Translate this page into:
Angiospastic macules of Bier: A cause of mottled skin
Correspondence Address:
Jorge Ocampo-Candiani
Department of Dermatology, “Dr. José E. González” University Hospital of the School of Medicine of the “Universidad Autónoma de Nuevo León,” Monterrey 64610
Mexico
| How to cite this article: Villarreal-Villarreal CD, Robles-Mendez JC, Guerra-Vazquez AE, Ocampo-Candiani J. Angiospastic macules of Bier: A cause of mottled skin. Indian J Dermatol Venereol Leprol 2018;84:645 |
Sir,
A 12-year-old girl with no past relevant medical history was referred to our Department of Dermatology at the university hospital “Dr. José E. González” Monterrey, México, with a 5-month history of asymptomatic white spots on her limbs which were first noticed on her legs and later on her arms. She recalled exercise and standing for a long time as triggering factors. The patient gave a history of malar erythema exacerbated with sun exposure and arthralgias of her knees. On physical exploration, oral ulcers and scarring alopecia were absent and she denied systemic symptoms, such as tachycardia, fever, weight loss and malaise.
Dermatologic examination revealed irregular hypopigmented macules surrounded by blanching diffuse erythema which were accentuated on orthostasis. The lesions disappeared when the limbs were raised and by applying pressure [Figure - 1] and [Figure - 2].
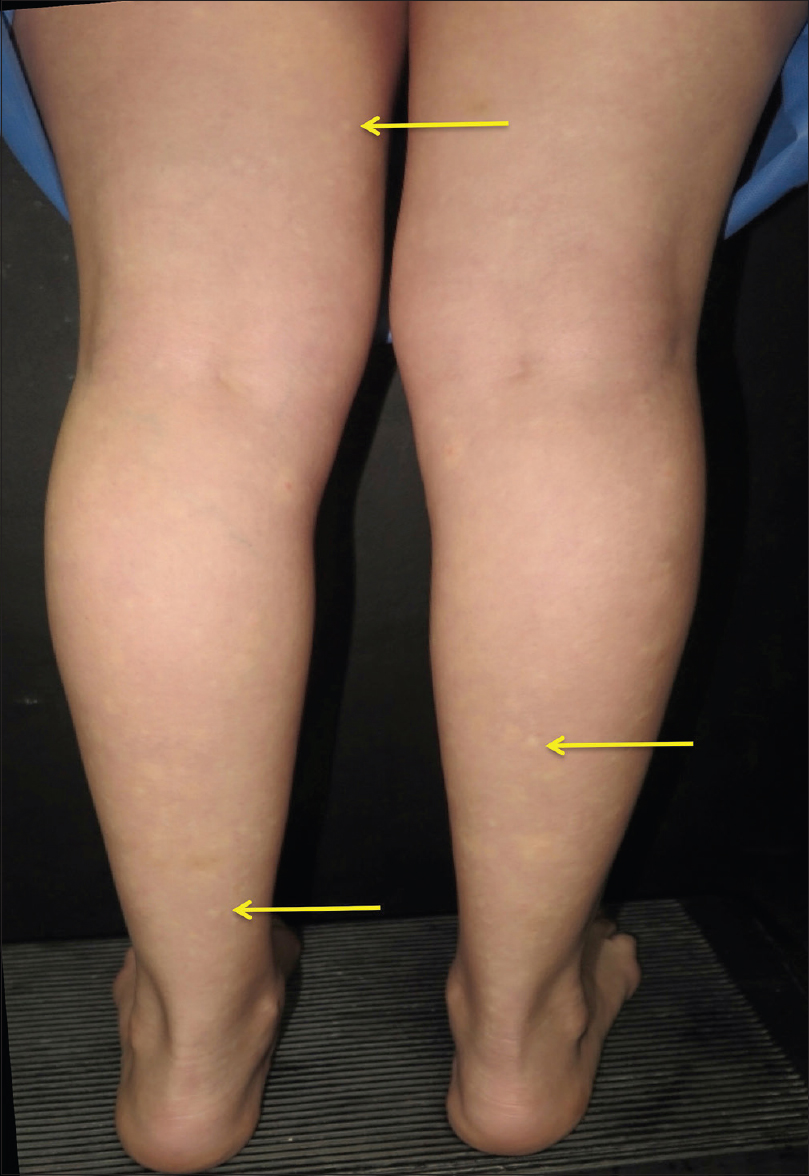 |
| Figure 1: Irregular hypopigmented macules with bilateral distribution, surrounded by diffuse erythema on lower extremities |
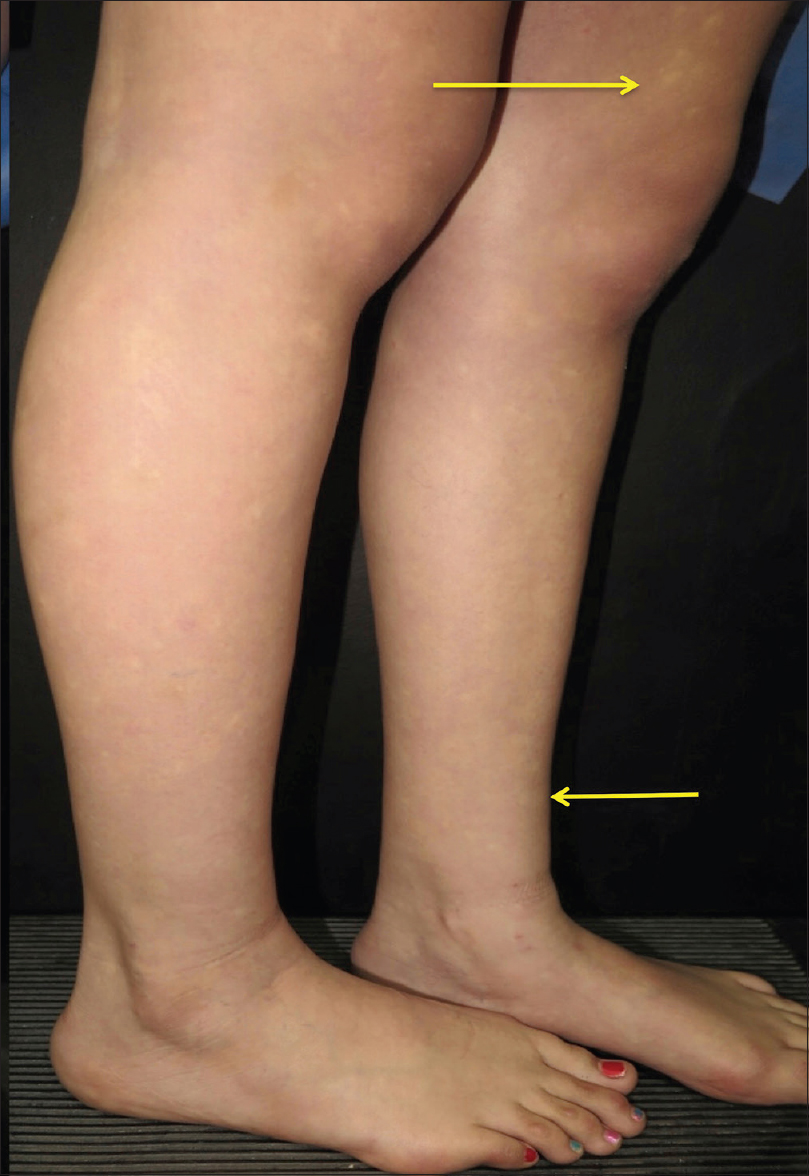 |
| Figure 2: Lateral view of the patients lower extremities. Hypopigmented macules are noticed, giving the appearance of mottled skin |
Skin biopsy with hematoxylin and eosin stain showed papillary dermal edema and dilated capillaries. Routine laboratory tests, including a complete blood count, blood chemistry including double-stranded deoxyribonucleic acid, Coombs test, C3, C4 and urine test, were within normal range. Although antinuclear antibodies were positive(1:160), the patient did not fulfill the criteria of systemic lupus erythematosus. Diagnosis of idiopathic Bier spots was made based on the patient's clinical features. The patient did not undergo treatment.
Angiospastic macules, speckled mottling of the limbs or Bier spots, received their name from the German surgeon Dr. Augustus Bier, who in 1898 described this entity by making a vascular experiment. He applied a tourniquet and occluded the blood supply of the arm. Bier spots were induced and disappeared once the blood supply was restored.
Bier spots are an abnormal and transient vascular response that occur with vasodilatation and vasoconstriction. They are mostly reported in patients between 20 and 40 years (range, 15–75 years of age) of age and men outnumber women with a 2:1 ratio.[1] It is proposed that an exaggerated vasospastic response occurs secondary to venous hypertension, arterial constriction or a lack of blood supply. Usually reported triggers are changes of position of the extremities (orthostasis) or cooler environments and hypoxia.[2]
Clinically, Bier spots are recognized as asymptomatic, multiple, small (5–10 mm) hypochromic macules with irregular shape and distribution, surrounded by blanching diffuse erythema. They are commonly seen on the extensor surface of extremities and even sometimes in a generalized distribution.[1] Diagnosis can be made easily through physical examination as these pale macules appear with orthostatic position and typically, they disappear by applying pressure on the surrounding skin or with elevation of the limbs, as was in our case.
Differential diagnoses include hypopigmentation disorders such as vitiligo, pityriasis versicolor, postinflammatory hypopigmentation and nevus depigmentosus which do not disappear neither by applying pressure nor elevating the extremities, as well as nevus anemicus which is a congenital and permanent vascular anomaly that usually appears on the trunk. All of these were ruled out by physical examination.[3]
Bier spots typically show no abnormalities on laboratory tests or skin biopsy. Although patients are usually healthy, it has been reported in different conditions, such as pregnancy, scleroderma, aortic hypoplasia and coarctation, as well as in autoimmune diseases, such as alopecia areata, lichen planus and cryoglobulinemia.[1] It is important to remember that, although positive (1:160) anti - nuclear antibody can be positive in upto 5% of general population, antinuclear antibody may develop years, if not decades, before the symptoms of autoimmune disease.[4],[5] After1-year follow-up, our patient had neither fulfilled the diagnostic criteria of systemic lupus erythematosus nor developed any systemic signs of autoimmune diseases.
Limitations in our article are that we only presented one patient with a short follow-up course (1 year). Another limitation is the fact that information about this entity is scarce as it is seldom reported and only some articles about this entity exist limiting our pool of references.
In conclusion, Bier spots represent an idiopathic and benign entity in the majority of cases and treatment is not needed as they tend to resolve spontaneously. Nevertheless, in some cases, systemic disease should be ruled out since they could be the first sign of a systemic disease. Reassuring the patient of the physiological and benign nature of this entity is the mainstay of treatment.
Acknowledgment
We thank Dr. Sergio Lozano for the review of this article.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Fan YM, Yang YP, Li W, Li SF. Bier spots: Six case reports. J Am AcadDermatol 2009;61:e11-2.
[Google Scholar]
|
| 2. |
Peyrot I, Boulinguez S, Sparsa A, Le Meur Y, Bonnetblanc JM, Bedane C. Bier's white spots associated with scleroderma renal crisis. ClinExpDermatol 2007;32:165-7.
[Google Scholar]
|
| 3. |
Cabanillas M, Suárez-Amor O, Loureiro M, Ginarte M, Toribio J. Bier's spots in association with hypoplasia of the aorta. Dermatology 2007;215:166-7.
[Google Scholar]
|
| 4. |
Arbuckle MR, McClain MT, Rubertone MV, Scofield RH, Dennis GJ, James JA, et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med 2003;349:1526-33.
[Google Scholar]
|
| 5. |
Mahler M, Ngo JT, Schulte-Pelkum J, Luettich T, Fritzler MJ. Limited reliability of the indirect immunofluorescence technique for the detection of anti-Rib-P antibodies. Arthritis Res Ther 2008;10:R131.
[Google Scholar]
|
Fulltext Views
9,572
PDF downloads
2,904





