Translate this page into:
Angiotropic melanocytes: Possibly a distinctive finding in extra-facial acquired dermal melanocytosis
-
Received: ,
Accepted: ,
How to cite this article: Singh S, Elhence P. Angiotropic melanocytes: Possibly a distinctive finding in extra-facial acquired dermal melanocytosis. Indian J Dermatol Venereol Leprol 2023;89:65-70.
Abstract
Background:
Acquired dermal melanocytosis is a heterogenous group of hyperpigmented lesioins which predominantly involve the face.
Aim:
The aim of this study was to study the clinical presentation and histopathology of cases with extra-facial acquired dermal melanocytosis.
Methods:
Retrospective record analysis was performed between May 2016 to August 2019 to retrieve cases of extra-facial acquired dermal melanocytosis seen at the out-patient department of dermatology at the All India Institute of Medical Sciences, Jodhpur. Consecutive cases with histopathologically proven diagnosis of acquired dermal melanocytosis were included. Documentation of variation in clinical presentation and histopathologic findings was done in light of the existing literature.
Results:
Overall, four cases of extra-facial acquired dermal melanocyosis (female:male = 1:3) were seen during the study period. The lone case on head and neck involved the ear lobule and peri-auricular area. The other three cases had involvement of the hand. The histopathology confirmed the diagnosis of dermal melanocytosis but revealed peculiar findings of angiotropic melanocytes and dilated capillaries.
Limitations:
Small sample size and lack of comparison with perilesional normal skin were the limitations of this study.
Conclusion:
The findings of angiotropic melanocytes may be unique to extra-facial acquired dermal melanocytosis. This might indicate interaction between dermal melanocytes and capillary endothelial cells. This finding along with dermal capillary ectasia may indicate a possible role for vascular lasers in the management of these disorders.
Keywords
Acquired dermal melanocytosis
dendritic melanocytes
dermal melanocytosis
hand pigmentation
helix pigmentation
Plain Language Summary
Dermal melanocytosis is an uncommon condition of the skin caused by the presence of pigment-producing cells (i.e, melanocytes) below the top layer of the skin (i.e, below epidermis) and most cases are of infantile or childhood onset. Acquired dermal melanocytosis is an even rarer condition where this condition usually arises in adulthood and is more common on the face. We performed an analysis of all such patients having disease on areas other than the face seen by the lead author (SS) at the department of dermatology at AIIMS, Jodhpur (India). We found four patients (one female and the rest males) ranging in age from 21 years to 33 years. The female patient had pigmentation over the ear and rest all had the lesions on hands. The skin biopsy taken from these patients showed similar changes, namely, pigment-producing melanocytes that were seen surrounding the blood vessels in the skin. This is an extremely rare finding and its importance lies in the fact that there may be some cross-talk between the melanocytes and blood vessel cells. We suggest, that the pigment-reducing lasers may be combined with vessel-reducing lasers for improvement of such pigmentation disorders.
Introduction
Acquired dermal melanocytosis is an adult-onset pigmentary disorder originally characterized as symmetric bluish- brown macules on the face in Asian women.1 Owing to variable distribution of lesions, several variants have been defined including those of the hands, and face and extremities. Extra-facial distribution of this entity localized to the hand and helix is unusual.2,3 We report four patients with an unusual presentation of idiopathic acquired dermal melanocytosis and having a predominant perivascular distribution of dermal melanocytes on histopathology.
Methods
A retrospective data review was performed to retrieve all cases of extra-facial acquired dermal melanocytosis seen by the first author (SS) at the dermatology outpatient department of All India Institute of Medical Sciences, Jodhpur between May 2016 to August 2019. Only those cases which were proven to be dermal melanocytosis histologically and completed at least one follow up visit were included in the study. All the demographic, clinical and investigational records of these cases were reclaimed and studied in detail. Old histopathology slides were reviewed by both authors (SS and PE). Fresh sections were prepared from the paraffin-embedded blocks and staining with hematoxylin-eosin and immunohistochemistry was performed. Patients were contacted telephonically and requested to share their clinical course and treatment details along with a plea request for a fresh hospital visit.
Results
Over a period of 39 months (May 2016 to August 2019), 19 patients of dermal melanocytosis were seen by the lead author (SS). They were predominantly of the Mongolian spots type (12 patients), four were extra-facial acquired dermal melanocytosis and three were nevus of Ota type. No facial acquired dermal melanocytosis cases were seen in the out-patient department. Amongst the patients, there were three males and one female with a mean age of 27.25 + 5.05 years and a mean disease duration of 7.5 + 5.45 years. All patients had skin phototype four and none were outdoor workers. Overall, findings are summarized in Table 1.
| S.No | Age (years)/sex | Duration (years) | Site | Clinical findings | Histopathology and other investigations | Follow up |
|---|---|---|---|---|---|---|
| 1 | 21/Female | 3 | Left ear helix, pre-and post-auricular areas | Gradual onset, greyish-black pigmentation. Darker on the helix | Upper and mid dermis had moderate aggregate of dendritic melanocytes, more prominent around the capillaries. Dermal capillary dilatation and increased number seen Immunohistochemistry: S-100 and HMB-45 positive cells. Few also stained with CD 68 Patch testing with Indian Standard Series was negative |
4 years. No relief with topical depigmenting agents |
| 2 | 29/Male | 8 | Left hand | Bluish-brown pigmentation on the sparing the tips of fingers, distal one-fourth of the left palm and was limited by proximal palmar crease | Mild aggregate of dendritic melanocytes around the capillaries in upper dermis. Dermal capillary dilatation and increased number seen Immunohistochemistry: S-100 and HMB-45 positive cells |
3 years and 9 months |
| 3 | 33/Male | 4 | Left hand | Greyish-brown macules, ill-defined and discrete to coalescent on the palmar surface of the fingers and then onto adjacent palm limited by the proximal palmar crease | Mild aggregate of dendritic melanocytes around the capillaries in upper dermis. Dermal capillary dilatation and increased number seen. Immunohistochemistry: S-100 and HMB-45 positive cells | 3 years |
| 4 | 26/Male | 15 | Left hand (dorsum) and wrist | Greyish-brown macule over the dorsum of left hand and wrist with peripheral scatter and variegation of pigmentation without hypertrichosis | Mild to moderate aggregate of dendritic melanocytes around the capillaries in upper dermis. Dermal capillary dilatation and increased number seen Immunohistochemistry: S-100 and HMB-45 positive cells Patch testing with Indian Standard Series was negative |
2 years and 6 months |
Patient one was a 21-year-old college student with gradually progressive greyish-black pigmentation involving almost the entire left ear helix for three years. She had similar but fainter pigmentation over the left pre-auricular area and behind the ear [Figure 1a]. Patient two was a 29-year-old postgraduate with bluish-brown pigmentation on the left hand for eight years. His pigmentation was noted to spare the tips of fingers, distal one-fourth of the left palm and was limited by proximal palmar crease [Figure 1b]. Patient three was a 33-year-old businessman who presented with greyish-brown pigmentation on the left palm and fingers for four years. The macules were ill-defined and discrete to coalescent on the palmar surface of the fingers and the adjacent palm bounded by the proximal palmar crease. Patient four was a 26-year-old graduate with pigmentation over the dorsum of left hand for 15 years. He had a greyish-brown macule over the dorsum of left hand and wrist with peripheral scatter and variegation of pigmentation without hypertrichosis [Figure 1c]. Overall, the lesions were asymptomatic, insidious in onset and progressive at commencement but had stabilized over 1 to 2 years. There was no history of preceding trauma, local inflammation, drug intake, contact with metals/chemicals/ hair dye, topical hydroquinone application, significant sun exposure, photosensitivity or similar lesions in the family members in any of these patients. Other body sites, mucosae and nails were uninvolved. The provisional diagnoses included lichen planus pigmentosus, Becker’s melanosis, vascular malformation, contact pigmentation to hair dye, pigmented contact dermatitis and ochronosis (patient 1).

- Patient 1 – Blackish pigmentation involving the left helix. Faint greyish pigmentation is also noticed in the preauricular area

- Patient 2 – Bluish pigmentation on left hand, mainly over the palmar aspect of fingers with extension onto the palm

- Patient 4 – Dark brown pigmentation over the dorsum of left hand with extension onto the wrist. Peripheral part of the pigmentation is fainter
Patch testing with Indian standard series of allergens was performed in two patients (patient 1 and 4) and was inconclusive. Skin biopsies from all the patients showed unremarkable epidermis with presence of scattered spindle-shaped dendritic melanocytes prominently in a perivascular distribution in the superficial and mid-dermis with few cells going in between collagen fibres [Figures 2a-c]. Dermal capillaries appeared modestly dilated and increased in numbers and collagen was unremarkable. Immunohistochemistry revealed the melanin-containing dendritic cells to be strongly positive for S-100 and HMB-45, thus suggestive of dendritic melanocytes [Figures 3a-c]. However, few perivascular pigmented cells also showed positivity for CD-68, suggestive of melanophages. The dermal capillary dilatation which was not very apparent on routine hematoxylin-eosin stained sections was highlighted well on CD-31 immunostain. None of the patients could afford Nd-YAG laser treatment and a 4-6 months trial with topical depigmenting agents (2% kojic acid, 5% arbutin, 2% hydroquinone, 10% glycolic acid) failed to provide any improvement. The lesions in all patients have remained unchanged over the mean follow up period of 2.9 ± 0.3 years (2.5 to 3.3 years).
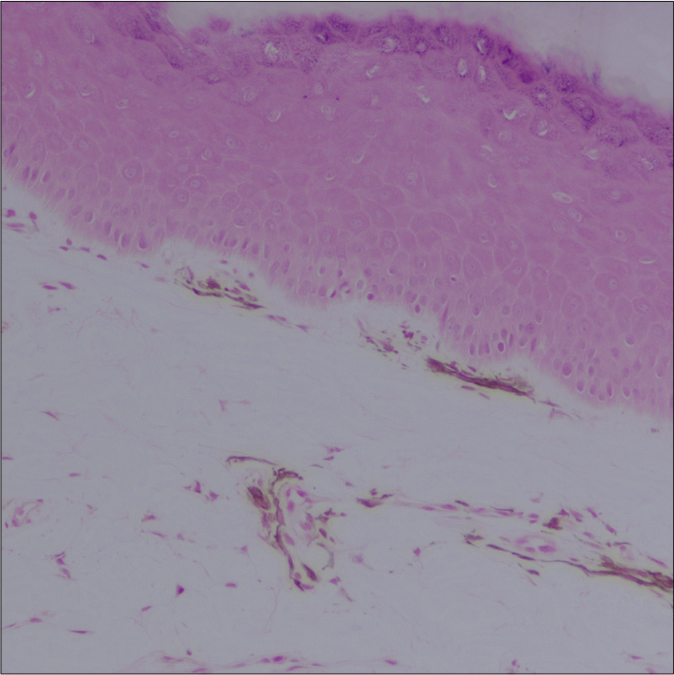
- Patient 2 – Melanocytes with long dendritic processes are seen surrounding the upper dermal capillaries (H and E, 20×)
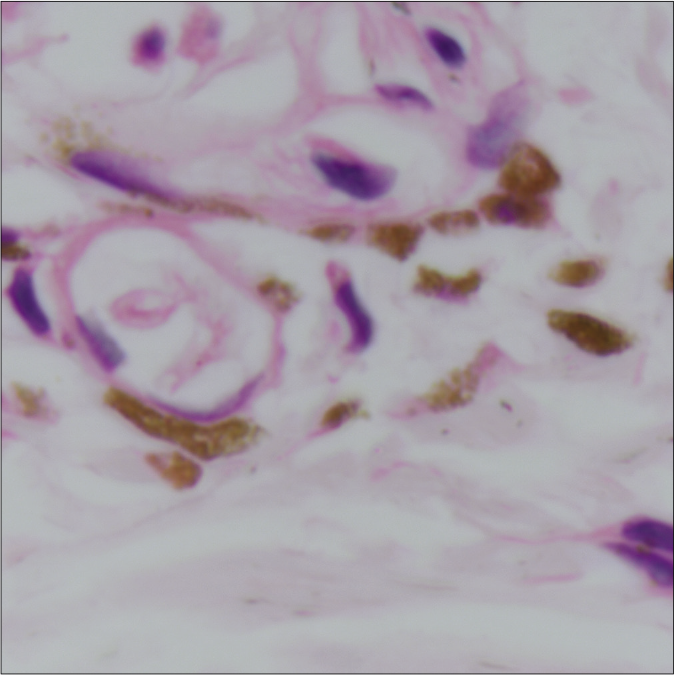
- Patient 3 – Pigment containing cells tightly surrounding upper dermal capillary system (H and E, 100×)

- Patient 4 – Pigment containing cells closely surrounding the mid dermal vascular plexus (H and E, 40×)
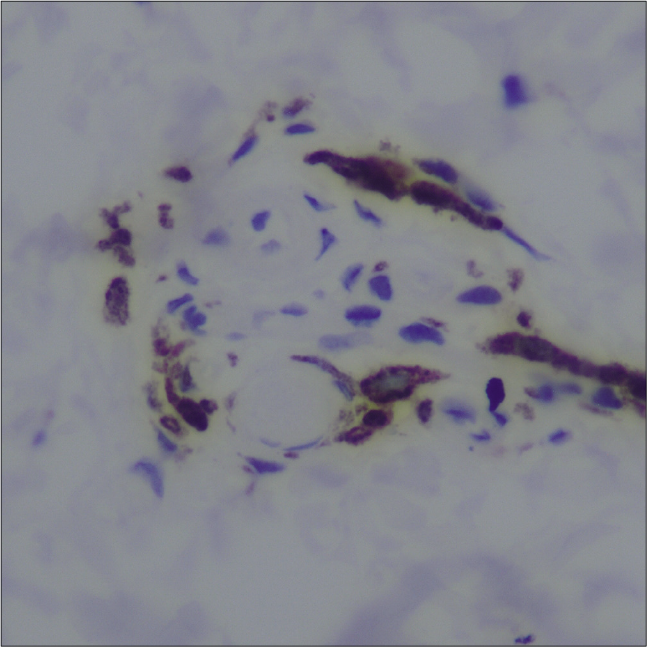
- Patient 2 – Dark-brown positive cells (cytoplasmic plus nuclear staining) closely surrounding the upper dermal vascular plexus (S-100 immunostain, 40×)

- Patient 3 – Dark-brown positive cells closely surrounding the mid-dermal vascular plexus (HMB-45 immunostain, 100×)
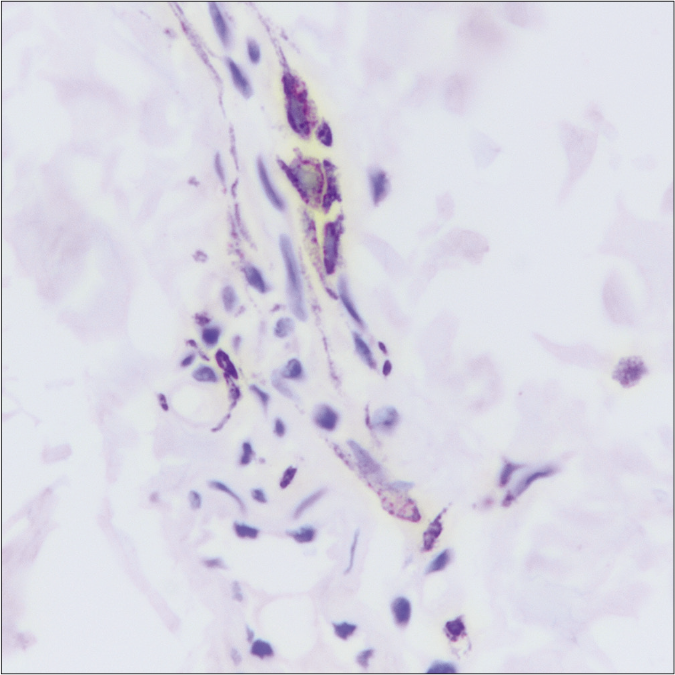
- Patient 4 – Dark-brown positive cells closely surrounding the mid-dermal vascular plexus (HMB-45 immunostain, 40×)
Discussion
Hori’s nevus is the traditionally cited example of acquired dermal melanocytosis and presents as symmetric patches on the face.1 There have been several reports of extra-facial acquired dermal melanocytosis occurring over the trunk and extremities. Lesions involving face and extremities have been named as acquired dermal melanocytosis on face and extremities but those features were lacking in our patients.4 Pigmentation localized to the hand can involve the dorsal and/or palmar aspects of the hand.2,5,6 Younger age at onset in our patients with hand lesions matches findings described in the literature but the predominance in males in our cases was at a variance from the usual. Even though our patient 1 nearly fits the literature description of C3 dermatomal dermal melanocytosis,3,7 her pigmentation was unusually localized to ear and was blackish and reticulated behind the ear. Being entirely asymmetrical, our patients posed diagnostic difficulty which was eventually resolved by histopathology.
The exact pathogenesis of pigmentation in acquired dermal melanocytosis is as yet unclear and several hypotheses have been proposed. Faulty migration of melanocytes from the neural crest to the basal layer of the epidermis may contribute to the occurrence of dermal melanocytes.5 Dermal melanocytes may descend from the basal layer of the epidermis or the hair follicle bulb.1 Various factors such as ultraviolet light, hormonal therapy like estrogen/ progesterone, persistent local inflammation as described in treated psoriasis, chemicals like hydrochloric acid, trauma or aging may lead to re-activation of immature dermal melanocytes.1,2 Mediators released from mast cells may also have a role in lesions associated with atopic dermatitis, in view of the proximity of melanocytes and mast cells observed in skin biopsies.8 It has been demonstrated that immature melanocytes are present in the dermis of both pigmented and perilesional uninvolved skin of these patients as well as healthy controls possibly since birth. These cells may be activated by known stimuli or there may not be any triggering factors and the melanin synthesizing potential of dermal melanocytes may grow slowly.9
The prominent presence of dermal melanocytes in a perivascular location in our patients has rarely been described in acquired dermal melanocytosis.2,6,10 Wang et al. described the presence of both melanocytes and mononuclear cells around upper dermal blood vessels, thereby suggesting inflammation as a possible trigger for melanocyte activation.10 On reviewing published images, we were able to identify two more reports of extra-facial acquired dermal melanocytosis with probably a prominent perivascular melanocytic infiltrate which was not mentioned in their histopathology description.3,11 There was no clinical or histological suggestion of inflammation in our patients. Lately there is growing evidence for role of endothelial cells in epidermal pigmentation in absence of ultraviolet exposure.12 Conversely, epithelial melanocytes have been shown to affect uveal vascularization through secretion of fibromodulin.13 Another anatomic area with angiotropic melanocytes is inner ear where it is known that perivascular-resident macrophage-like melanocytes are essential for the integrity of the intrastrial fluid-blood barrier.14 However, none of the above or similar functions have been elucidated for dermal melanocytes. Malignant melanoma arising in dermal melanocytosis is rare. It has more often been reported with congenital variants and in lesions involving head and neck region.15 Yet another observation which remains unexplained is the ectasia of dermal capillaries which was uniformly seen in all of our patients. However, we could not substantiate this feature in a more robust manner by comparing capillary density with perilesional clinically normal skin. There was no history of contributory factors like excessive sun-exposure or topical steroid application. The vascular dilatation was probably unrelated to lesional site as the latter was not uniform.
Despite performing histopathology and immunohisto chemical stains to confirm our findings, the generalizability of the same is restricted by low sample size in view of the fact that extra-facial acquired dermal melanocytosis is an uncommon disease. Another limitation was lack of perilesional skin biopsy which could have provided much-needed insight into the number and location of melanocytes in normal skin vis a vis lesional site.
Therefore, we suggest that the finding of perivascular (angiotropic) melanocytes and vascular proliferation may be peculiar of to extra-facial acquired dermal melanocytosis and may have a role in its pathogenesis due to ‘molecular crosstalk’ between endothelial cells and dermal melanocytes. The same hypothesis may be translated into possible therapeutic benefit using a combination of pigmentation and vascular lasers, which certainly requires corroboration in clinical studies. These patients require long term follow up in order to gain more knowledge about the natural course of this pigmentary condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acquired, bilateral nevus of ota-like macules. J Am Acad Dermatol. 1984;10:961-4.
- [CrossRef] [Google Scholar]
- Acquired dermal melanocytosis confined to the palm with a review of published cases of acquired dermal melanocytosis on the hands. J Dermatol. 2016;43:701-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermal melanocytosis of the helix. Pediatr Dermatol. 2010;27:305-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic features of acquired dermal melanocytosis of the face and extremities. Clin Exp Dermatol. 2018;43:806-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired dermal melanocytosis of the hand: A new clinical type of dermal melanocytosis. J Dermatol. 1993;20:561-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired dermal melanocytosis confined to the hand. Ann Dermatol. 2018;30:380-1.
- [CrossRef] [PubMed] [Google Scholar]
- A case of late onset dermal melanocytosis in the C3 dermatome. Indian J Dermatol Venereol Leprol. 2016;82:705-7.
- [CrossRef] [PubMed] [Google Scholar]
- Aquired symmetrical dermal melanocytosis (naevus of Hori) developing after aggravated atopic dermatitis. Br J Dermatol. 2005;152:903-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dormant melanocytes in the dermis: Do dermal melanocytes of acquired dermal melanocytosis exist from birth? Br J Dermatol. 1998;139:349-50.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired dermal melanocytosis: A case with conjunctival and gingival pigmentation. J Dermatol. 2004;31:752-5.
- [CrossRef] [PubMed] [Google Scholar]
- Late-onset acquired dermal melanocytosis on the hand of a Chinese woman. Indian J Dermatol Venereol Leprol. 2013;79:269.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial cells promote pigmentation through endothelin receptor B activation. J Invest Dermatol. 2015;135:3096-104.
- [CrossRef] [PubMed] [Google Scholar]
- Melanocyte-secreted fibromodulin promotes an angiogenic microenvironment. J Clin Invest. 2014;124:425-36.
- [CrossRef] [PubMed] [Google Scholar]
- Perivascular-resident macrophage-like melanocytes in the inner ear are essential for the integrity of the intrastrial fluid-blood barrier. Proc Natl Acad Sci U S A. 2012;109:10388-93.
- [CrossRef] [PubMed] [Google Scholar]
- Melanoma arising in a nevus of Ito: Novel genetic mutations and a review of the literature on cutaneous malignant transformation of dermal melanocytosis. J Cutan Pathol. 2016;43:57-63.
- [CrossRef] [PubMed] [Google Scholar]






