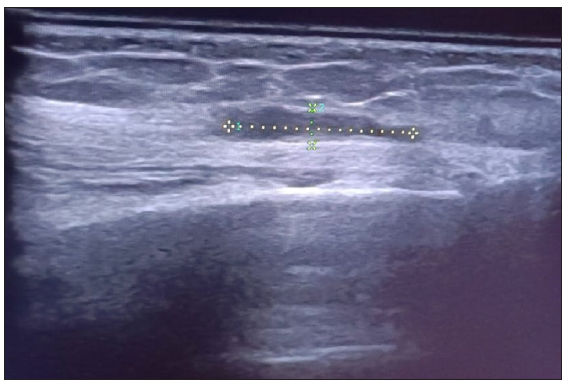
- Multiple linear hypoechoic tracts (maximum 10 × 3mm) extending into perineural space along the nerve.
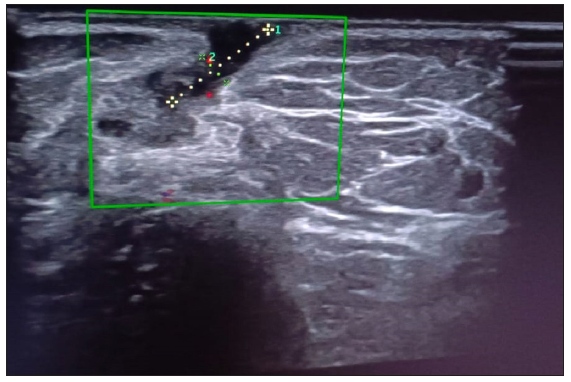
- Hypoechoic tract (sinus) extending onto the skin surface (Green square highlights the selected area).

- Healed lesions with scar.
Ulnar neuritis with disability frequently occurs in Hansen’s disease. Pure neural Hansen’s is a diagnostic challenge. Depending upon the patient’s immunity, it varies from tuberculoid to lepromatous. Young children and teenagers account for most cases. Ulnar, posterior auricular, peroneal and posterior tibial nerves are most commonly affected.3 However, Mittal et al. reported involvement of brachial plexus. As skin lesions are absent in pure neural Hansen’s cases, other non-lepromatous aetiologies like compression, trauma,4 tuberculosis, diabetes, hypertension, nerve sheath tumours2 and rarely neurofibromatosis, syphilis and amyloidosis5 must be ruled out. Nerve conduction studies, magnetic resonance imaging, HRUS-guided fine needle aspiration cytology and nerve biopsy with acid fast/Fite-Faraco staining helps in the diagnosis. Nerve abscesses are usually observed in tuberculoid spectrum of pure neural Hansen’s disease,1-6 but, sinus over skin is very rare. In these cases, ulnar nerve tuberculoma7 must be ruled out. Loss of sensation on the left hand, partial claw hand, thickened ulnar nerve and HRUS corroborated the diagnosis in our patient. Early diagnosis is essential to preserve the nerve functions and avoid permanent disability. Multi-drug therapy, oral corticosteroids, nerve decompression, drainage of abscess if needed, splints and physiotherapy are the possible treatment options for neuritis. Lack of histopathology is a limitation in this case.
In a country like India which still accounts for over 50% of the global burden of leprosy cases, any case of hypoesthesia or muscle weakness with thickened nerves must be evaluated in detail to rule out pure neuritic leprosy. We present a case of pure neural Hansen’s disease with sinuses on the skin which improved with multi-drug therapy. Partial claw hand improved with splint and physiotherapy subsequently.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pure neuritic leprosy: Current status and relevance. Indian J Dermatol Venereol Leprol. 2016;82:252-61.
- [CrossRef] [PubMed] [Google Scholar]
- Hansen’s disease with pure nerve involvement and perineural abscess mistaken for peripheral nerve sheath tumour. EMJ. 2023;10306433
- [CrossRef] [Google Scholar]
- Brachial plexopathy with ulnar nerve abscess in leprosy: A case showing importance of magnetic resonance neurography with clinical, imaging and histopathological correlation. Indian J Dermatol Venereol Leprol. 2022;88:385-8.
- [CrossRef] [PubMed] [Google Scholar]
- The red flags of ulnar neuropathy in leprosy. PLoS One. 2021;16:e0259804.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pure neural leprosy or amyloid neuropathy? Systematic review and clinical case report. Rev Assoc Med Bras. 2021;67:140-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nerve abscess in Leprosy: A retrospective study. Lepr Rev. 1993;64:357-61.
- [CrossRef] [PubMed] [Google Scholar]
- Management of ulnar nerve tuberculoma: A challenge to plastic surgeons. Cureus. 2022;14:e23872.
- [CrossRef] [PubMed] [Google Scholar]





