Translate this page into:
Angiosarcoma of the gingiva: Metastasis from a primary tumor of the scalp
2 Department of Medical Oncology, The Second People's Hospital of Sichuan, Chengdu, PR China
3 Department of Periodontology, West China Hospital of Stomatology, Sichuan University, Chengdu, PR China
4 State Key Laboratory of Oral Diseases, West China School of Stomatology, Sichuan University, Chengdu; Department of Periodontology, West China Hospital of Stomatology, Chengdu, PR China
Correspondence Address:
Yi Xu
Department of Periodontology, West China School of Stomatology, Sichuan University, No. 14, Section 3, Renmin Nan Road, Chengdu 610041
PR China
| How to cite this article: Yang J, Mei K, Wu C, Wu Y, Xu Y. Angiosarcoma of the gingiva: Metastasis from a primary tumor of the scalp. Indian J Dermatol Venereol Leprol 2017;83:626 |
Sir,
Angiosarcoma is a rare malignant sarcoma of endothelial origin that is further classified as hemangiosarcoma or lymphosarcoma depending on whether it derives from vascular or lymphatic channels. Angiosarcomas are reported to account for approximately 2% of all soft-tissue sarcomas.[1] Compared to other sarcomas, angiosarcomas have a predilection for the skin and soft tissues, particularly on the head. However, primary tumors arising in the oral cavity and salivary gland areas account for only 1% of all angiosarcomas.[2] Here, we report a patient with metastatic angiosarcoma of the gingiva from a primary scalp lesion.
A 61-year-old man of Chinese origin was referred for a neoplasm on the gingival papilla between the left central and lateral incisors that had been detected 10 days earlier. He had a history of premature ventricular beats but no history of previous oral surgery, radiation or industrial chemical exposure. Intraoral examination revealed a well-defined 7 mm × 7 mm protruding mass on the buccal side [Figure 1a] and a 6 mm × 6 mm mass on the palatal side of the gingival papilla [Figure 1b] with local tenderness on the tissue. The surrounding soft tissues were normal without swelling or pain. The tumor was immobile. On clinical examination, epulis and other inflammatory hyperplasias were considered as differential diagnoses. Alveolar bone resorption was evident on radiographic examination [Figure 1c]. Four months before he had been treated surgically for a primary angiosarcoma of the scalp by extensive resection and locoregional flap reconstruction. Physical examination revealed granulation tissue along the areas of surgical excision, on the scalp and skull [Figure - 2]. The patient refused further positron emission tomography evaluation as it was not covered by medical insurance. He had also not undertaken chemotherapy and radiotherapy for personal reasons.
 |
| Figure 1a: Frontal intra-oral view shows a neoplasm between the central and lateral incisor teeth |
 |
| Figure 1b: Grossly swollen mass on the palatal gingival papilla |
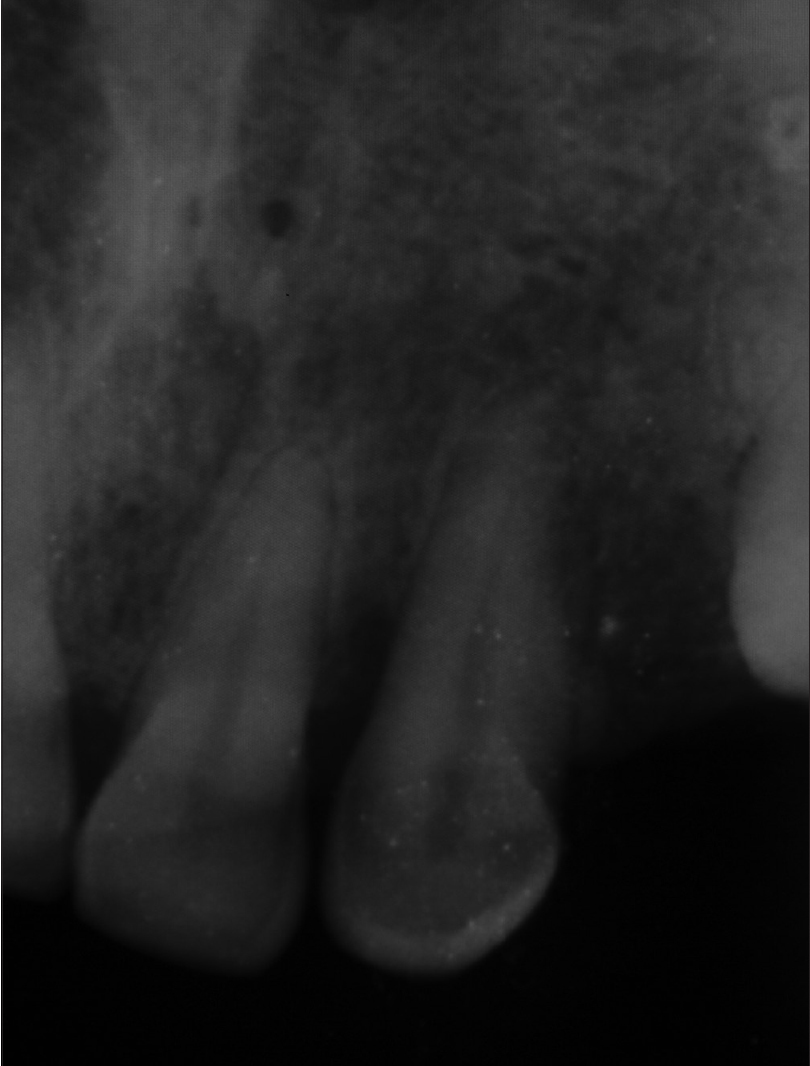 |
| Figure 1c: Radiographic examination shows alveolar bone resorption between the central and lateral incisors |
 |
| Figure 2: The site of previous resection of the scalp angiosarcoma, with areas of the scalp and skull removed |
Biopsy from the gingival lesion revealed an infiltrative tumor composed of abundant proliferating pleomorphic cells with hyperchromatic nuclei as well as vasoformative features viz., primitive vascular spaces filled with erythrocytes. A spindle cell or sarcomatoid cell population with atypical mitotic activity was also seen within the tumor [Figure - 3]. On immunohistochemistry, strong positive staining for CD31, CD34, D2-40 and erythroblast transformation-specific-related gene was seen [Figure - 4]. However, Ki-67 expression was low (~10%). Immunohistochemical evaluation of scalp angiosarcoma after radical resection detected positivity for factor VIII-related antigen, CD31, CD34, erythroblast transformation-specific-related gene, vimentin and D2-40 and negativity for pancytokeratins [Figure - 5]. Accordingly, we made a diagnosis of metastatic gingival angiosarcoma.
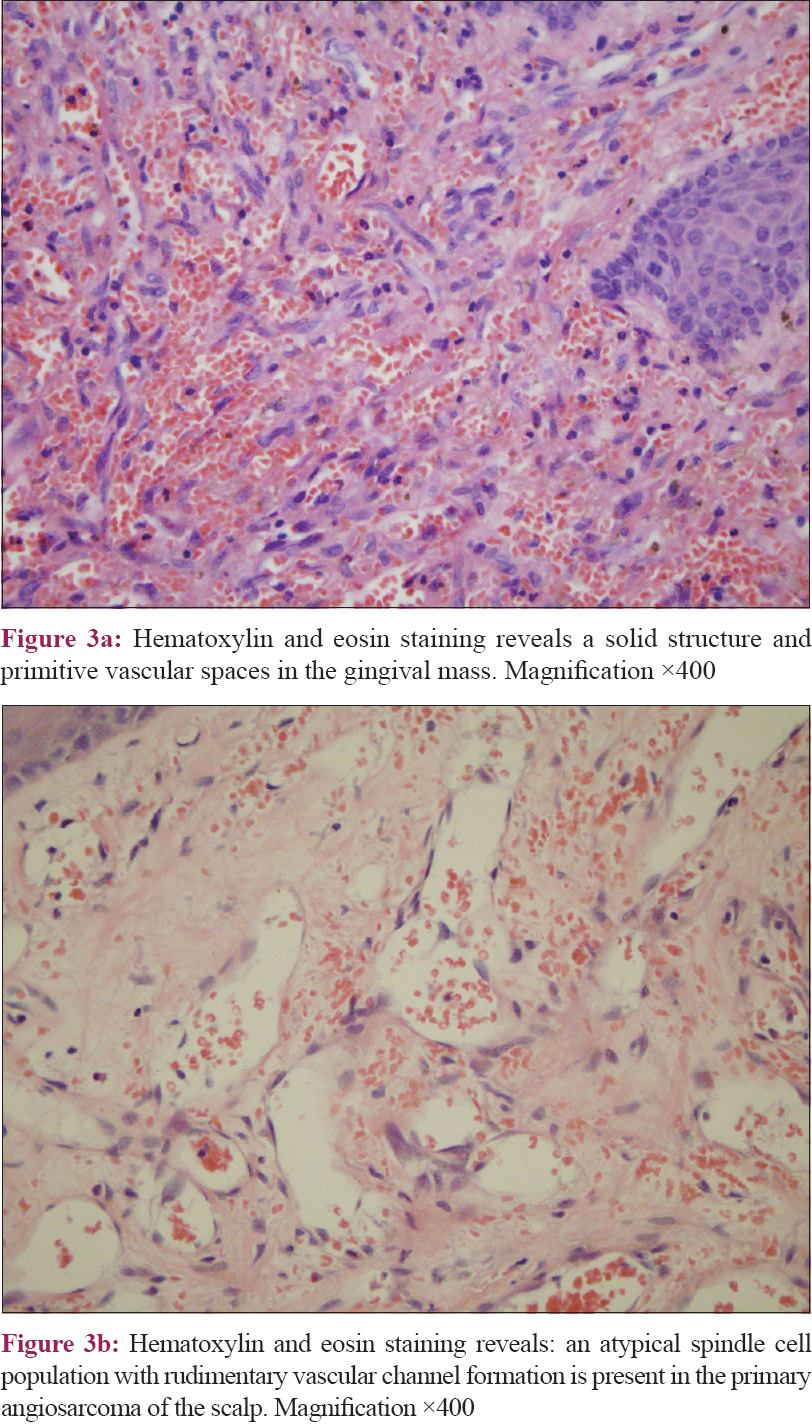 |
| Figure 3 |
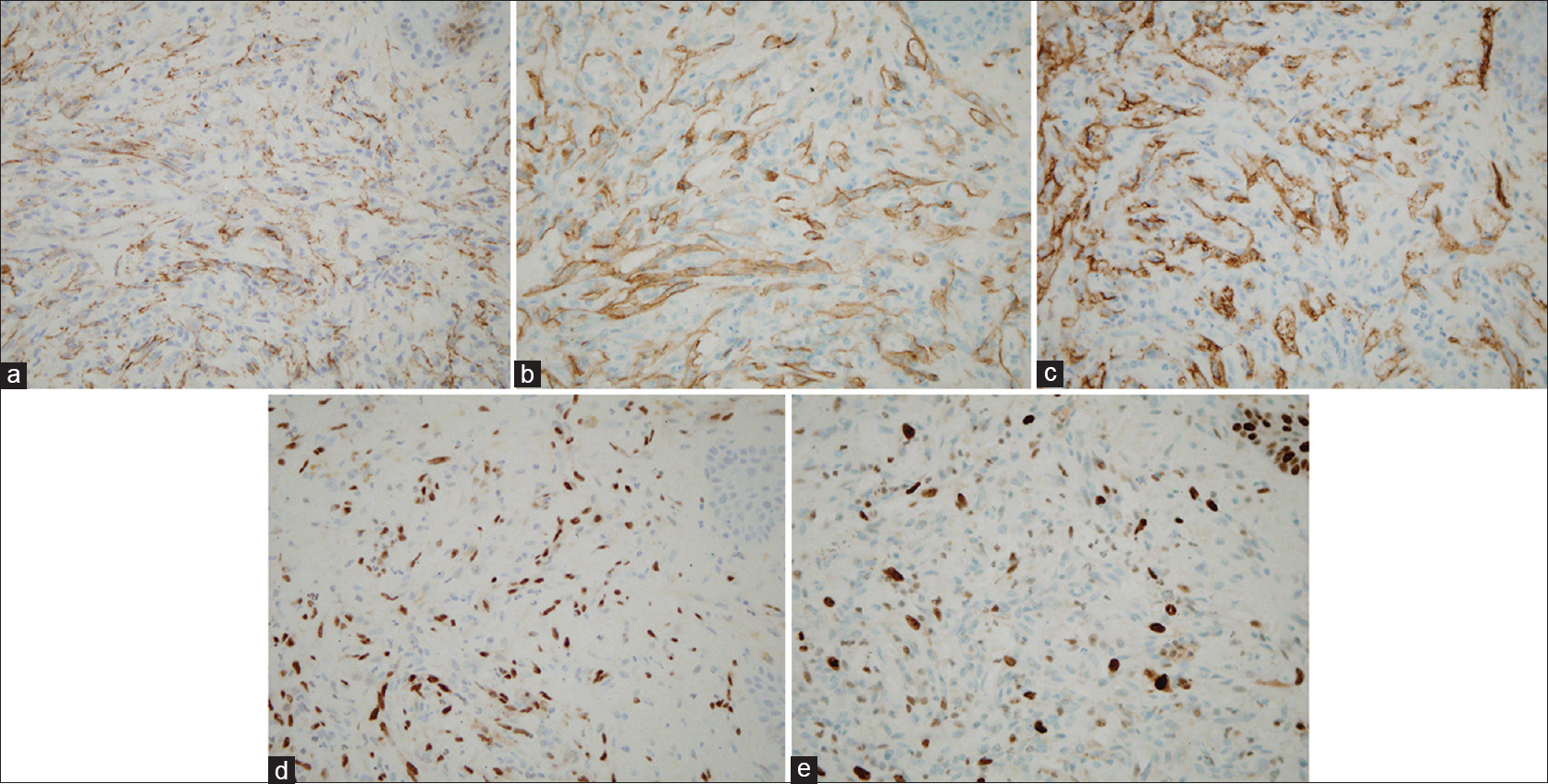 |
| Figure 4: (a) Diffuse immunochemical staining with CD31-positive cells. Magnification ×400. (b) Diffuse immunochemical staining with CD34-positive cells. Magnification ×400. (c) Diffuse immunochemical staining with D2-40-positive cells. Magnification ×400. (d) Diffuse immunochemical staining with ETS-related gene (ERG)-positive cells. Magnification ×400. (e) Diffuse immunochemical staining with Ki67-positive cells. Magnification ×400 |
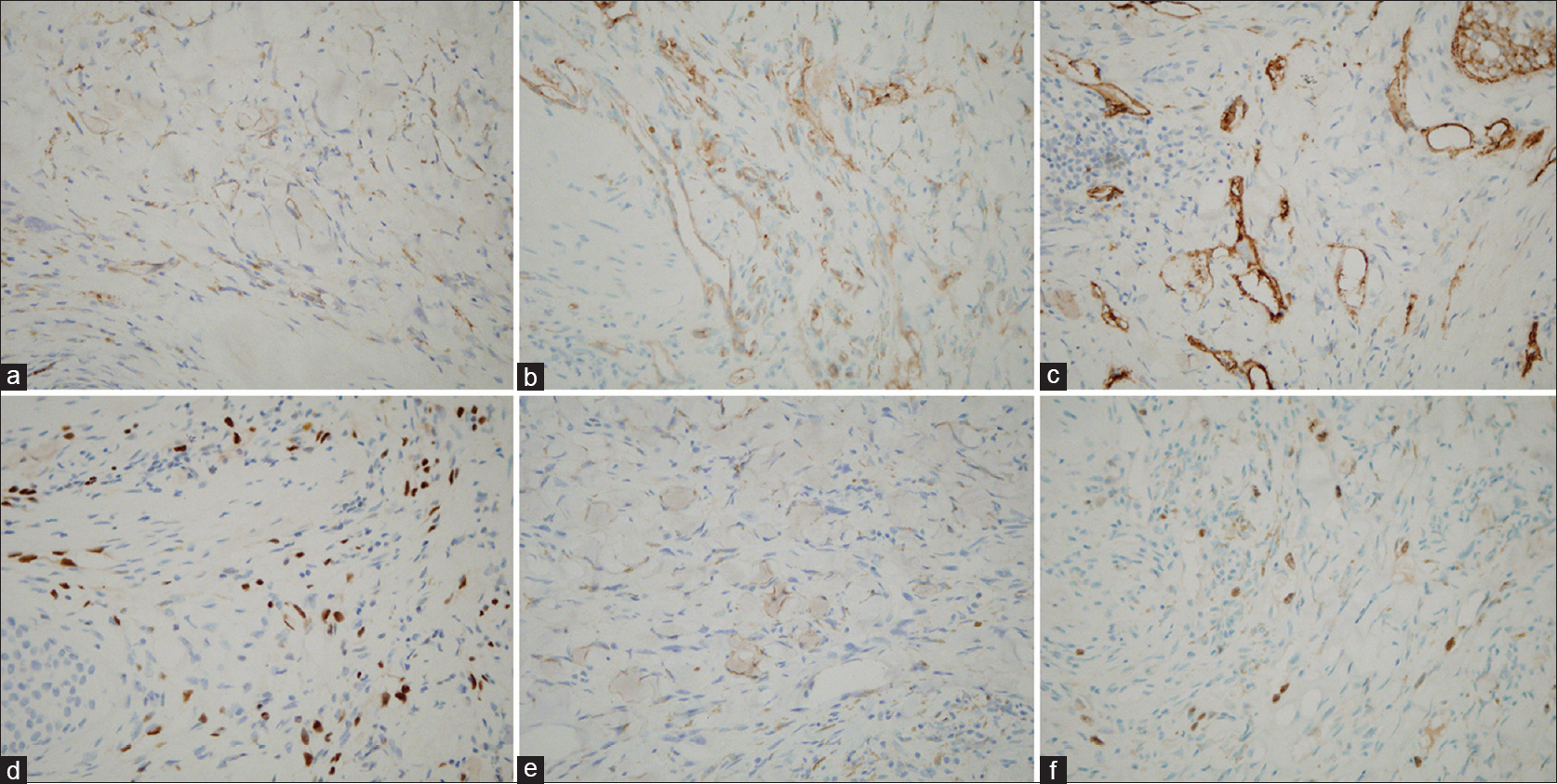 |
| Figure 5: (a) Immunohistochemical features of the primary tumor, with CD31-positive cells. Magnification ×400. (b) Immunohistochemical features of the primary tumor, with CD34-positive cells. Magnification ×400. (c) Immunohistochemical features of the primary tumor, with D2-40-positive cells. Magnification ×400. (d) Immunohistochemical features of the primary tumor, with ETS-related gene (ERG)-positive cells. Magnification ×400. (e) Immunohistochemical features of the primary tumor, with factor VIII-related antigen cells. Magnification ×400 (f) Immunohistochemical features of the primary tumor, with Ki67-positive (~10%) cells. Magnification ×400 |
After radical excision of the gingival angiosarcoma, the patient received chemotherapy 16 days later. The chemotherapy regimen comprised two cycles of isophosphamide, etoposide and bevacizumab. Unfortunately, the tumor progressed and metastasized to the sternum 1 month later. No evidence of regional node involvement or lung metastasis was found. The patient underwent a switch to cisplatin plus docetaxel therapy, but he subsequently declined further treatment.
Angiosarcomas are very aggressive tumors. Scalp lesions most commonly metastasize to the lungs, followed by the liver, cervical lymph nodes, spleen and rarely the heart and brain.[3] Some cases of scalp angiosarcoma with metastasis to the gingiva have previously been reported. The early manifestation of gingival angiosarcoma, a tender, exophytic lesion that is usually hemorrhagic, resembles a hyperplastic or reactive lesion such as a pyogenic granuloma, vascular epulis or peripheral giant cell granuloma. Furthermore, the histological features of angiosarcomas vary from a well-differentiated neoplasm with an anastomosing vascular system to a poorly differentiated tumor without vasoformative activity.[4] Therefore, early biopsy with immunohistochemistry is mandatory for the differentiation of an angiosarcoma from other neoplasms with similar morphologies. The tumor is positive for CD31, CD34 and factor VIII. In the present case, the positive expression of factor VIII-related antigen, a tissue-specific marker for endothelial cells, as well as the lack of pancytokeratins, helped us confirm the endothelial nature of this sarcomatous proliferation. The expression of vimentin also excluded the possibility of a poorly differentiated squamous cell carcinoma with a pseudoangiosarcomatous pattern.[4] In addition, the detection of erythroblast transformation-specific-related gene further supports our diagnosis of cutaneous angiosarcoma; this is particularly seen in poorly differentiated cases.[5]
Although the oral cavity is not a common site for metastases and the morphology of a gingival angiosarcoma is similar to that of an epulis or other inflammatory diseases, the patient's history together with histological and immunochemical analyses helped us confirm the diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lu HJ, Chen PC, Yen CC, Hsiao FC, Tzeng CH, Ma H, et al. Refractory cutaneous angiosarcoma successfully treated with sunitinib. Br J Dermatol 2013;169:204-6.
[Google Scholar]
|
| 2. |
Nagata M, Yoshitake Y, Nakayama H, Yoshida R, Kawahara K, Nakagawa Y, et al. Angiosarcoma of the oral cavity: A clinicopathological study and a review of the literature. Int J Oral Maxillofac Surg 2014;43:917-23.
[Google Scholar]
|
| 3. |
Morgan MB, Swann M, Somach S, Eng W, Smoller B. Cutaneous angiosarcoma: A case series with prognostic correlation. J Am Acad Dermatol 2004;50:867-74.
[Google Scholar]
|
| 4. |
Guarda LA, Ordonez NG, Smith JL Jr., Hanssen G. Immunoperoxidase localization of factor VIII in angiosarcomas. Arch Pathol Lab Med 1982;106:515-6.
[Google Scholar]
|
| 5. |
McKay KM, Doyle LA, Lazar AJ, Hornick JL. Expression of ERG, an Ets family transcription factor, distinguishes cutaneous angiosarcoma from histological mimics. Histopathology 2012;61:989-91.
[Google Scholar]
|
Fulltext Views
3,516
PDF downloads
2,209





