Translate this page into:
Anti-pruritic efficacies of doxycycline and erythromycin in the treatment of acne vulgaris: A randomized single-blinded pilot study
2 Biostatistics Unit, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
3 Department of Dermatology and Cutaneous Surgery, University of Miami Health System, USA
4 National Skin Centre; Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
Correspondence Address:
Hong Liang Tey
1 Mandalay Road, Singapore - 308205
Singapore
| How to cite this article: Cao T, Tan ES, Chan YH, Yosipovitch G, Tey HL. Anti-pruritic efficacies of doxycycline and erythromycin in the treatment of acne vulgaris: A randomized single-blinded pilot study. Indian J Dermatol Venereol Leprol 2018;84:458-460 |
Sir,
Pruritus is a significant symptom that is frequently experienced by patients with acne vulgaris and contributes significantly to patients' morbidity.[1],[2] In our clinical experience, pruritus in acne vulgaris can be effectively reduced with systemic antibiotics, such as doxycycline and erythromycin, which are commonly used as first-line systemic acne medications. However, it is not known if this effect results from a decrease in inflammation alone or if there are additional anti-pruritic effects mediated by the antibiotics. A study on human keratinocytes demonstrated that tetracycline attenuates the protease-activated receptor 2 interleukin-8 axis in the modulation of proinflammatory responses.[3] This effect was not observed in the macrolides, including erythromycin and clarithromycin.[4] Because protease-activated receptor 2 has been shown by multiple studies to be an important itch receptor, doxycycline may possibly have a greater efficacy in relieving itch through the inhibition of protease-activated receptor 2, as compared to erythromycin.
The aim of this randomized single-blinded pilot trial was to evaluate the anti-pruritic efficacies of doxycycline and erythromycin in the treatment of acne vulgaris. Approval for the study was obtained from the National Healthcare Group Ethics Review Board and Health Sciences Authority, Singapore.
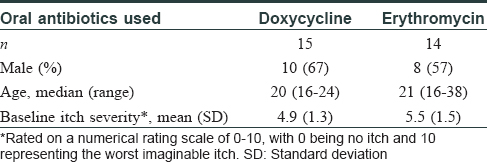
Patients with mild-to-moderate acne based on the Comprehensive Acne Severity Scale [Figure - 1] and [Figure - 2] and associated itch intensity of more than 2 on a 10-point numerical scale were recruited from the dermatology clinics at the National Skin Centre in Singapore.[5] Subjects were randomized to receive either oral doxycycline 100 mg daily or erythromycin 500 mg b.d. for 6 weeks. All subjects were instructed to stop the application of any topical agents during this period and to use the same type of mild cleanser (QV wash®) for facial washing up to a maximum of three times a day. At baseline and 6 weeks after treatment, an itch questionnaire was administered;[6] which included the average itch intensity over the prior 1 week on a 10-point numerical scale, frequency of itch (graded 1–7, ranging from 1 episode a month to more than 10 episodes daily) and itch quality-of-life assessment (16 questions, each graded 1–6 ranging from not affected to severely affected, giving a total score of 16–96). The severity of acne was also graded by a dermatologist blinded to the treatment arm (graded 0–5 on the Comprehensive Acne Severity Scale [Figure - 3], from clear to very severe) at baseline and at 6 weeks. Analyses were performed on a per-protocol basis using the paired t-test (for within-group comparisons) and two-sample t-test (for between-groups comparisons).
 |
| Figure 1: Grade 2 (mild in severity) acne based on Comprehensive Acne Severity Scale. Easily recognizable, less than half affected area involved. Many comedones, papules and pustules |
 |
| Figure 2: Grade 3 (moderate in severity) acne based on Comprehensive Acne Severity Scale. More than half affected area involved. Numerous comedones, papules and pustules |
 |
| Figure 3: Acne quality-of-life questionnaire |
Thirty-six subjects were recruited, of whom 29 completed the study and 7 were lost to follow-up. Of the 29 subjects, 14 received erythromycin, while 15 received doxycycline. Both groups had comparable baseline characteristics [Table - 1]. Grading of acne severity [Table - 2] significantly improved in both groups (P< 0.01), and there was no significant difference between the two treatment arms (P = 0.29). Subjects in the doxycycline group experienced a significant reduction in itch intensity scores at 6 weeks (P = 0.03) and this remained significant after adjusting for improvement in acne grading (P = 0.02). The reduction in itch intensity scores was not statistically significant in the erythromycin group (P = 0.11). Comparing the efficacies of doxycycline and erythromycin in reducing itch intensity scores, the difference was not statistically significant (P = 0.42). The itch quality-of-life scores were significantly better in both groups (P = 0.03), but the frequency of itch was not much different.
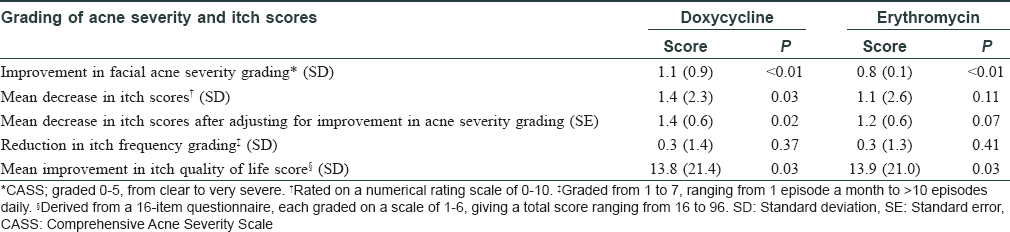
We were unable to find any previous reports of the anti-pruritic efficacies of systemic antibiotics in the treatment of acne. Doxycycline was found to significantly reduce pruritus in acne vulgaris and we postulate that in addition to a reduction in inflammation, attenuation of the protease-activated receptor 2 interleukin-8 pathway may contribute to this effect. A limitation of this study is the relatively high dropout rate (19%). Sample size is very small. Other factors like age of the patient, other comorbidities and general skin condition have not been taken into consideration.
In conclusion, our results revealed that doxycycline effectively reduces itch intensity in pruritic acne and this effect was independent of improvements in acne severity. Doxycycline may serve as a good antibiotic option for patients who experience itch in their acne lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Reich A, Trybucka K, Tracinska A, Samotij D, Jasiuk B, Srama M, et al. Acne itch: Do acne patients suffer from itching? Acta Derm Venereol 2008;88:38-42.
[Google Scholar]
|
| 2. |
Lim YL, Chan YH, Yosipovitch G, Greaves MW. Pruritus is a common and significant symptom of acne. J Eur Acad Dermatol Venereol 2008;22:1332-6.
[Google Scholar]
|
| 3. |
Ishikawa C, Tsuda T, Konishi H, Nakagawa N, Yamanishi K. Tetracyclines modulate protease-activated receptor 2-mediated proinflammatory reactions in epidermal keratinocytes. Antimicrob Agents Chemother 2009;53:1760-5.
[Google Scholar]
|
| 4. |
Tsuda T, Ishikawa C, Konishi H, Hayashi Y, Nakagawa N, Matsuki M, et al. Effect of 14-membered-ring macrolides on production of interleukin-8 mediated by protease-activated receptor 2 in human keratinocytes. Antimicrob Agents Chemother 2008;52:1538-41.
[Google Scholar]
|
| 5. |
Tan JK, Tang J, Fung K, Gupta AK, Thomas DR, Sapra S, et al. Prevalence and severity of facial and truncal acne in a referral cohort. J Drugs Dermatol 2008;7:551-6.
[Google Scholar]
|
| 6. |
Yosipovitch G, Zucker I, Boner G, Gafter U, Shapira Y, David M, et al. Aquestionnaire for the assessment of pruritus: Validation in uremic patients. Acta Derm Venereol 2001;81:108-11.
[Google Scholar]
|
Fulltext Views
4,935
PDF downloads
2,051





