Translate this page into:
Anatopic response: Double sparing phenomenon in a patient with dapsone hypersensitivity syndrome
Correspondence Address:
Raghu Ram Maddala
1C, Street 12, Hospital Sector, Bhilai - 490 009, Chhattisgarh
India
| How to cite this article: Maddala RR, Ghorpade A, Adulkar S, Polavarapu M. Anatopic response: Double sparing phenomenon in a patient with dapsone hypersensitivity syndrome. Indian J Dermatol Venereol Leprol 2017;83:241-243 |
Sir,
Dapsone syndrome is also called the “five-week dermatitis” because it occurs suddenly, 5–6 weeks after the administration of dapsone. This drug-induced hypersensitivity syndrome. also known as “sulfone syndrome”, consists of exfoliative dermatitis and/or other skin rashes, generalized lymphadenopathy, hepatosplenomegaly, fever and hepatitis. Here, we report a case of dapsone hypersensitivity, where the rash affected the skin of whole body, yet spared the patches of leprosy and tinea versicolor.
A 26-year-old man, who was on multidrug treatment for borderline lepromatous leprosy for the past 1 month, presented with a history of high-grade fever for 1 week, yellowish discoloration of the sclera, and a reddish pruritic rash. There were erythematous papules and confluent plaques on his face, neck, trunk and limbs with conspicuous sparing of the distal limbs in a glove and stocking pattern. There were some areas of icteric skin in between the confluent erythematous rash [Figure - 1]. Further examination revealed sparing of the scaly macules of tinea versicolor on the trunk [Figure - 2]. Generalized lymphadenopathy was present. There was hypoesthesia on the distal spared zones and on the icteric patches on the elbows and the gluteal region. Multiple asymmetrical nerve thickening was noted. Investigations revealed a hemoglobin of 8 g% (13.8-17.2), white blood cell count of 5000/mm 3(4000-11000) and erythrocyte sedimentation rate of 40 mm after the first hour (<15). His liver function tests were abnormal with a direct bilirubin of 2.6 mg/dl (0.1 to 0.3), indirect bilirubin of 2.0 mg/dl (0.2-1.2), aspartate aminotransferase of 80 U/l (5-31), alanine aminotransferase of 38 U/l (5-35), alkaline phosphatase of 135 U/l (44-147), serum albumin of 2.7 g/dl (3.5-5) and prothrombin time of 15 s (10-13sec). Viral hepatitis serology was negative. Renal function tests were within normal limits. Abdominal ultrasound showed uniform liver enlargement. Chest radiograph was normal.
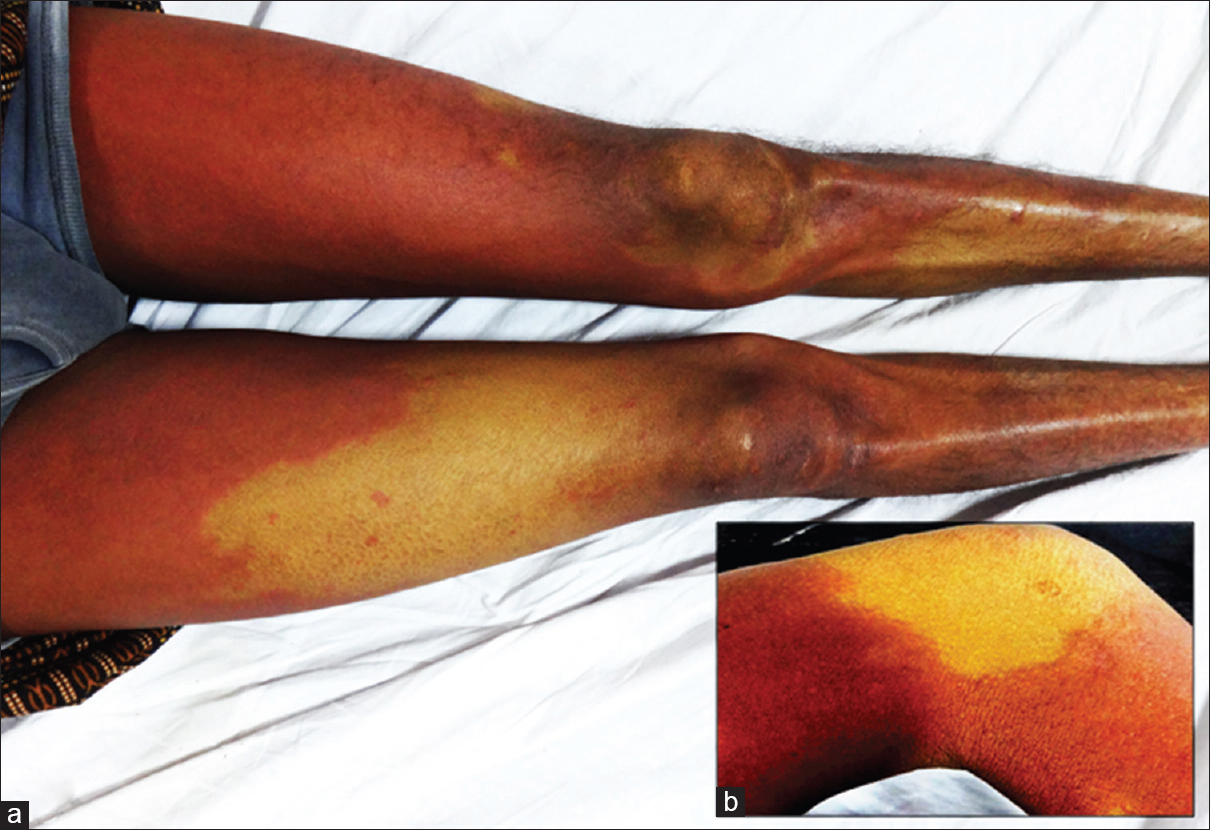 |
| Figure 1: (a) Erythematous rash on bilateral thighs with sparing of leprosy patches on the legs. (b) Icteric hypoesthetic patch spared in the background of dapsone rash |
 |
| Figure 2: (a) Spared patches of tinea versicolor lesions on the trunk, icteric hypoesthetic patches on both the elbows with visible, enlarged, right ulnar nerve. (b) Gluteal region showing uninvolved anesthetic patch (on 5th day of admission) |
A biopsy specimen from an erythematous plaque on the thigh showed focal exocytosis with a superficial perivascular lymphocytic infiltrate [Figure - 3]a. An incisional biopsy taken from the hypoesthetic patch on the leg revealed a flattened epidermis, separated from the dermal infiltrate by a Grenz zone of normal collagen, sparse lymphocytes and diffuse sheets of histiocytes in the mid and lower dermis [Figure - 3]b. Acid-fast bacilli were abundantly seen (4+).
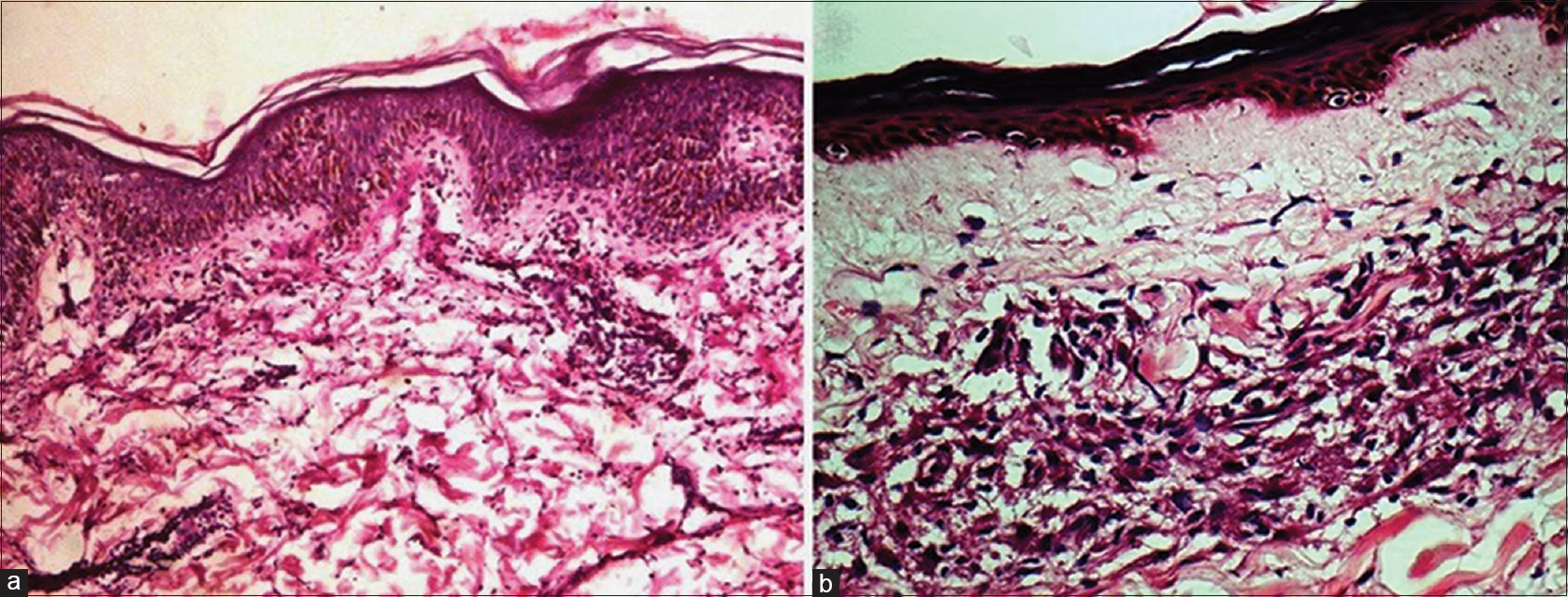 |
| Figure 3: (a) Epidermis showing spongiosis and upper dermis showing a lymphocytic infiltrate (H and E, ×400). (b) Flattened epidermis with Grenz zone of normal collagen. Mid- and lower dermis show diffuse sheets of histiocytes with sparse lymphocytes and (H and E, ×100) |
Dapsone hypersensitivity syndrome was diagnosed. Dapsone was stopped and he was given oral prednisolone 40 mg daily for 1 week, tapered to 30 mg daily for the next 14 days. The dose was further tapered over another 3 weeks. He was subsequently restarted on leprosy treatment consisting of rifampin 600 mg monthly and clofazimine 50 mg daily with no recurrence of the eruption.
Dapsone syndrome is a drug-induced hypersensitivity reaction. Although the exact immune mechanisms are unclear, a combination of type I, type IV and perhaps type III Gel and Coomb ' s hypersensitivity reactions are implicated in its pathogenesis. The generation of toxic metabolites such as nitrosamines, and possibly other compounds, through the N-hydroxylation pathway of dapsone metabolis, coupled with genetic and environmental factors, is considered vital in the etiology.[1]
Duration of onset of rash varies from 6 weeks to 6 months after initiating the treatment, to as short as 48 hrs. It is characterized by sudden onset of a papular or exfoliative rash, accompanied by fever, malaise and weakness, followed by jaundice and tenderness of the liver, lymphadenopathy and mononucleosis. In addition, hemolytic anemia, methemoglobinemia, eosinophilia, raised erythrocyte sedimentation rate, increased levels of serum bilirubin and raised liver enzymes may be seen.
The cutaneous manifestations of this syndrome show wide variations including erythroderma, papular erythematous eruptions, erythema multiforme, toxic epidermal necrolysis and Stevens–Johnson syndrome. Erythematous maculopapular rash and exfoliative dermatitis are present in the majority of cases.
The distinctive feature of our case was the sparing of leprosy patches and tinea versicolor lesions by the rash. The term “anatopic phenomenon” is used to describe this pattern, which includes the modulation of the inflammatory response of one dermatosis by another unrelated cutaneous infection at the same site.[2]
The accepted theory is that nerve damage in leprosy may affect the microvasculature and the local immune response resulting in the nonexpression of the hypersensitivity reaction, resulting in the “ islands of sparing in the deep red sea” picture.[3] The microvasculature of the skin is the final common pathway for the expression of erythema in various types of hypersensitivity reactions. Vasoactive amines that act on the microvasculature are also released by mast cells in type III hypersensitivity reactions (via complement activation) and type IV reactions (via interleukin-3).[4] Because the flare reaction is believed to be a neurogenic reflex, lack of neuropeptides will affect the expression of the drug reaction regardless of the type of hypersensitivity reaction involved. They have been found to enhance T-cell proliferation, immunoglobulin production, cytokine production/release and monocyte chemotaxis. Nerve damage in leprosy may not only affect the microvasculature, but may also affect the expression of a hypersensitivity reaction.
Two other cases have been reported under anatopic phenomena, including the sparing of leprosy patches by ampicillin hypersensitivity rash and dapsone hypersensitivity syndrome.[3],[4]
Four cases were reported by Pakran et al., in which unrelated dermatoses (viral exanthem, acute generalized exanthematous pustulosis, polymorphous light eruption and irritant contact dermatitis) spared the sites affected with tinea versicolor.[2] They speculated that the presence of Malassezia spp. may be responsible for this, either by providing a physical barrier or by means of local immunomodulation. A similar case of dithranol-induced erythema sparing tinea versicolor affected skin was previously reported by Shenoy et al.[5]
Acknowledgment
The authors sincerely acknowledge the contribution to Dr. Manish Kumar, Dr. Sanket Ukande, Dr. Vishwaja, Dr. Madhavi and Dr. Ankur for the valuable suggestions for the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Grossman SJ, Jollow DJ. Role of dapsone hydroxylamine in dapsone-induced hemolytic anemia. J Pharmacol Exp Ther 1988;244:118-25.
[Google Scholar]
|
| 2. |
Pakran J, Riyaz N. Interesting effect of Malassezia spp. infection on dermatoses of other origins. Int J Dermatol 2011;50:1518-21.
[Google Scholar]
|
| 3. |
Pavithran K. Sparing of leprosy macule in ampicillin hypersensitivity rash. Indian J Lepr 1987;59:309-12.
[Google Scholar]
|
| 4. |
Ng PP, Goh CL. Sparing of tuberculoid leprosy patch in a patient with dapsone hypersensitivity syndrome. J Am Acad Dermatol 1998;39(4 Pt 1):646-8.
[Google Scholar]
|
| 5. |
Shenoy SD, Wali I, Srinivas CR. Dithranol-induced erythema sparing hypopigmented lesions of pityriasis versicolor. Contact Dermatitis 1993;28:253.
[Google Scholar]
|
Fulltext Views
5,948
PDF downloads
2,176





