Translate this page into:
An uncommon presentation of paediatric chronic graft-versus-host disease after umbilical cord blood transplantation: True lichen planus-like lesions
Corresponding author: Dr. Lai-San Wong, Department of Dermatology, Chang Gung Memorial Hospital-Kaohsiung Medical Center and Chang Gung University College of Medicine, Kaohsiung, Taiwan. laisan7@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hsu T, Wong L. An uncommon presentation of paediatric chronic graft-versus-host disease after umbilical cord blood transplantation: True lichen planus-like lesions. Indian J Dermatol Venereol Leprol 2023;89:160.
Sir,
Umbilical cord blood transplantation has become an alternative haematopoietic stem cell transplantation.1 In paediatric patients, it is especially popular due to its easier availability, tolerance of human leucocyte antigen disparity, and lower risk of graft-versus-host disease.1,2 However, cutaneous chronic graft-versus-host disease have been rarely reported even following umbilical cord transplantation in the paediatric population. We report a case of the disease after umbilical cord blood transplantation with an initial presentation with true lichen planus-like lesions, which are uncommon in paediatric graft-versus-host disease.
An 11-year-old girl presented with a two-month history of progressive generalised itchy skin rash on her limbs and trunk. She was a diagnosed case of acute lymphoid leukaemia since 3 years of age and had received umbilical cord blood transplantation from a human leucocyte antigen partially matched unrelated donor. The post-transplantation follow-up was uneventful until one year earlier when she developed diplopia, which was suspected to be caused by autoimmune-related arteritis or graft-versus-host disease. She had been taking 10 mg of prednisolone orally every day since then and diplopia had resolved. At the time of the current presentation, she only had skin symptoms and denied any gastrointestinal or other systemic symptoms. On physical examination, there was no icterus. Cutaneous examination showed multiple well-defined round to oval, erythematous to violaceous papules and plaques with whitish Wickham striae over her limbs and trunk [Figure 1a-c]. There were also whitish reticulate striae on the lips [Figure 1d]. The skin lesions were severely itchy and progressed from the lower limbs to the upper limbs, and eventually the trunk. Laboratory examination revealed normal renal function and mildly elevated liver enzymes. Despite the remarkable morphologic similarity with lichen planus, we made a tentative diagnosis of cutaneous graft-versus-host disease based on her history. The histopathological examination of skin biopsy specimen showed lichenoid dermatitis, with basal cell vacuolization, keratinocytic necrosis, and lichenoid infiltrate of lymphocytes involving hair follicles, which supported the diagnosis of graft-versus-host disease [Figure 2a and b].

- Generalised erythematous to violaceous papules on the trunk and limbs
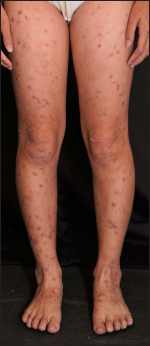
- Skin lesions on the lower limbs

- Close-up view of the papules with Wickham striae

- Whitish reticulate striae on lips
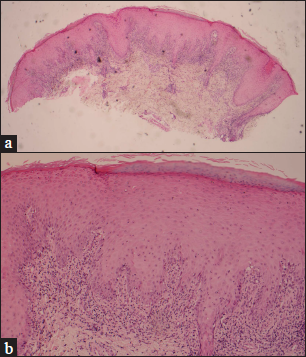
- (a) Lichenoid dermatitis involving hair follicles. (haematoxylin and eosin stain, ×25), (b) Lichenoid dermatitis. Basal vacuolation, keratinocytic necrosis and lichenoid infiltrate of lymphocyte involving dermis and hair follicles were evident. (haematoxylin and eosin stain, ×100)
The skin severity score was 2 based on the involved body surface area (19-50%) and the absence of sclerotic features, and the global severity of chronic graft-versus-host disease was moderate.3 We increased the dose of prednisolone to 30 mg daily and started oral tacrolimus at 2 mg daily, which was later titrated to meet satisfactory blood trough concentration. After the titration, we gradually tapered prednisolone. The skin lesions achieved a partial response with oral medications. Phototherapy with narrowband ultraviolet B was given for the recalcitrant lesions. Most lesions resolved with hyperpigmentation [Figure 3a-c].

- (a-c) Most lesions resolved with hyperpigmentation after treatment with oral tacrolimus and narrowband ultraviolet B phototherapy
Skin is the most common and often the earliest affected organ in both acute and chronic graft-versus-host disease.4 The diagnostic features of the disease include lichen planus-like lesions, poikiloderma, sclerotic features and morphea-like lesions and lichen sclerosus-like lesions.3 Although often being termed “lichen planus-like lesions” due to the appearance of violaceous patches and plaques, it rarely manifests as true lichen planus-like lesions in children.2,5 In this case, classic lichen planus-like lesions, characterised by well-defined erythematous to violaceous papules and overlying Wickham striae, were the earliest manifestations.
Graft-versus-host disease after umbilical cord blood transplantation are rarely reported, possibly due to its lower risk than in haematopoietic stem cell transplantation.1 There are multiple risk factors for developing acute and chronic graft-versus-host disease including donor-recipient human leucocyte antigen disparity, an unrelated donor, an older age of the donor, a female donor to a male recipient, conditioning regimens, transplant methodologies and a donor leucocyte infusion. A previous history of acute graft-versus-host disease is also associated with an increased risk of developing chronic graft-versus-host disease.3 Possible risk factors in our case included the partially mismatched human leucocyte antigen typing and the diplopia that possibly resulted from an episode of acute graft-versus-host disease.
Documenting all clinical features, grades, and severity of chronic graft-versus-host disease is essential because these are important in both selecting strategy of treatment and predicting prognosis.3,4 The treatment needs a multidisciplinary approach and delicate adjustment of doses of immunosuppressants based on the condition of the individual patient.3,4 Symptomatic mild cutaneous graft-versus-host disease, which is defined as localized cutaneous involvement, can be treated with topical corticosteroids or topical calcineurin inhibitors.3,4 In moderate to severe cases with extensive involvement (affected body surface area more than 19% or presenting with sclerotic features) or involvement of three or more organs, systemic immunosuppressive therapy should be considered. Systemic corticosteroids remain the mainstay of therapy for chronic graft-versus-host disease. Calcineurin inhibitors, rituximab, mycophenolate mofetil, extracorporeal phototherapy and phototherapy with psoralen combined with ultraviolet A, ultraviolet A alone, or narrowband ultraviolet B are alternative options.2,3 In our patient, the extensive involvement of the disease warranted oral steroid, which successfully reduced the size and severity of the lesions. Follow-up narrowband ultraviolet B phototherapy achieved a good response in the remaining skin lesions.
Declaration of patient consent
The authors certify that the patient consent is waived by the Institutional Review Board for this case report.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Umbilical cord blood transplantation: The first 25 years and beyond. Blood. 2013;122:491-8.
- [CrossRef] [PubMed] [Google Scholar]
- Paediatric cutaneous graft versus host disease: A review. Curr Pediatr Rev. 2017;13:100-10.
- [CrossRef] [PubMed] [Google Scholar]
- National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389-401.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous graft-versus-host disease: Diagnosis and treatment. Am J Clin Dermatol. 2018;19:33-50.
- [CrossRef] [PubMed] [Google Scholar]





