Translate this page into:
Anaplastic large cell non Hodgkin's lymphoma presenting as diffuse cutaneous hyperpigmentation
2 Department of General Medicine, Government Medical College, Kozhikode, Kerala, India
3 Department of Pathology, Government Medical College, Kozhikode, Kerala, India
Correspondence Address:
Sarita Sasidharanpillai
“Rohini,” Girish Nagar, Nallalom PO, Kozhikode - 673 027, Kerala
India
| How to cite this article: Sasidharanpillai S, Abdul Latheef EN, Kumar PJ, Sathi PP, Manakkad SP, Jishna P, Smitha T, Vidya AS. Anaplastic large cell non Hodgkin's lymphoma presenting as diffuse cutaneous hyperpigmentation. Indian J Dermatol Venereol Leprol 2018;84:316-320 |
Sir,
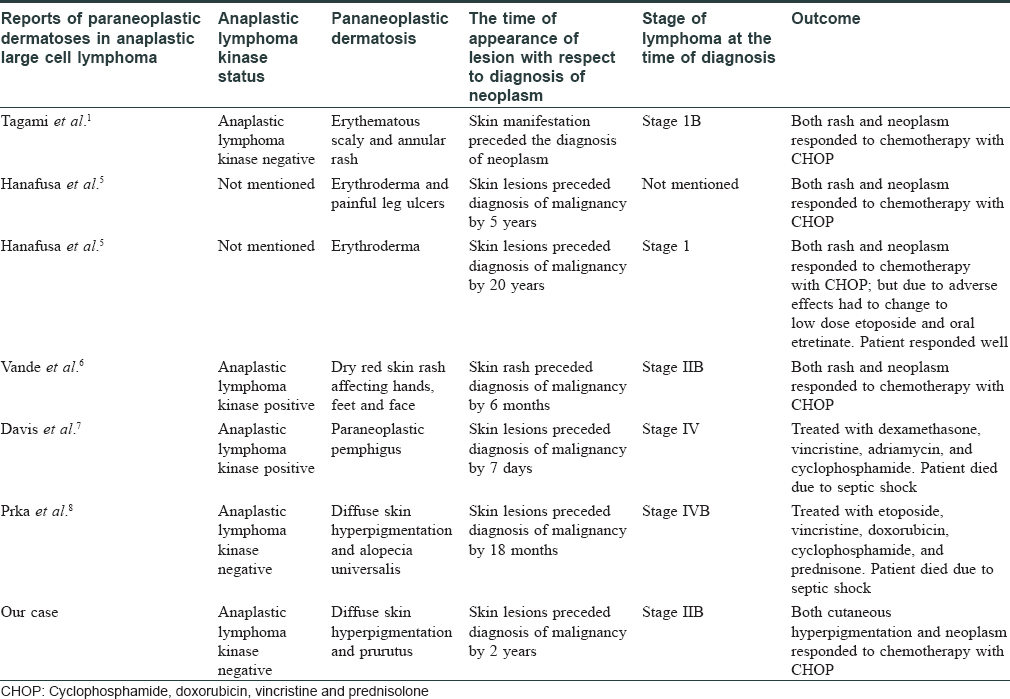
Paraneoplastic dermatoses often help in the early detection of underlying neoplasms. Paraneoplastic dermatoses documented in anaplastic large cell lymphoma include diffuse erythroderma, skin ulceration, annular rash and paraneoplastic pemphigus.[1]
We report a young male with anaplastic large cell lymphoma who presented with progressive hyperpigmentation of skin.
A 29-year-old male patient attended the Department of Dermatology of Government Medical College, Kozhikode with diffuse hyperpigmentation and intractable pruritus (that did not respond to antihistamines, emollients and topical steroids) of 2 years' duration and significant weight loss for 6 months. No exacerbating factors or diurnal variation were observed for pruritus which involved his entire body. He was not on any medication prior to the onset of hyperpigmentation.
Clinical examination revealed generalized hyperpigmentation of the body [Figure - 1]a and palmar creases [Figure - 1]c with sparing of mucosae and nails. A single, firm, nontender and mobile lymph node of 2 cm × 2 cm was detected in the right axilla. He had low hemoglobin (10 g%), raised erythrocyte sedimentation rate (100 mm/aefh), hypochromic microcytic anemia on peripheral smear analysis, and elevated serum lactate dehydrogenase. Mantoux test and sputum examination for acid fast bacilli were negative. Serum levels of cortisol, ferritin, transferrin, and vitamin B12 were within normal limits. Ultrasonogram and computerized tomogram evaluation of the abdomen and pelvis and magnetic resonance imaging of the brain detected no abnormality. The probable differential diagnoses of diffuse hyperpigmentation such as drug intake, vitamin B12 deficiency, tuberculosis, human immunodeficiency virus infection, adrenal pathology, adrenocorticotropic hormone secreting tumors (normal serum cortisol and brain imaging), and hemochromatosis were ruled out. Chest radiography showed a homogenous opacity in the left lung field sparing the apical and lower zones.
 |
| Figure 1 |
High-resolution computerized tomogram of thorax detected an anterior mediastinal soft tissue density lesion (8.3 × 7.7 × 12.5 cm) with calcification infiltrating the chest wall and great vessels [Figure - 2].
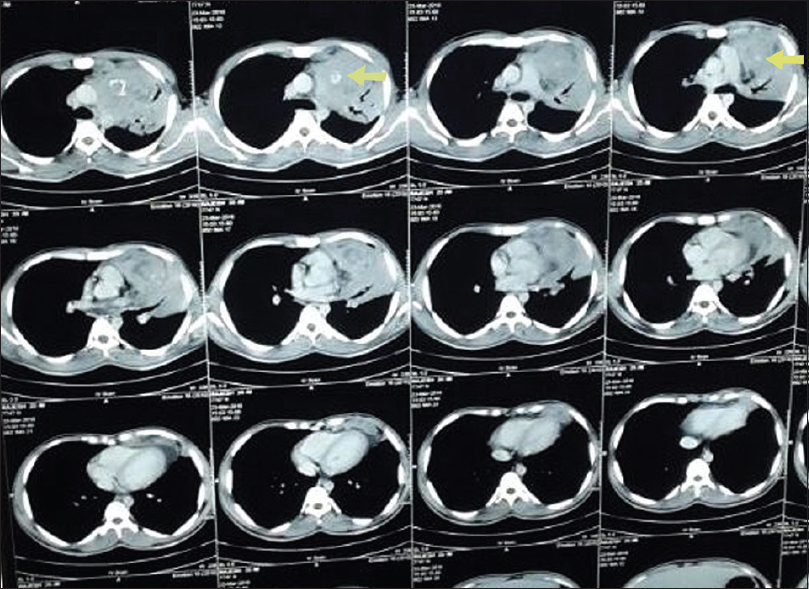 |
| Figure 2: High resolution computerized tomogram of the thorax showing an anterior mediastinal mass with calcification (arrow on left side) infiltrating the chest wall and great vessels (arrow on right side) |
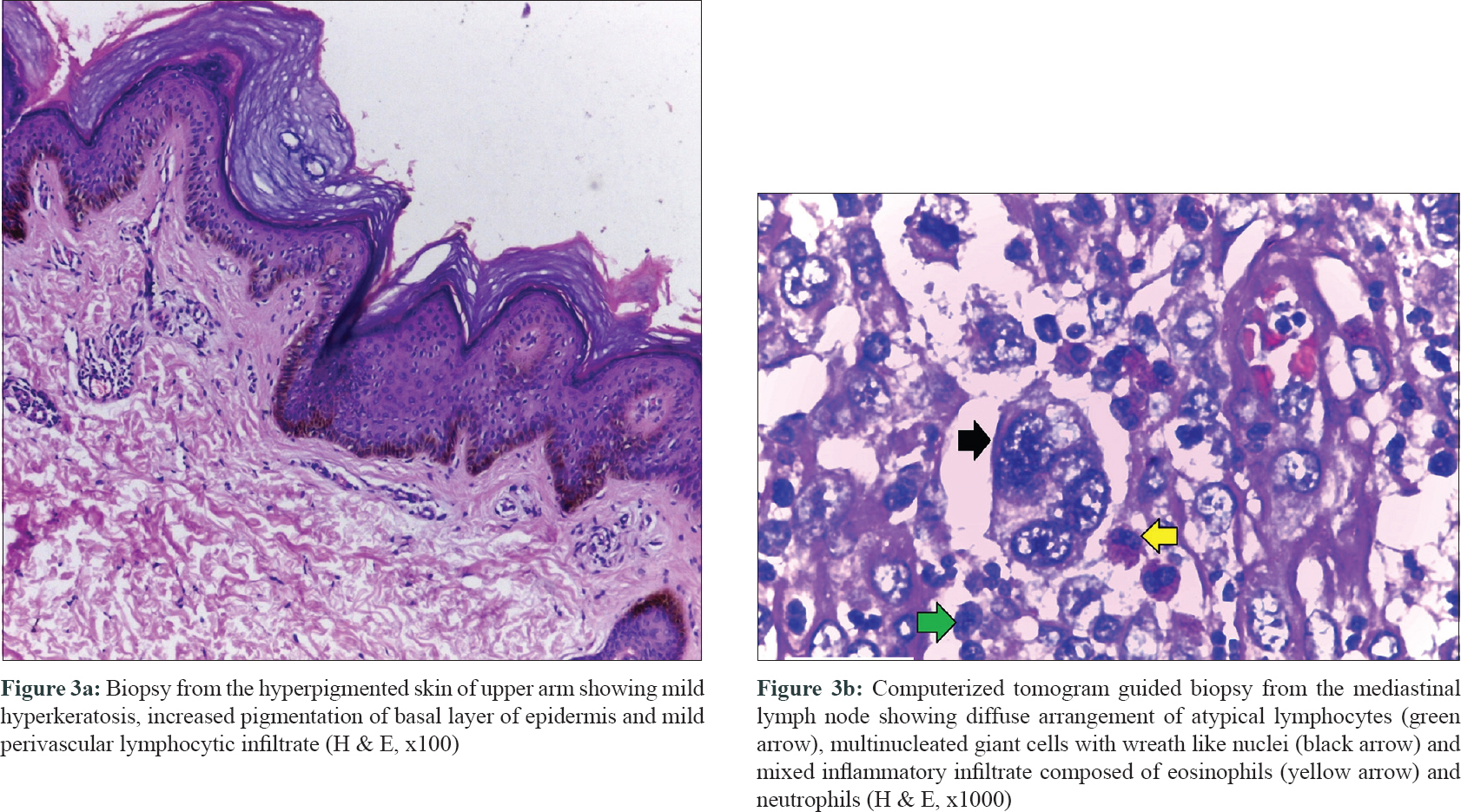
Biopsy from the hyperpigmented skin of upper arm showed increased pigmentation of basal layer of epidermis without any pigment incontinence [Figure - 3]a. Prussian blue staining failed to detect hemosiderin deposition.
 |
| Figure 3 |
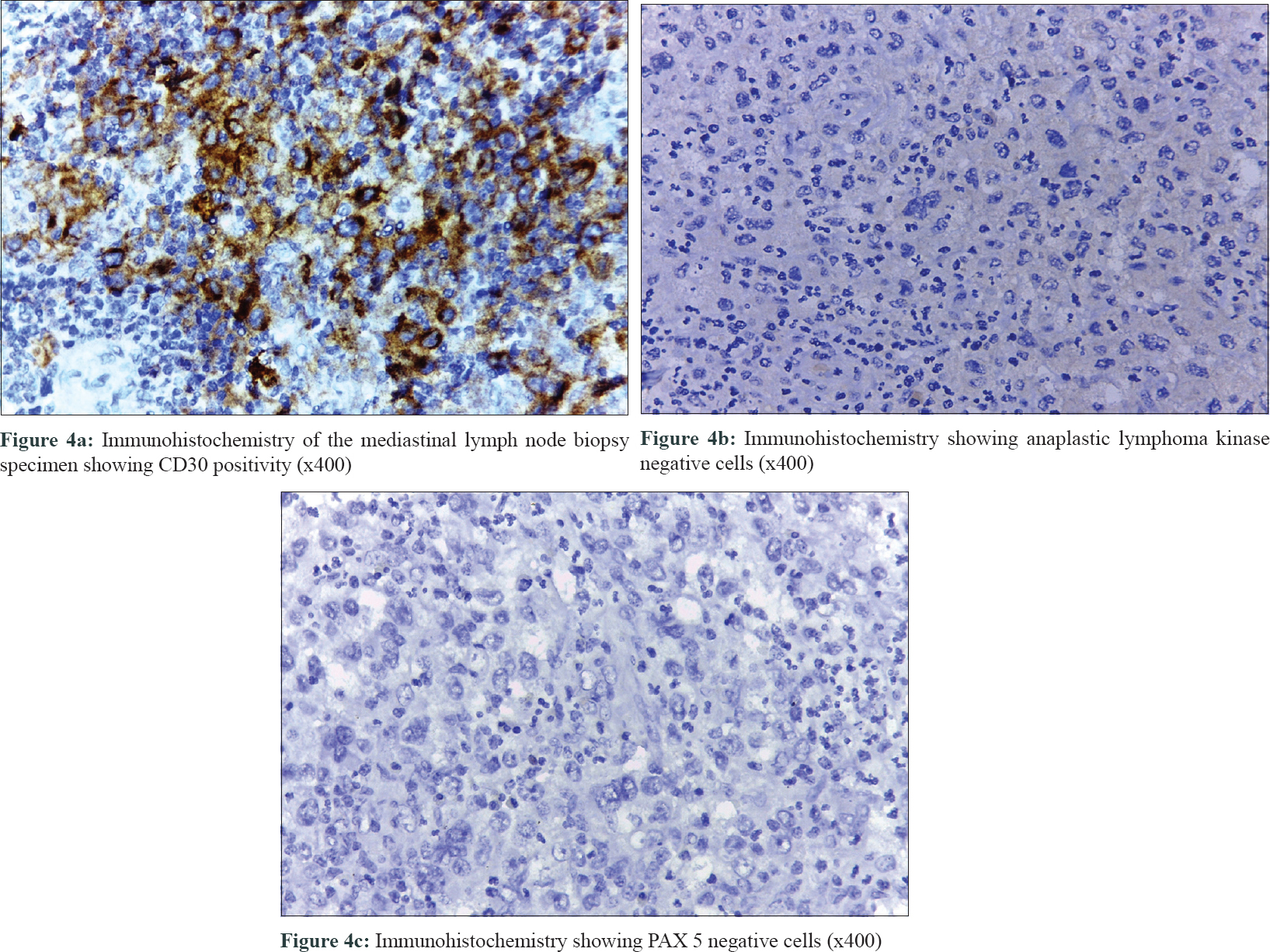
Computerized tomogram-guided biopsy from the mediastinal lymph node showed a neoplasm with atypical lymphocytes, multinucleated giant cells with wreath-like nuclei, and mixed inflammatory infiltrate composed of eosinophils and neutrophils [Figure - 3]b. Immunohistochemistry found the cells to be positive for CD3, CD30 [Figure - 4]a, and epithelial membrane antigen (EMA) and negative for CD20, CD15, anaplastic lymphoma kinase [Figure - 4]b, and paired box (PAX) 5 [Figure - 4]c confirming the diagnosis as anaplastic large cell non-Hodgkins lymphoma- stage 2B as per Ann Arbor staging system (International prognostic index score was 1) with generalized hyperpigmentation and pruritus as a paraneoplastic phenomenon.[2] Presently, 2 months after completion of chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone, the patient has attained complete resolution of neoplasm and pruritus, marked improvement in cutaneous hyperpigmentation and has gained weight [Figure - 1]b.
 |
| Figure 4 |
Anaplastic large cell lymphoma is categorized into anaplastic lymphoma kinase-positive and negative anaplastic large cell lymphoma and primary cutaneous anaplastic large cell lymphoma.[3] anaplastic lymphoma kinase positive anaplastic large cell lymphoma has better prognosis compared to anaplastic lymphoma kinase negative anaplastic large cell lymphoma.[3]
Lymph node histology and immunohistochemistry including negative staining for PAX 5 in our patient favored anaplastic lymphoma kinase negative anaplastic large cell lymphoma over Hodgkin's lymphoma which could also present with addisonian-like pigmentation without mucosal involvement.[3],[4] T cell gene rearrangement study, another important tool to distinguish Hodgkin's lymphoma, was not performed due to financial constraints. Angioimmunoblastic lymphoma and peripheral T cell lymphoma, not otherwise specified, were unlikely because they express less number of CD30 positive cells.[3]
Though the common age at diagnosis for anaplastic lymphoma kinase negative anaplastic large cell lymphoma is 40–65 years, it is occasionally reported in young individuals (as our patient).[3]
Clinical picture and skin biopsy findings in our case ruled out lichen planus pigmentosus, scleroderma, acanthosis nigricans and direct cutaneous involvement by anaplastic lymphoma kinase-negative anaplastic large cell lymphoma and pointed to diffuse hyperpigmentation and pruritus appearing as paraneoplastic phenomenon.
Relatively earlier stage of the disease (stage IIB) and a low international prognostic index score of 1 detected at the time of diagnosis could be a reflection of the cutaneous symptoms prompting the patient to seek early medical aid.[3]
We have come across only one other instance of anaplastic lymphoma kinase negative anaplastic large cell lymphoma manifesting with diffuse cutaneous hyperpigmentation in the literature where histology revealed hemosiderin deposition in macrophages [Table - 1].[1],[5],[6],[7],[8] The absence of the same along with the increased basal cell pigmentation observed in the skin biopsy of our patient denotes a role for melanocyte stimulating substances secreted by the tumor cells.
We report this case to highlight a rare presentation of anaplastic large cell lymphoma manifesting with diffuse cutaneous hyperpigmentation and pruritus which suggests that the combination of these symptoms should raise the suspicion of an underlying malignancy.
Acknowledgement
We are grateful to Dr. Neena Mampilli, Pathologist, Baby Memorial Hospital, Kozhikode for the invaluable help in carrying out the immunohistochemistry analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Tagami T, Alhalabi O, Ward N, Huang J. Paraneoplastic dermatosis in a patient with anaplastic large-cell lymphoma: Case report and literature review. Dermatopathology (Basel) 2016;3:39-43.
[Google Scholar]
|
| 2. |
International Non-Hodgkin's Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med 1993;329:987-94.
[Google Scholar]
|
| 3. |
Kinney MC, Higgins RA, Medina EA. Anaplastic large cell lymphoma: Twenty-five years of discovery. Arch Pathol Lab Med 2011;135:19-43.
[Google Scholar]
|
| 4. |
Garg S, Mishra S, Tondon R, Tripathi K. Hodgkin's lymphoma presenting as alopecia. Int J Trichology 2012;4:169-71.
[Google Scholar]
|
| 5. |
Hanafusa T, Igawa K, Takagawa S, Yahara H, Harada J, Tani M, et al. Erythroderma as a paraneoplastic cutaneous disorder in systemic anaplastic large cell lymphoma. J Eur Acad Dermatol Venereol 2012;26:710-3.
[Google Scholar]
|
| 6. |
Vande Walle N, Van den Enden E, Fostier K, De Coninck A, Nieboer K, Velkeniers B, et al. Systemic anaplastic large cell lymphoma presenting with cutaneous manifestations in a young man: A case report. Acta Clin Belg 2012;67:127-9.
[Google Scholar]
|
| 7. |
Davis AK, Cole-Sinclair M, Russell P. Anaplastic large cell lymphoma presenting with paraneoplastic pemphigus. J Clin Pathol 2007;60:108-10.
[Google Scholar]
|
| 8. |
Prka Z, Tomasovic-Loncaric C, Pejsa V, Nevajda B, Kusec R. Diffuse skin hyperpigmentation in CD30+ lymphoproliferation. Ann Saudi Med 2012;32:318-20.
[Google Scholar]
|
Fulltext Views
3,940
PDF downloads
3,736





