Translate this page into:
Annular epidermolytic ichthyosis: A rare phenotypic variant of bullous congenital ichthyosiform erythroderma
2 Department of Pathology, Indian Council of Medical Research, Safdarjung Hospital, New Delhi, India
Correspondence Address:
V Ramesh
Department of Dermatology and STD, 5th Floor, OPD block, VM Medical College and Safdarjung Hospital, New Delhi - 110 029
India
| How to cite this article: Jha A, Taneja J, Ramesh V, Singh A. Annular epidermolytic ichthyosis: A rare phenotypic variant of bullous congenital ichthyosiform erythroderma. Indian J Dermatol Venereol Leprol 2015;81:194-197 |
Sir,
Bullous congenital ichthyosiform erythroderma of Brocq is a rare mechanobullous eruption first described by Brocq in 1902. This autosomal dominant disorder is characterized by blistering and erythroderma in early life with many similarities to epidermolysis bullosa simplex. However, these patients subsequently develop ichthyosis and hyperkeratosis. Epidermolytic hyperkeratosis is the hallmark feature on light and electron microscopy. Annular epidermolytic ichthyosis is a distinct phenotypic variant of bullous congenital ichthyosiform erythroderma characterized by intermittent development of polycyclic, erythematous, scaly plaques on the trunk and proximal extremities. [1] Histological features are similar to those of classical epidermolytic hyperkeratosis, and keratin K10 or K1 mutations, similar to those of bullous congenital ichthyosiform erythroderma, have been identified in annular epidermolytic ichthyosis. [2],[3],[4]
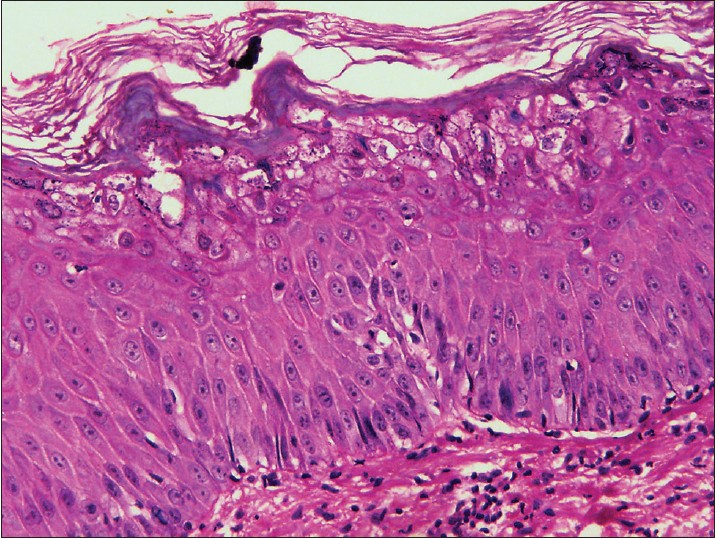
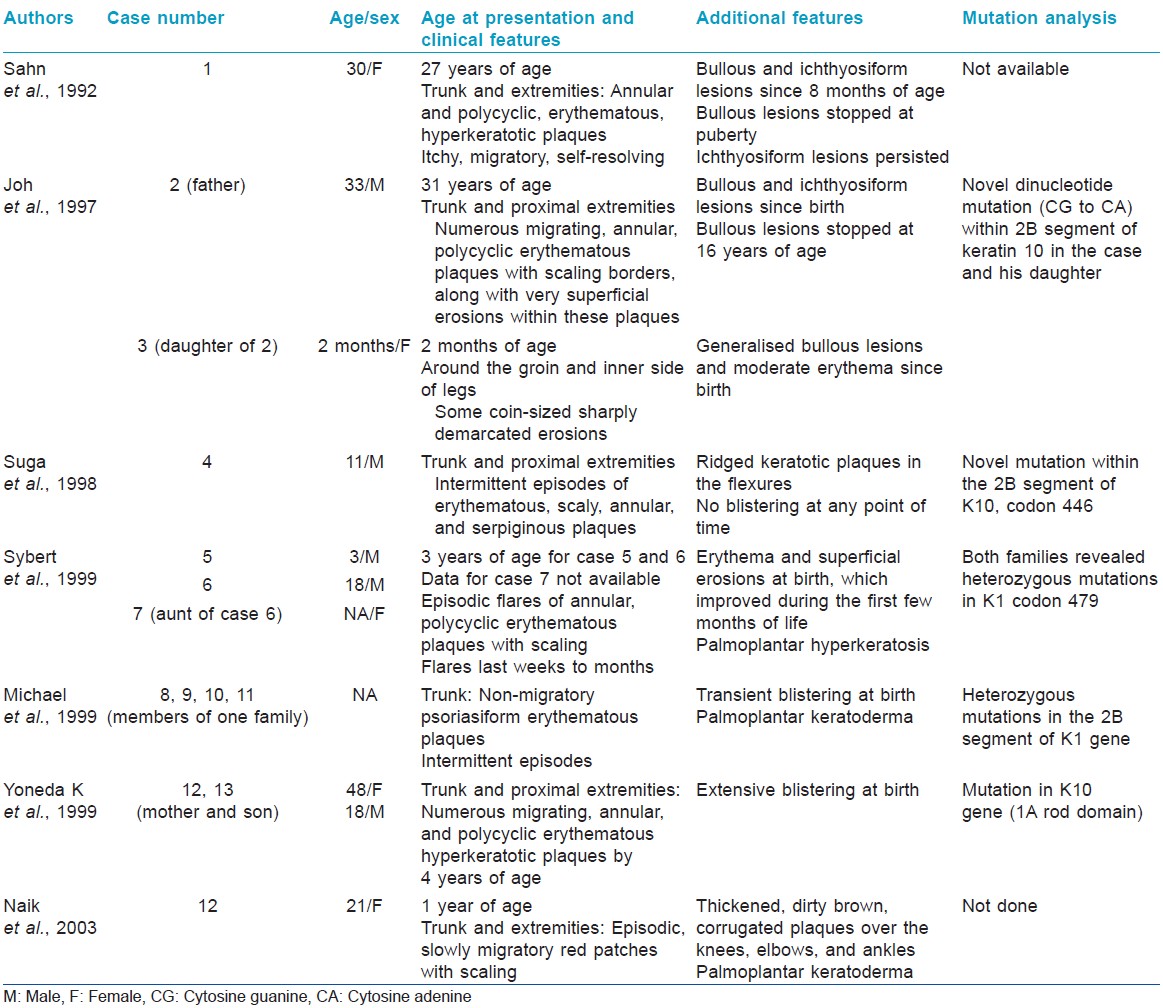
A 26-year-old female, born of a non-consanguineous marriage, presented to the dermatology outpatient of Vardhaman Mahavir Medical College and Safdarjung Hospital, New Delhi, India, with a history of generalized recurrent blistering since birth. She had begun to develop hyperkeratotic plaques all over the body since early infancy and by 8 years of age, the lesions had cleared from most areas and had localized to the flexures (neck, cubital fossae, elbows, and wrist) [Figure - 1]a. For the past 3 years, she was also developing recurrent episodes of erythematous annular plaques with scaling over the trunk, thighs, and inframammary areas. These lesions increased in size over a period of 8-10 days and later developed peripheral desquamation giving them an annular appearance [Figure - 2]a and b. She had given birth to a boy with erythroderma with subsequent development of rippled hyperkeratosis of the flexures [Figure - 3]a and b. There was no history of neonatal blistering in the child. Examination of the child revealed polycyclic, psoriasiform, scaly plaques on the trunk and extremities. Clinically, the hair, teeth, and nails were normal. With the provisional differential diagnoses of bullous congenital ichthyosiform erythroderma (BCIE) occurring alone, in combination with erythrokeratoderma, or in combination with with psoriasis, a skin biopsy was taken from the annular plaque and a hyperkeratotic lesion that represented the two main clinical aspects of the disease. Light microscopy of the specimens revealed hyperkeratosis, acanthosis, and degeneration of granular layer with dispersion of keratohyalin granules. Vacuolar changes were evident in the keratinocytes of the stratum spinosum [Figure - 4]. These findings were consistent with the diagnosis of epidermolytic hyperkeratosis. A complete blood count, liver and kidney function tests, and serum electrolytes were normal. Skin scrapings from the scaly plaques were negative for fungi.
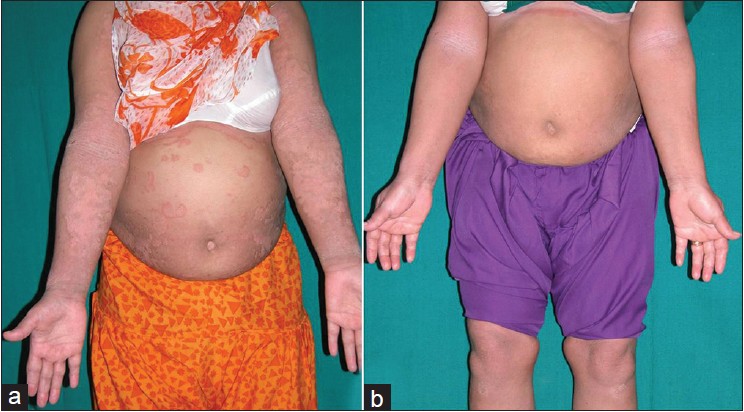 |
| Figure 1: (a) Annular psoriasiform plaques over the trunk and extremities and ribbed hyperkeratosis over the flexures. (b) Considerable improvement after treatment with acitretin |
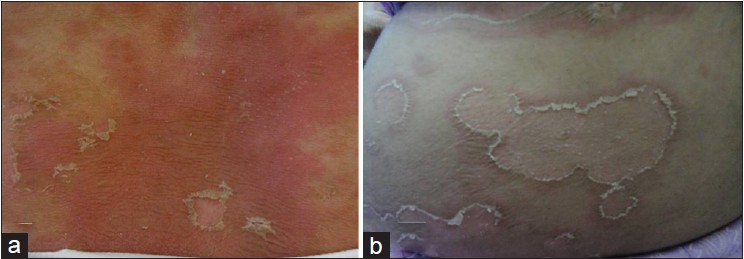 |
| Figure 2: (a) Erythematous polycyclic plaques over the trunk with exfoliation starting from the center. (b) Exfoliation extending toward the periphery giving an annular appearance |
 |
| Figure 3: (a) Diffuse erythema and creamy white scaling in the child. (b) Peeling of the skin over the soles in the child |
 |
| Figure 4: Hyperkeratosis, epidermal acanthosis with granular layer degeneration and vacoular alteration in keratinocytes (H and E, ×400) |
She was initially started on emollients and ciclosporin 3.5 mg/kg body weight because of the presumptive differential diagnosis of psoriasis for the annular plaques. Retinoids were not considered at this point because she was breastfeeding. The erythematous, annular plaques improved moderately after 6 weeks of treatment. The plaques remained stable for 1 month after which she had a flare of the annular plaques. She was then started on acitretin 0.5 mg/kg/day after detailed counselling regarding contraception. Four weeks later, all the annular plaques disappeared and there was a remarkable improvement in the flexural as well as the annular plaques [Figure - 1]b. No recurrence was noted after 2 months. We plan to re-institute acitretin in the event of a relapse. The child was treated with emollients in view of the milder phenotype and the potential side effect profile of acitretin.
The distinct phenotype seen in our patient has only been described in eight families thus far in the literature and we were unable to find any previous cases reported from India [Table - 1]. It was first reported in a young female by Sahn et al. in 1992 who also coined the term annular epidermolytic ichthyosis. [1] She had bullous and ichthyosiform skin lesions since the age of 8 months. Later, she developed numerous annular and polycyclic, erythematous, hyperkeratotic plaques on the trunk and extremities, which were pruritic, enlarged slowly, and then resolved. Histopathology of the annular plaques revealed epidermolytic hyperkeratosis. Our case also had a similar presentation. Subsequently, Joh et al. reported a similar condition in a family with two generations being affected. Histological examination showed typical features of epidermolytic hyperkeratosis and molecular analysis revealed a novel dinucleotide mutation within the 2B segment of the keratin 10 gene that was passed on to offspring. [2] Similar cases were reported by Suga et al. in 1998 [3] and Sybert et al. in 1999. [4] Molecular analysis of these families revealed mutations in keratin 10 and keratin 1 genes, respectively. Naik reported episodic flares of polycyclic psoriasiform patches in a young woman with a life-long history of palmoplantar keratoderma with histological features of epidermolytic hyperkeratosis. [5]
The molecular mechanisms underlying this particular phenotype of epidermolytic ichthyosis caused by mutations in K1 and K10 are unclear. We were not able to perform the mutation analysis in our patient because the facility was not available in our setting.
| 1. |
Sahn EE, Weimer CE Jr, Garen PD. Annular epidermolytic ichthyosis: A unique phenotype. J Am Acad Dermatol 1992;27:348-55.
[Google Scholar]
|
| 2. |
Joh GY, Traupe H, Metze D, Nashan D, Huber M, Hohl D, et al. A novel dinucleotide mutation in keratin 10 in the annular epidermolytic ichthyosis variant of bullous congenital ichthyosis erythroderma. J Invest Dermatol 1997;108:357-61.
[Google Scholar]
|
| 3. |
Suga Y, Duncan KO, Heald PW, Roop DR. A novel helix termination mutation in keratin 10 in annular epidermolytic ichthyosis, a variant of bullous congenital ichthyosiform erythroderma. J Invest Dermatol 1998;111:1220-3.
[Google Scholar]
|
| 4. |
Sybert VP, Francis JS, Corden LD, Smith LT, Weaver M, Stephens K, et al. Cyclic ichthyosis with epidermolytic hyperkeratosis: A phenotype conferred by mutations in the 2B domain of keratin k1. Am J Hum Genet 1999;64:732-8.
[Google Scholar]
|
| 5. |
Naik NS. Annular epidermolytic ichthyosis. Dermatol Online J 2003;9:4.
[Google Scholar]
|
Fulltext Views
4,688
PDF downloads
1,648





