Translate this page into:
Angiolymphoid hyperplasia with eosinophilia associated with hepatitis C antibodies
Correspondence Address:
Nawaf Al-Mutairi
P.O. Box 280, Farwaniya 80000
Kuwait
| How to cite this article: Al-Mutairi N, Manchanda Y. Angiolymphoid hyperplasia with eosinophilia associated with hepatitis C antibodies. Indian J Dermatol Venereol Leprol 2007;73:367 |
Abstract
Angiolymphoid hyperplasia, for a long time, has been confused with Kimura's disease. In the recent past, various workers have tried to differentiate these two entities. Various new differences in immunohistochemistry have been found, which have not yet been included in the dermatology literature. In this case report, we have presented a middle-aged man complaining of recurrent nodular lesions on the right ear for 8 years. On examination there were multiple firm 0.5-2.0 cm size, erythematous to violaceous nodules located in and around the right ear. Regional lymph nodes were not involved, and there were no systemic complaints. Histopathological examination from the excision biopsy of one of the nodules revealed features classical of angiolymphoid hyperplasia with eosinophilia. Immunohistochemical stains carried out on the biopsy specimen revealed predominantly T-cell type of infiltrate. All routine investigations were within normal limits, and serum immunoglobulin E was marginally raised. He had positive anti-hepatitis C virus antibodies, an association not so far reported in the literature.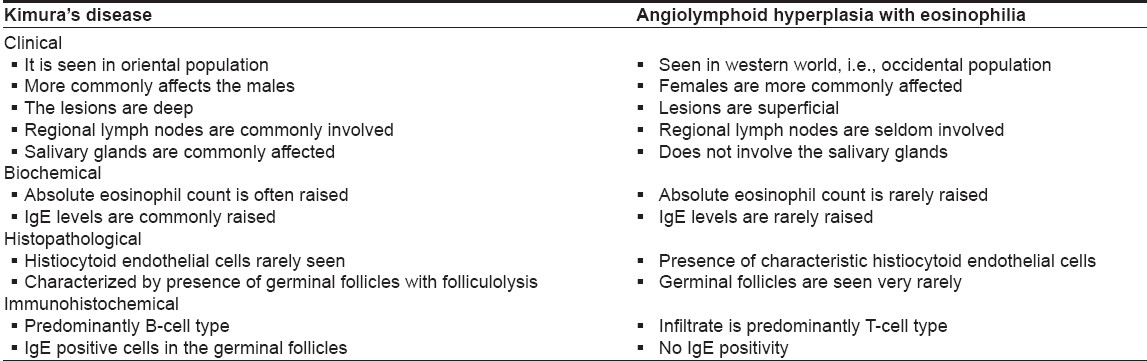
 |
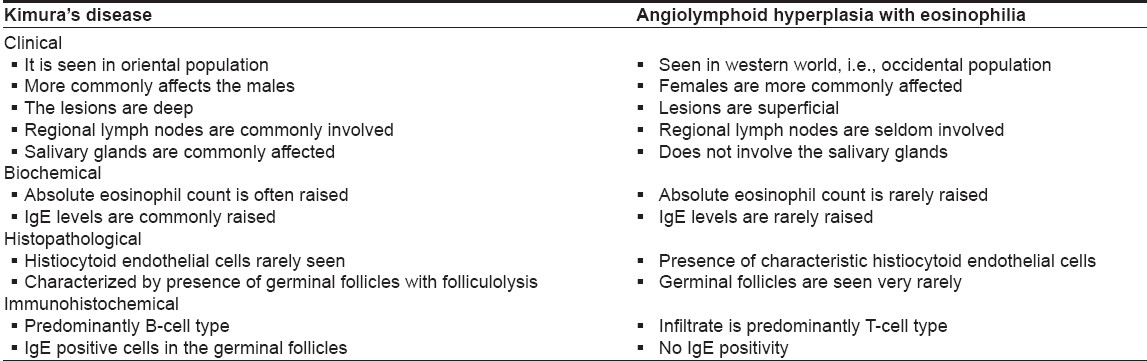
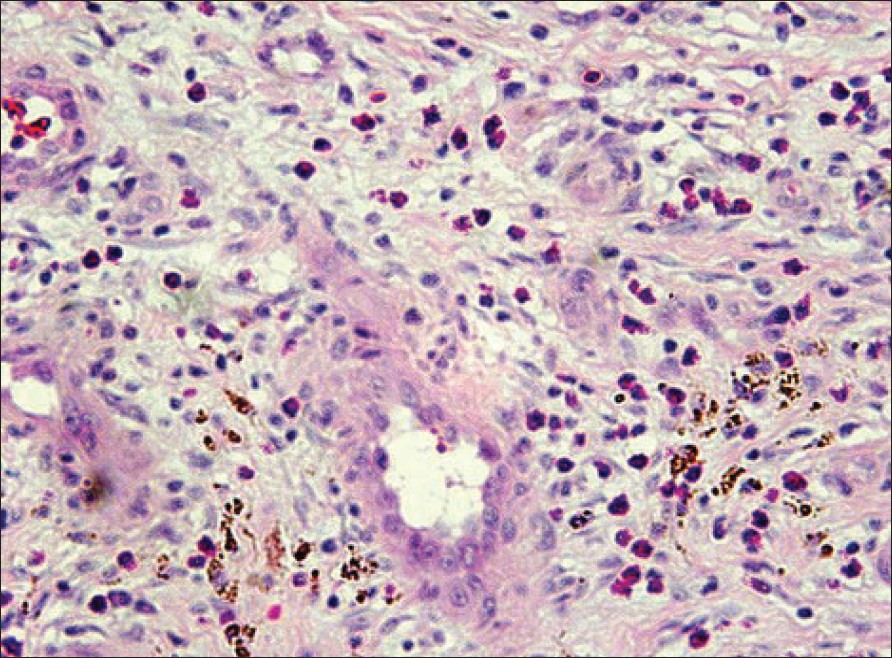
| Figure 3: Immunohistochemistry showing predominantly CD 3 positive cells in the dermal infiltrate (X100) |
 |
| Figure 3: Immunohistochemistry showing predominantly CD 3 positive cells in the dermal infiltrate (X100) |
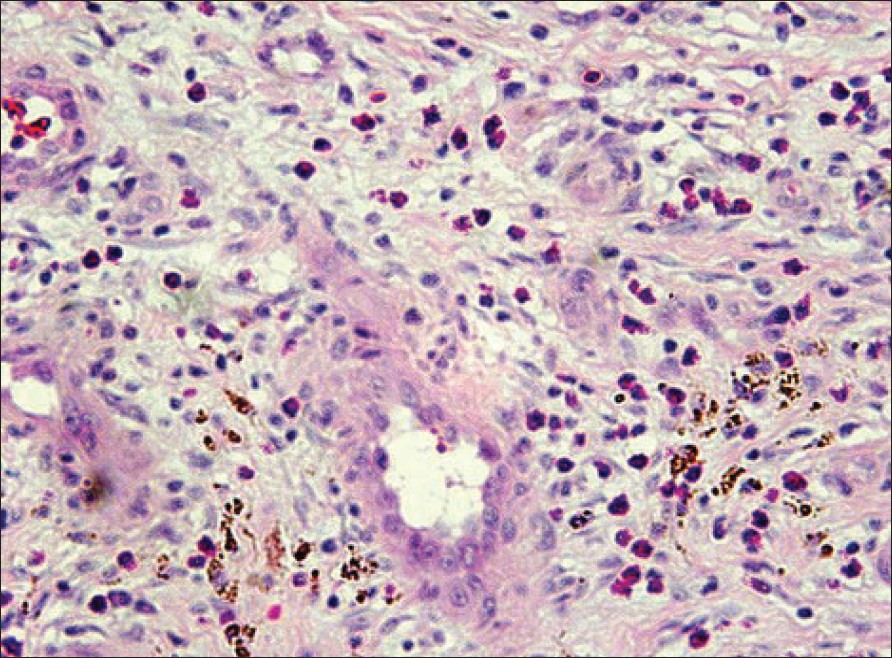 |
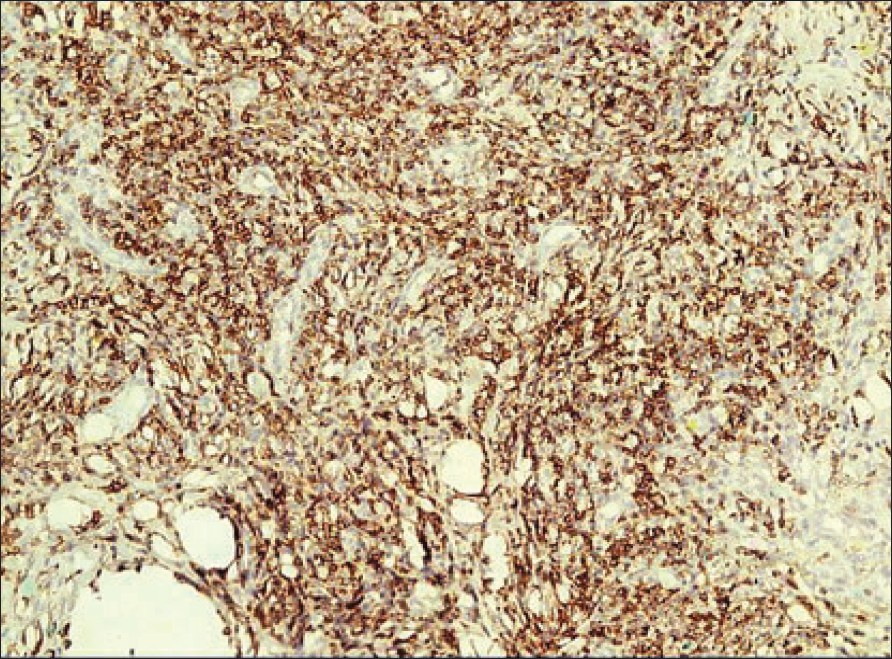
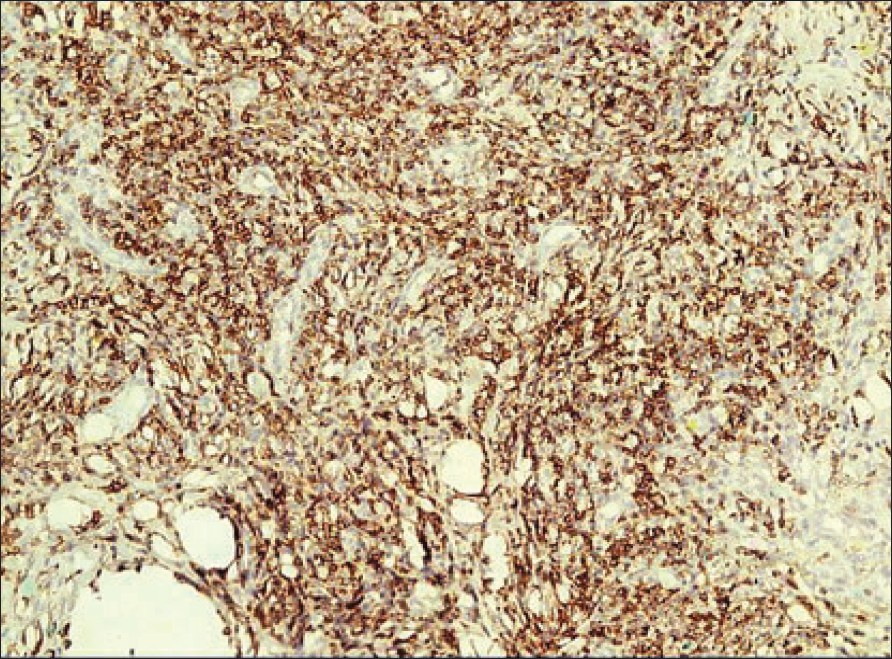
| Figure 2: Dilated dermal blood vessels with histiocytoid endothelial lining and surrounded by infi ltrate rich in eosinophils (H and E, X100) |
 |
| Figure 2: Dilated dermal blood vessels with histiocytoid endothelial lining and surrounded by infi ltrate rich in eosinophils (H and E, X100) |
 |
| Figure 1: Multiple skin-colored to violaceous firm nodules around the right ear |
 |
| Figure 1: Multiple skin-colored to violaceous firm nodules around the right ear |
Introduction
Angiolymphoid hyperplasia with eosinophilia is an entity distinct from Kimura′s disease. With the advancement of staining techniques, various new differences between the two entities have been unraveled. These differences have not yet gained place in the dermatology literature. Along with a case report, we have updated the differences between the two entities by including the same.
Case Report
A 40-year-old Syrian male complained of recurrent nodular lesions on the right ear for the last 8 years, with a history of bleeding on trauma. It started 8 years back as a single firm nodule on the concha of the right ear, which slowly increased in size over a period of 6-8 months. A year later it was surgically excised, but the condition recurred within the next 1 year. This time he gradually developed multiple lesions localized to the right ear, covering both the anterior and posterior aspects. There was no history of hearing problem or discharge from right ear. Also, he had no respiratory or ocular complaints. There was no history of recurrent headaches, seizures. There was no history suggestive of any high-risk behavior. On examination there were multiple 0.5-2.0 cm size firm nodules around the right ear, with involvement of the external auditory canal [Figure - 1]. The lesions were skin colored to slightly erythematous with a violaceous hue. They were not mobile on the underlying structures, and the overlying skin was attached to these nodules. Some of the nodules were covered by a hemorrhagic crust, but there was no discharge even on pressing them. The regional lymph nodes were not involved, and examination of the salivary glands did not reveal any abnormality. The examination of other organ systems, including chest, eye and ear, nose and throat evaluation, was found to be normal.
On laboratory evaluation, complete blood count, differential counts, liver function tests, renal function tests were all within normal limits. Serum immunoglobulin E was found to be marginally raised, and the serum was positive for anti-hepatitis C virus antibodies. The serology for antibodies against human immunodeficiency virus (HIV) was negative. Fungal culture done on one of the excised nodules did not show any growth. Histopathological examination of the excised nodule showed angioproliferative cells with prominent fibrosis, lymphocytic infiltrates and extravasation [Figure - 2]. Special stains revealed the infiltrate to be predominantly of T-cell type [Figure - 3].
Discussion
Angiolymphoid hyperplasia with eosinophilia (ALHE) was originally described by Wells and Whimster [1] in 1969. They considered the process to be a late stage of Kimura′s disease, a disorder described in the Japanese literature 20 years earlier. [2] Wells and Whimster themselves were the ones who first linked ALHE to Kimura′s disease, a view that has been considered valid until recently. Currently, however, most authors believe that ALHE and Kimura′s disease are two separate entities. [3],[4] To further complicate the issue, ALHE has been described with different names by different authors, including atypical pyogenic granuloma, pseudopyogenic granuloma, inflammatory angiomatous nodule, papular angioplasia, inflammatory arteriovenous hemangioma, intravenous atypical vascular proliferation, cutaneous histiocytoid hemangioma and epithelioid hemangioma. It has been recently classified under cutaneous vascular hyperplasias, along with pyogenic granuloma and bacillary angiomatosis.
It is an uncommon benign but potentially disfiguring vascular proliferation. It has a particular predilection for head and neck area, especially for the ears. It is most commonly seen in women in their third to fourth decade. The condition presents with erythematous or skin-colored dome-shaped dermal papules or nodules. It is often associated with spontaneous bleeding, pain, pulsation, pruritus and growth. Eosinophilia is only present in 20% of the cases, and lymphadenopathy is uncommon. Extracutaneous involvement is rare. histopathologically, ALHE involves the dermis and/or the subcutaneous tissue. It shows anomalous proliferation of dilated small- to medium-sized blood vessels with a mixed nodular, perivascular inflammatory infiltrate composed of lymphocytes, eosinophils, histiocytes, plasma cells, neutrophils and mast cells. The affected vessels are tubular, elongated or branching and lined by characteristically plump, hobnail endothelial cells, which line and protrude into the lumina of blood vessels, resulting in a characteristic ′tombstone′ appearance. The cause of ALHE is unknown, although trauma and reactive hyperplastic processes have been proposed. [5] Recently, it has been hypothesized that the pathology may represent a T-cell lymphoproliferative disorder of benign or low-grade malignant nature. [6] Also, malignant transformation has been observed in a young patient with ALHE who developed peripheral T-cell lymphoma. [7] Multiple treatment options have been reported to be effective, including curettage and desiccation, cryotherapy, radiotherapy, steroids (oral, topical and intralesional), retinoids, [8] excision and various lasers. [9],[10],[11] Some cases of spontaneous healing have also been reported.
Kimura′s disease is a rare chronic inflammatory disorder of unknown etiology. [12] It usually presents as a deep, subcutaneous mass in the head and neck region and is frequently associated with regional lymphadenopathy or salivary gland involvement. [13] The disease was first described in Chinese literature as ′eosinophilic hyperplastic lymphogranuloma′ [14] but became widely known as Kimura′s disease after Kimura et al. reported similar cases under the title ′On the unusual granulation combined with hyperplastic changes of lymphatic tissue.′ [2] The condition is apparently more prevalent among Orientals. [15] The rare occurrence of genuine Kimura′s disease in western countries probably caused the current confusion between Kimura′s disease and ALHE, evident in western literature. In fact, the terms have been frequently used synonymously. [16],[17],[18],[19] Rosai et al. [20] were the first to note that Kimura′s disease is different from ALHE. After reviewing the literature, we have gathered characteristic differentiating points between the two diseases and have listed these in [Table - 1].
The association of hepatitis C virus with ALHE has not been described in the literature so far. The exact etiology of ALHE is unclear, with opinions varying between a benign vascular neoplasm to a reactive inflammatory lesion in the form of an atopic reaction to various agents and trauma. Also, in the past there have been reports of association of HHV 8 with ALHE. Hence we thought that anti-HCV antibody positivity may be of some relevance. However, because of the absence of any history suggestive of hepatitis, the chances of it being just a coincidental finding cannot be ruled out. This also seems more likely keeping in view the high incidence of anti-HCV positivity in the general population in this part of the world. But we still feel that this association needs to be highlighted and further evaluated so as to prove or disprove any relevance of anti-HCV antibody positivity in the cases of ALHE, especially from other parts of the world.
The term ′eosinophilia′ is commonly used to indicate raised levels of eosinophils in blood. Moreover, increased level of eosinophils in blood is a feature seen in Kimura′s disease, rather than in ALHE. The occurrence of raised blood eosinophil levels in cases of ALHE is uncommon, and not more than 20% of cases of ALHE have raised levels of eosinophils in the blood. Hence we support the view of Ackerman and colleagues that the term eosinophilia in ALHE may not be correct and may rather confuse the physician at its face value. [21] However, the presence of eosinophils on histopathology is a characteristic feature of this entity and needs to be highlighted. In that case, it would be best to call it ′angiolymphoid hyperplasia with eosinophils.′ It would not only highlight the presence of eosinophils on histopathological examination of this entity but also remove the confusion and wrong impression created by raised blood eosinophils count, as reflected by including the term ′eosinophilia′ in the description of the disease entity. At the same time, the well-accepted abbreviation for this entity would still remain the same.
| 1. |
Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969;81:1-15.
[Google Scholar]
|
| 2. |
Kimura T, Yoshimura S, Ishikawa E. Abnormal granuloma with proliferation of lymphoid tissue. Trans Soc Pathol Jpn 1948;37:179-80.
[Google Scholar]
|
| 3. |
Googe PB, Harris NL, Mihm MC Jr. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: Two distinct histopathological entities. J Cutan Pathol 1987;14:263-71.
[Google Scholar]
|
| 4. |
Kung IT, Gibson JB, Bannatyne PM. Kimura's disease: A clinicopathological study of 21 cases and its distinction from angiolymphoid hyperplasia with eosinophilia. Pathol 1984;16:39-44.
[Google Scholar]
|
| 5. |
Chung TH, Kim DK, Yoon MS, Yang WI. Angiolymphoid hyperplasia with eosinophilia showing characteristics of Kimura's disease. J Dermatol 2000;27:27-30.
[Google Scholar]
|
| 6. |
Kempf W, Haeffner AC, Zepter K, Sander CA, Flaig MJ, Mueller B, et al . Angiolymphoid hyperplasia with eosinophilia: Evidence for a T-cell lymphoproliferative origin. Hum Pathol 2002;33:1023-9.
[Google Scholar]
|
| 7. |
Andreae J, Galle C, Magdorf K, Staab D, Meyer L, Goldman M, et al . Severe atherosclerosis of the aorta and development of peripheral T-cell lymphoma in an adolescent with angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 2005;152:1033-8.
[Google Scholar]
|
| 8. |
El Sayed F, Dhaybi R, Ammoury A, Chababi M. Angiolymphoid hyperplasia with eosinophilia: Efficacy of isotretinoin? Head Face Med 2006;2:32-6.
[Google Scholar]
|
| 9. |
Abrahamson TG, Davis DA. Angiolymphoid hyperplasia with eosinophilia responsive to pulsed dye laser. J Am Acad Dermatol 2003;49:S195-6.
[Google Scholar]
|
| 10. |
Hobbs ER, Bailin PL, Ratz JL, Yarbrough CL. Treatment of angiolymphoid hyperplasia of the external ear with carbon dioxide laser. J Am Acad Dermatol 1988;19:345-9.
[Google Scholar]
|
| 11. |
Papadavid E, Krausz T, Chu AC, Walker NP. Angiolymphoid hyperplasia with eosinophilia successfully treated with flash-lamp pulsed dye laser. Br J Dermatol 2000;142:192-4.
[Google Scholar]
|
| 12. |
Ioachim H, Ratech H. Kimura lymphadenopathy. In : Ioachim H, Ratech H, editors. Ioachim's lymph node pathology. 3 rd ed. Philadelphia: Lipincott-Raven; 2002. p. 209-11.
rd ed. Philadelphia: Lipincott-Raven; 2002. p. 209-11.'>[Google Scholar]
|
| 13. |
Chun SI, Ji HG. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: Clinical and histopathological differences. J Am Acad Dermatol 1992;27:954-8.
[Google Scholar]
|
| 14. |
Kung IT, Chan JK. Kimura's disease or Kimm's disease? Am J Surg Pathol 1988;12:804-5.
[Google Scholar]
|
| 15. |
Chang TL, Chen CY. Eosinophilic granuloma of lymph node and soft tissues. Report of 21 cases. Chin Med J 1962;81:384-7.
[Google Scholar]
|
| 16. |
Buchner A, Silverman S Jr, Wara WM, Hansen LS. Angiolymphoid hyperplasia with eosinophilia (Kimura's disease). Oral Surg Oral Med Oral Pathol 1980;49:309-13.
[Google Scholar]
|
| 17. |
Eisenberg E, Lowlicht R. Angiolymphoid hyperplasia with eosinophils: A clinicopathological conference. J Oral Pathol 1985;14:216-23.
[Google Scholar]
|
| 18. |
Kim BH, Sithian N, Cucolo GF. Subcutaneous angiolymphoid hyperplasia (Kimura disease). Report of a case. Arch Surg 1975;110:1246-8.
[Google Scholar]
|
| 19. |
Reed RJ, Terazakis N. Subcutaneous angioblastic lymphoid hyperplasia with eosinophilia (Kimura's disease). Cancer 1972;29:489-97.
[Google Scholar]
|
| 20. |
Rosai J, Gold J, Landy R. The histiocytoid hemangiomas: A unifying concept embracing several previously described entities of the skin, soft tissue, large vessel, bone and heart. Hum Pathol 1979;10:707-30.
[Google Scholar]
|
| 21. |
Ackerman AB, Kerl H, Sαnchez J, Guo Y, Hofer A, Kelly P, et al. A Clinical Atlas of 101 Common Skin Diseases. New York: Ardor Scribendi, Ltd. 2000.
[Google Scholar]
|
Fulltext Views
1,160
PDF downloads
1,186





