Translate this page into:
Anti-Mi-2 antibody–associated atypical dermatomyositis with extensive subcutaneous calcinosis
Corresponding author: Dr. Vinayak Viswanath, Department of Dermatology and Venereology, Government Medical College, Medical College PO, Thiruvananthapuram, India. vinayakviswanath21@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Viswanath V, Chandran R, George AE, Nair SS, Varghese SA. Anti-Mi-2 antibody–associated atypical dermatomyositis with extensive subcutaneous calcinosis. Indian J Dermatol Venereol Leprol. 2024;90:508-11. doi: 10.25259/IJDVL_384_2022
Dear Editor,
Calcinosis cutis is frequently found in juvenile dermatomyositis but is uncommon in adults.1 Anti-Mi-2 antibody is typically not linked to calcinosis,2 but rather to pathognomonic skin lesions of dermatomyositis such as Gottron’s sign and Gottron’s papules.3 We report a case of 38-year-old woman, who tested positive for anti-Mi-2 antibodies and developed skin nodules with calcinosis. However, she did not exhibit most of the typical skin manifestations of dermatomyositis usually seen in such cases.
A 38-year-old woman was diagnosed with dermatomyositis twelve years ago based on clinical findings, histopathological findings of skin and muscles, and elevated muscle enzymes. Her autoantibody profile at the time was not recorded. She presented with multiple, firm nodules over the arms, lateral hips and thighs of four years duration. The nodules started over the thighs, gradually enlarged in size, became painful and many exuded a calcium-like white chalky material. She denied any inciting trauma. She had been on low-dose oral prednisolone for twelve years before being started on mycophenolate mofetil 2 gm since the appearance of the skin nodules. She has also been on alendronate 70 mg weekly for one year and on diltiazem 60 mg daily for two months but this failed to prevent the progression of lesions.
Physical examination revealed confluent hyperpigmentation over the face and upper chest with induration of skin over forearms and legs, and multiple hard, hyperpigmented nodules over the arms, thighs, upper chest and iliac crest, some of which exuded chalky white material [Figures 1a and 1b].

- (a) Confluent hyperpigmented macules over the face and sides of the neck, (b) Multiple hyperpigmented nodules over the thigh, with a few showing central openings.
Laboratory studies revealed elevated levels of creatine phosphokinase (660 IU/L), serum aspartate aminotransferase (41 IU/L) and lactate dehydrogenase (691 IU/L). Serum calcium, inorganic phosphate, alkaline phosphatase, calcium-phosphate product (33.8 mg/dL), parathyroid hormone, vitamin D and renal function were all within normal limits. Antinuclear antibody profile was negative. Myositis-specific and associated antibody profile by immunoblot were strongly positive for anti-Mi-2 antibody (+++) and only borderline for anti-MDA5 (anti-melanoma differentiation-associated gene 5) and anti-PM-Scl 70 antibodies.
X-ray of indurated areas and computerized tomography (CT) scan identified symmetrical coarse calcification in the subcutaneous fat overlying the arms, upper chest, abdominal wall, and thighs, as well as diffuse atrophy of latissimus dorsi and gluteus maximus bilaterally with normal intra-abdominal viscera [Figures 2a, 2b and 3a–3c]. Histopathology of nodule showed homogenization of collagen in dermis without interface changes suggestive of scleroderma and calcification of the subcutis with foreign body cell reaction. Fourier transform infrared spectroscopy analysis (FTIR Analysis) of the extruded chalky material showed calcium hydroxyapatite.

- X-ray showing multiple calcifications (white arrows) over the right arm.

- X-ray showing multiple calcifications (white arrows) over both thighs.
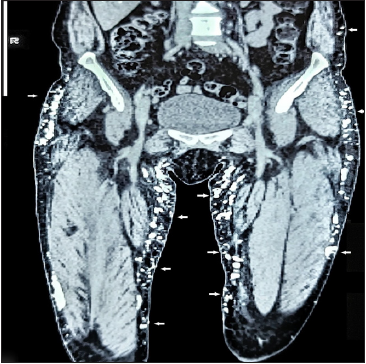
- CT scan: Coronal section showing coarse subcutaneous calcifications in flanks and thighs (white arrows).

- CT scan: Axial section showing calcification (white arrows) in subcutis of upper thighs.
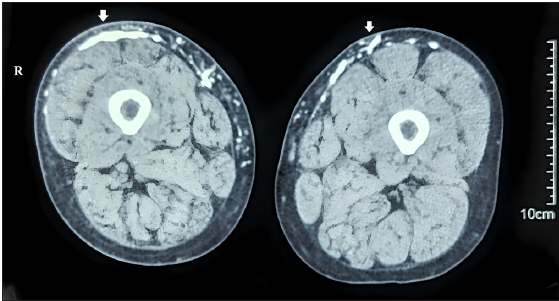
- CT Scan: Axial section showing calcification (white arrows) in subcutis of lower thighs.
Dermatomyositis (DM) is an idiopathic inflammatory myopathy characterized by heliotrope rash, Gottron’s papules, photo-distributed erythema, poikiloderma, periungual telangiectasia, and alopecia.1 Calcinosis is a frequent complication of dermatomyositis that affects up to 40% of patients with juvenile dermatomyositis (JDM).1,4 However, with a prevalence of 20%, it is only about half as prevalent as in adults and usually develops later in the course of the disease.2,5
Calcinosis in dermatomyositis can present as small superficial plaques or nodules on the skin and around joints (superficial calcaneal), deeper nodules in the dermis, subcutis or muscles (deep calcaneal), and as deposits along myofascial planes (calcinosis universalis), or as a generalised form covering all surfaces with joint contractures and immobility (exoskeleton).4,6
Calcinosis in adults often presents as firm, yellow or flesh-coloured dermal or subcutaneous papules or nodules over elbows, knees, buttocks and hands (areas of repeated microtrauma). Calcinosis associated with dermatomyositis is most commonly found in the extremities and trunk, but it can occur anywhere on the body.4,5 The distribution of dermatomyositis-associated calcinosis differs from that of systemic sclerosis in that it prominently affects both the trunk and the extremities. Extrusion of these nodules through the skin can occur and may cause secondary infection.5 Muscle calcification is generally asymptomatic and can only be detected radiologically.1
Each myositis-specific antibody is linked to a distinct clinical phenotype, with anti-NXP2, anti-Ro-52 and anti-MDA-5 autoantibodies most closely linked to calcinosis in both adult dermatomyositis and juvenile dermatomyositis.2,4 Anti-Mi-2 antibodies are highly specific for dermatomyositis, with no data correlating antibody titre with disease activity (sensitivity: 4.8–28.1%, specificity: 98.7–99.6%).3,7 Anti-Mi-2 is significantly associated with typical dermatomyositis skin lesions such as heliotrope rash, Gottron’s papules, V-sign and shawl-sign rashes, and cuticular overgrowth,3 but not with calcinosis in adult or juvenile dermatomyositis.2
This patient lacked most of the typical skin lesions despite having anti-Mi-2 antibodies, which differentiates this case from previous reports. The present case and previous reports of adult dermatomyositis with extensive calcinosis successfully treated with various treatment modalities have been summarized in Table 1. No known association has been reported so far between calcinosis and anti-Mi2-associated dermatomyositis in children or adults.2,3 The present case shows that patients with anti-Mi-2 antibodies may rarely present with skin findings other than those classically described.
| Cases | Age and gender | Site of calcinosis | Skin findings | Myositis-specific antibody (MSA) | Treatment given |
|---|---|---|---|---|---|
| Present case | 38, Female | Arms, upper chest, abdominal wall and thighs | Hyperpigmentation over face and chest | Anti Mi-2 | None started on any specific treatment |
| Vinen et al.,8 2000 | 20, Male | Proximal limbs and trunk | Not mentioned | Not mentioned | Diltiazem |
| Sultan-Bichat et al.,9 2012 | 46, Male | Left thumb, right knee | Not mentioned | Not mentioned | Extracorporeal shock-wave lithotripsy |
| Garel et al.,10 2015 | 49, Female | Arm, abdomen | Heliotrope rash, Gottron’s papules | Anti-NXP-2 | Intravenous immunoglobulin |
| Del Barrio-Díaz et al,.11 2016 | 65, Female | Trunk, elbows, knees | Not mentioned | Not mentioned | Topical sodium metabisulfite |
| Fodil et al.,12 2016 | 48, Male | Proximal limbs, abdomen | Heliotrope rash, v-sign, shawl sign, gottron papules | Anti-NXP2 | Zolendronate |
| Goossens et al.,13 2017 | 44, Female | Forearms, elbow, hips, back | Not mentioned | Anti-NXP2 | Intralesional sodium thiosulfate |
| Xie et al.,14 2020 | 24, Female | Upper arms and legs | Heliotrope rash, v-sign, shawl sign, gottron papules | Anti-SAE | Adalimumab |
| Shneyderman et al.,15 2021 | 50, Female | Neck, arm, lower back, abdomen | Heliotrope rash, Gottron’s papules | Anti-TIF-1γ | Tofacitinib |
Anti-NXP-2: Anti-nuclear matrix protein 2, Anti-SAE: Small ubiquitin-like modifier-activating enzyme, Anti-TIF-1γ: Transcription intermediary factor 1-gamma
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Identification of clinical features and autoantibodies associated with calcinosis in dermatomyositis. JAMA Dermatol. 2014;150:724.
- [Google Scholar]
- A comprehensive overview on myositis-specific antibodies: New and old biomarkers in idiopathic inflammatory myopathy. Clin Rev Allergy Immunol. 2017;52:1-19.
- [Google Scholar]
- Calcinosis biomarkers in adult and juvenile dermatomyositis. Autoimmun Rev. 2020;19:102533.
- [Google Scholar]
- Calcinosis cutis occurring in association with autoimmune connective tissue disease: The Mayo Clinic experience with 78 patients, 1996–2009. Arch Dermatol. 2012;148:455-62.
- [Google Scholar]
- Patterns of calcification in childhood dermatomyositis. AJR Am J Roentgenol. 1984;142:397-400.
- [Google Scholar]
- Autoantibodies to Mi-2 alpha and Mi-2 beta in patients with idiopathic inflammatory myopathy. Rheumatol. 2019;58:1655-61.
- [Google Scholar]
- Regression of calcinosis associated with adult dermatomyositis following diltiazem therapy. Rheumatol. 2000;39:333-4.
- [Google Scholar]
- Treatment of calcinosis cutis by extracorporeal shock-wave lithotripsy. J Am Acad Dermatol. 2012;66:424-9.
- [Google Scholar]
- Severe adult dermatomyositis with unusual calcinosis: Fig. 1. Rheumatol. 2015;54:2024.
- [Google Scholar]
- Topical sodium metabisulfite for the treatment of calcinosis cutis: A promising new therapy. Br J Dermatol. 2016;175:608-11.
- [Google Scholar]
- Universalis calcinosis in adult dermatomyositis: An “Anti-NXP2 syndrome”. J Clin Rheumatol. 2016;22:387-9.
- [Google Scholar]
- Efficacy of intralesional sodium thiosulfate injections for disabling tumoral calcinosis: Two cases. Semin Arthritis Rheum. 2017;47:451-5.
- [Google Scholar]
- Successful treatment of dermatomyositis and associated calcinosis with adalimumab. Clin Exp Dermatol. 2020;45:945-9.
- [Google Scholar]
- Calcinosis in refractory dermatomyositis improves with tofacitinib monotherapy: A case series. Rheumatol. 2021;60:e387-8.
- [Google Scholar]






