Translate this page into:
Appearances in dermatopathology: The diagnostic and the deceptive
2 Department of Dermatology , Seth GS Medical College and KEM Hospital, Mumbai, India
Correspondence Address:
Uday Khopkar
OPD 117, 2nd Floor, OPD Building, Seth GS Medical College and K.E.M Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Madke B, Doshi B, Khopkar U, Dongre A. Appearances in dermatopathology: The diagnostic and the deceptive. Indian J Dermatol Venereol Leprol 2013;79:338-348 |
Abstract
Dermatopathology involves study of the microscopic morphology of skin sections. It mirrors pathophysiologic changes occurring at the microscopic level in the skin and its appendages. Sometimes, we come across certain morphologic features that bear a close resemblance to our physical world. These close resemblances are referred to as "appearances" in parlance to dermatopathology. Sometimes, these "appearances" are unique to a certain skin disorder and thus help us to clinch to a definitive diagnosis (e.g., "tadpole" appearance in syringoma). However, frequently, these appearances are encountered in many other skin conditions and can be therefore be misleading. In this paper, we attempt to enlist such "appearances" commonly found in the dermatopathologic literature and also enumerate their differential diagnoses.Introduction
Dermatopathologic descriptions of various cutaneous tumors and disorders are frequently referred to by their characteristic appearances. While labeling the appearance of a condition like "dilapidated brick wall" or "jigsaw puzzle" may not always help in the understanding of pathogenesis, it makes recall easier. It is from this point of view that we set upon to enlist the various labeled appearances in dermatopathology.
A thorough literature search was performed in Medline with the keywords "dermatopathologic appearances," "histopathological appearances," Portable document format (pdf) version of Rook′s Textbook of Dermatology 8 th edition and Fitzpatrick Dermatology in General Medicine 7 th edition was screened with the search word "appearance." A similar search was carried out in the html file of Lever′s Histopathology of Skin 9 th edition. All relevant searches were noted and a literature review was performed for each of the "appearance." No attempt has been made by the authors to make this paper comprehensive to include every uncommon "appearance." However, we have tried our best to compile all the possible "appearances" seen on histopathology on the basis of the available literature and with relevance to Indian dermatology. For ease of referencing, they have been placed in an alphabetical order. At places, we have tried to demonstrate the similarity between histopathological features and the physical world around us.
Antler Like/Stag Horn Appearance
Literally, antler means deciduous horn of a member of the deer family. Dowling Degos disease (DDD) is an autosomal-dominant disorder characterized by spotted and reticulate pigmentation of the flexures. Histopathology of the lesional skin shows delicate digitate downgrowth of the epidermis layer with melanocytic hyperplasia at the tip giving the resemblance to antler-like pattern [1] [Figure - 1]. However, a similar appearance may be seen in Haber′s syndrome, Galli Galli disease (acanthoeytic variant of Dowling Dego disease) and pigmented actinic keratosis. [2]
 |
| Figure 1: Rete ridges showing antler-like downgrowth with pigmentation at the tip in a case of Dowling Degos disease (H and E, ×40) |
Box Shaped/Squared off Appearance
Biopsy from the indurative stage of morphea (localized scleroderma) is squared off at the edges, giving the appearance of box-shaped (or boxed dermis appearance) biopsy under scanner view [3] [Figure - 2]. This boxing of the dermis probably happens due to the marked sclerosis of collagen throughout the reticular dermis and extending to the septa of subcutaneous fat. Morphea-lichen sclerosus overlap and scleredema can also similarly show squared off edges of biopsy specimen.
 |
| Figure 2: Biopsy from an indurated plaque showing boxed off appearance at the edges (H and E, ×40) |
Busy Dermis Appearance
It is a descriptive term for changes seen on scanning magnification, and is due to inflammatory infiltrate present in the interstitial dermis rather than around the superficial and deep perivascular location. It can be considered as a separate pattern seen in inflammatory or infiltrative dermatoses. Depending on the nature of infiltrate present in the dermis: (i) histiocytes-granuloma annulare, histiocytoma, interstitial granulomatous dermatitis of connective tissue diseases, interstitial granulomatous dermatitis with cutaneous cords and (ii) neutrophils-vasculitis, resolving folliculitis and Sweet′s syndrome. The busy dermis appearance can also be seen in the early stage of Kaposi′s sarcoma, desmoplastic melanoma, leukemia cutis, interstitial granulomatous drug reaction, mastocytosis and subtle breast carcinoma metastasis [4] [Figure - 3].
 |
| Figure 3: Hematoxylin and eosin section showing subtle interstitial infiltrate giving the whole specimen a "busy dermis" appearance (H and E, ×100) |
Camel Foot Appearance
It is a descriptive terminology for epidermal hyperplasia (regular acanthosis) seen in histopathology of plaque-type psoriasis. Normally, only 10% of the basal cells are in the proliferative phase, whereas in psoriasis about 90% of the basal cells are in the replicative phase. As a result, to accommodate the increasing population of basal cells, rete pegs take a plunge in the dermis in the form of regular elongation of rete ridges, giving the "camel foot" appearance to dermal rete ridges [5] [Figure - 4].
 |
| Figure 4: Regular acanthosis with rete peg elongation giving rete ridges a "camel foot" appearance (H and E, ×100) |
Cannon Ball Appearance
Classically seen in acquired tufted angioma (angioblastoma), a subtype of lobular capillary hemangioma (LCH) that shows clusters of angiomatous tufts and lobules scattered in the dermis in a "cannon ball" pattern. [6],[7] However, similar tufts of thick-walled capillaries are frequently seen in pseudo-Kaposi′s sarcoma or angiodermatitis of Mali.
Chicken Wire/Fish Net Pattern
It is a descriptive terminology seen on direct immunofluorescence study of pemphigus vulgaris, where intercellular deposition of IgG and C3 between epidermal cells give a "chicken wire" or "fish net" appearance [8] [Figure - 5]. Myxoid liposarcoma is a low-grade tumor composed of hypocellular bland fusiform to ovoid cells in a myxoid stroma with a prominent plexiform capillary network and scattered signet-ring lipoblasts. Myxoid liposarcoma shows prominent branching pattern of capillaries throughout the tumor in a so-called chicken-wire pattern. [9]
 |
| Figure 5: Direct immunofluorescence studies showing intercellular deposition of immune complexes giving a "chicken wire/fish net" look (×100) |
Church Spire Appearance
Described in the histopathology of "hyperkeratotic seborrheic keratosis" and "acrokeratosis verruciformis of Hopf" (an allelic disorder to Darier′s disease). Both these entities show a distinctive pattern of epidermal features with hyperkeratosis, hypergranulosis and acanthosis together with papillomatosis. These epidermal changes frequently lead to numerous digitate upward extensions of epidermis-lined papillae, giving the appearance of "church spires." [10],[11] Other conditions where "church spire" appearance can be seen are verruca vulgaris, epidermodysplasia verruciformis, verruca plana, actinic keratosis, arsenic keratosis, tar keratosis, acanthosis nigricans, epidermal nevus, confluent and reticulate papillomatosis of Gougerot-Carteaud, hyperkeratosis lenticularis and verrucous carcinoma [12] [Figure - 6].
 |
| Figure 6: Biopsy from a seborrheic keratosis showing hyperkeratosis along with papillomatosis resembling the epidermal changes as "church spire" (H and E, ×40) |
Claw Clutching Ball Appearance
The histological appearance of lichen nitidus is commonly referred to as ball and claw configuration for the infiltrate and epidermis, respectively. The ball is comprised of well-circumscribed granulomatous infiltrate composed of lymphocytes, epithelioid cells and occasional Langhans giant cells that are clutched by surrounding hyperplastic rete ridges, giving the overall "claw clutching ball" appearance [13] [Figure - 7]. Similar resemblance can be seen in histology of early lesions of juvenile xanthogranuloma (JXG) and lichenoid eruptive histiocytoma. Occasionally, micropapular lichen planus and tuberculoid leprosy may show such appearance, although with shorter "claws."
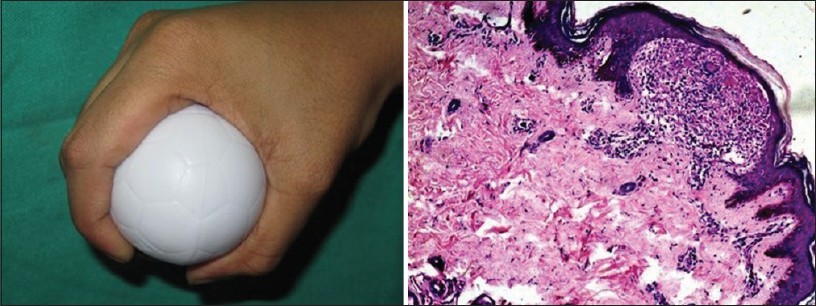 |
| Figure 7: Histology of lichen nitidus showing well-defined granuloma enclosed by rete pegs giving the appearance of "claw clutching a ball" on scanning magnification (H and E, ×40) |
Clock Face/Cart Wheel Appearance
Plasma cell has a characteristic cart-wheel appearance owing to its typical nuclear configuration. The plasma cell is round or oval, with an eccentrically placed nucleus and chromatin arranged in a pyramidal block against the nuclear membrane, giving the characteristic "cart wheel" appearance. [14]
Coat Sleeve Appearance
Historically, coat sleeve appearance was described in the histopathology of primary and secondary lesions of syphilis, where the inflammatory infiltrate of lymphocytes and plasma cells are located in a perivascular coat sleeve-like pattern. [15] A similar picture can also be seen in the histology of erythema annulare centrifugum, where dermal perivascular infiltrate of lymphocytes is arranged in a "coat sleeve" pattern. [16] Several other inflammatory diseases with lymphoplasmocytic infiltrate may show perivascular coat sleeve pattern. However, the thickened endothelial lining contributes to the coat sleeve appearance in syphilis.
Cribriform Appearance
Literally, cribriform means a structure having resemblance to a sieve akin to cribriform plate of the ethmoid bone through which pass the fibers of the olfactory nerve. Trichoepithelioma is a benign neoplasm showing mostly follicular germinative differentiation. [17] Five different histopathologic patterns have been described columnar (desmoplastic trichoepithelioma), retiform, racemiform, adamantenoid and cribriform (trichoepithelioma).
Histology of trichoepithelioma of the cribriform pattern shows presence of horn cysts of varying sizes and basaloid epithelial cribriform nests and a few elongated strands embedded in a fibroblastic stroma [Figure - 8]. Papillary mesenchymal bodies formed by stromal fibroblastic aggregation are seen typically adjacent to epithelial islands. However, cribriform pattern may also be seen with basal cell carcinoma, glomus tumor and several other benign and malignant neoplasms.
 |
| Figure 8: Hematoxylin and eosin-stained section of trichoepithelioma showing epithelial islands in a cribriform pattern (H and E, ×100) |
Dilapidated Brick Wall Appearance
It is a well known appearance in dermatopathology. It is classically seen in Hailey-Hailey disease, which shows prominent suprabasal clefting and extensive loss of intercellular bridges (acantholysis) with partial coherence of cells between keratinocytes, giving the whole epidermis a "dilapidated brick wall" appearance. [18] It has also been described in cases of bullous Darier′s disease and Hailey-Hailey variant of Grover disease [19],[20] [Figure - 9].
 |
| Figure 9: Biopsy from a representative lesion of Hailey-Hailey disease showing partial acantholytic dyskeratosis giving the whole epidermis a "dilapidated brick wall resemblance" (H and E, ×100) |
Festooned Papillae Appearance (See Undecorated Tomb Stoning)
Classically described in the histopathology of porphyria cutanea tarda, wherein a biopsy from a fresh blister shows a subepidermal bulla with minimal dermal inflammatory infiltrate and dermal papillae protruding upward into the blister cavity (festooning) and hence the name "festooned papillae" appearance [21] [Figure - 10].
 |
| Figure 10: Biopsy from a blister in a case of porphyria showing subepidermal blister along with festooning of dermal papillae (×100) |
Flame-Thrower-Like Appearance
It is a histopathological description of the vertical section of telogen hair shaft. Telogen club hairs have a non-pigmented bulb with an irregular shaggy border. The presence of bright red trichilemmal keratin bordering the club hair results in a "flame-thrower like" appearance in vertical hematoxylin and eosin sections [22] [Figure - 11].
 |
| Figure 11: Vertical section from scalp biopsy showing telogen hair lined with eosinophilic trichilemmal keratin giving "flame thrower" appearance (H and E, ×200) |
Fried Egg Appearance
Mast cells are found in small numbers (up to 10 mast cells per 40X field) in a perivascular location in the dermis and larger number in some neoplasms (e.g., neurofibroma) and certain forms of mastocytosis. These cells are commonly oval with a centrally located dark round nucleus, giving a "fried egg" appearance [23] [Figure - 12].
 |
| Figure 12: Histology of mastocytosis showing numerous mast cells having centrally located nuclei (H and E, ×200) |
Hobnail (Matchstick) Appearance
Retiform hemangioendothelioma is a rare variant of low-grade angiosarcoma characterized by indolent clinical behavior. Histologically, it bears a close resemblance to the architecture of rete testis on scanning magnification. The tumor is composed of elongated, arborizing blood vessels lined by monomorphic bland endothelial cells with prominent apical nuclei and scanty cytoplasm. These endothelial cells have been described to have a "match stick" or hobnail appearance. [24],[25] Similar is the appearance of endothelial cells lining the vessels of angiolymphoid hyperplasia. [26]
Jigsaw Puzzle Appearance
Cylindroma is a benign tumor of hair follicle origin. The tumor is composed of irregularly shaped islands of basaloid cells arranged in a mosaic-like mass molding together in a "jigsaw puzzle" pattern [27] [Figure - 13]. A rim of densely eosinophilic, Periodic acid Schiff-positive basement membrane-like material commonly envelops the individual nests. A similar jigsaw puzzle appearance of tumorous mass was also reported in eccrine spiradenomas. [28]
 |
| Figure 13: Histological section of cylindroma showing numerous tumor islands molded into each other giving a "jigsaw puzzle" appearance (H and E, ×100) |
Mariner′s Pilot Wheel Appearance
It is description of the tissue phase of paracoccidioidomycosis (also known as Brazilian blastomycosis, South American blastomycosis, Lutz-Splendore-de Almeida disease) caused by the thermally dimorphic fungus Paracoccidioides brasiliensis. In biopsy specimens, the tissue phase of the fungus is seen as multiple buds surrounding the whole surface of the mother yeast cell. This configuration is described as "Mariner′s pilot wheel" or "Mickey mouse" appearance [29] [Figure - 14].
 |
| Figure 14: Gomori methenamine silver stain showing the tissue phase of paracoccidioidomycosis resembling the so-called "Mariner's pilot wheel" appearance (×1000) |
Morula-Like Appearance
Protothecosis is a rare infection caused by members of the genus Prototheca, an achlorophyllic alga. Olecranon bursitis and localized cutaneous infections are the most common presentation seen in immunocompetent patients. [30] Prototheca species divide by symmetrical endosporulation. Lactophenol cotton blue or calcofluor white mount of culture reveals the morula-like appearance of sporangia containing multiple endospores; however, the endospores are less as compared with that seen in rhinosporidiosis and coccidioidomycosis. [31]
Onion Skin Appearance
Pacinian corpuscle is a specialized type of touch receptor present in the deeper layers of the skin. Each corpuscle is composed of the end of a sensory nerve fiber with layers of connective tissue wrapped around it, resembling "onion skin" appearance. [32],[33],[34] Mycobacterial infiltration of the nerve in cases of borderline and polar lepromatous leprosy leads to proliferation of perineurium of the nerve bundles leading to "onion peel appearance" [35] [Figure - 15]. Eosinophilic angiocentric fibrosis (mucosal variant of granuloma faciale) and chronic fibrosing vasculitis could lead to a similar "onion skin" appearance due to extensive fibrosis of blood vessels. [36]
 |
| Figure 15: Histology of pacinian corpuscle showing the classical onion peel appearance (H and E, ×200) |
Owl′s Eye Appearance
Histopathology of verruca plana shows, in addition to hyperkeratosis and acanthosis, diffuse vacuolization of cells in the upper spinous and granular layer. The nuclei of the vacuolated cells lie at the centers of the cells with empty shells around the nucleus. This appearance of vacuolated cells is referred to as Owl eye appearance [37] [Figure - 16]. These vacuolated cells should be differentiated from Paget cells. Similar "owl′s eye" appearance of Reed Sternberg cell (cells having either multinucleated or bilobed nucleus) is considered pathognomonic for classical Hodgkin′s lymphoma. [38]
 |
| Figure 16: Histopathology of verruca plana showing the typical cytopathic effect on keratinocytes called as koilocytes having a perinuclear halo referred to as "owl-eye appearance" (H and E, ×200) |
Paint Brush-Like Appearance
The name Penicillium comes from the word "brush." Penicilliosis is a systemic fungal infection caused by a dimorphic fungus, Penicillium marneffei, common in HIV patients whose CD4 count is less than 50/mm, 3 and was first isolated from bamboo rats in Vietnam. [39] Fungal culture shows grey-white colonies surrounded by diffusible red pigment, and lactophenol cotton blue stain preparation of the culture specimen shows brush-like clusters of septate hyphae with terminal conidiospores. [40]
Palisading Appearance
Palisade means a wall or fence made from either wooden stakes or iron plates, and is built to defend a structure. In dermatopathology, palisading means typical arrangement of cells of either tumorous origin as in basal cell carcinoma, [41] where basal layer of cells lies perpendicular to the basement membrane giving a palisaded appearance or histiocytes surround a deposit or area of collagen alteration in granuloma annulare. [42],[43] Benign tumors like palisaded and encapsulated neuroma also show palisading by spindle cells of neural origin. [44] Other conditions where palisading appearance can be seen are: Palisading neutrophilic and granulomatous dermatitis, [45],[46] rheumatoid nodule, necrobiosis lipoidica, [47] syphilis and foreign body reaction [48] [Figure - 17].
 |
| Figure 17: Specimen obtained from nodular basal cell carcinoma showing the classical arrangement of peripheral basaloid cells in a palisading configuration (H and E, ×200) |
Picket Fence Appearance
This appearance is seen on direct immunofluorescence (DIF) studies of dermatitis herpetiformis. DIF of non-involved perilesional skin shows deposit of IgA alone or in combination with C3, which are arranged in a granular pattern at the dermoepidermal junction. These granular deposits may be vertically elongated, giving a "picket-fence" appearance [49] [Figure - 18].
 |
| Figure 18: Direct immunofluorescence showing deposition of IgA along the tips of dermal papilla giving a "picket fence" appearance. (×100) (Photo contributed by Dr. Raghavendra Rao, Kasturba Medical College, Manipal) |
Ravelled Wool Appearance
Literally, ravelled means tangled mass of threads. It is a classical histopathological description seen in pseudoxanthoma elasticum (PXE). Biopsy from a lesion will show small, fragmented, wavy and clumped eosinophilic elastic fibers, giving a "ravelled wool" appearance [50] [Figure - 19]. Similar appearance of elastic fibers can also be seen in D-penicillamine-induced PXE and periumbilical PXE. [51]
 |
| Figure 19: Biopsy from a papular lesion of pseudoxanthoma elasticum showing fragmented and calcified elastic fibers forming a tangled mass resembling woolen threads, the so-called "ravelled wool appearance" (H and E, ×200) |
Safety Pin Appearance
In granulomatous lesions of donovanosis, the bacterium Calymmatobacterium granulomatis (C. granulomatis) displays characteristic bipolar staining, giving a "safety pin appearance." [52] These bacilli are found in large number in the cytoplasm of mononuclear cells of the monocyte/macrophage lineage forming Donovan bodies.
Saw-Tooth Appearance
Yet another well-known histopathological finding seen in lichen planus. Histology of lichen planus shows irregular hyperplasia of the malpighian (spinous) layer (irregular acanthosis) in a triangular pattern giving a saw-tooth appearance [53] [Figure - 20]. Similar saw tooth appearance may be seen in some cases of lichenoid drug eruptions and in lichen planus-like keratoses.
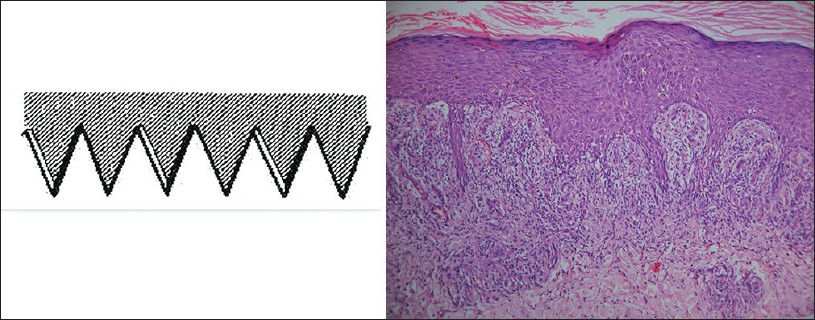 |
| Figure 20: Histology of a papule of lichen planus showing the typical saw tooth morphology of rete ridges (H and E, ×100) |
Septate Tomato Appearance
In Molluscum contagiosum, scanner view of hematoxylin and eosin-stained sections shows an epidermal invagination with several closely spaced lobules of epidermal proliferation leading to a septate tomato appearance. The septum of this appearance is formed by normal dermis and not by epidermal proliferation. In the lower epidermis, these viral bodies appear as minute, ovoid eosinophilic structures. At the level of granular layer, these bodies change their staining pattern from eosinophilic to basophilic [Figure - 21].
 |
| Figure 21: Molluscum contagiosum showing the epidermal invagination and numerous eosinophilic viral inclusion bodies resembling a septate tomato on scanner view (H and E, ×40) |
Sieve-Like Appearance
Kaposi sarcoma (KS) is a low-grade malignant tumor of vascular origin associated with human herpes simplex virus 8 (HHV-8) infections. Biopsy from the plaque stage of KS shows spindle cells arranged in fascicles with slit-like dense and irregular vascular spaces, creating a sieve-like appearance. [54]
Spaghetti and Meatball Appearance (Banana and Grape Appearance)
Hematoxylin and eosin-stained biopsy from the lesions of pityriasis versicolor shows slender septate hyphae and spores resembling the sphagetti and meat ball appearance [55] [Figure - 22].
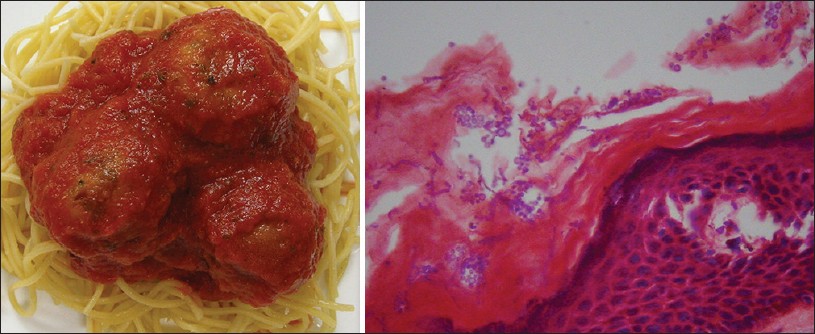 |
| Figure 22: Numerous fungal elements of malasezzia species seen as elongated hyphae and spores, familiarly called as "spaghetti and meat-ball" appearance (×200) |
Storiform Appearance
This is classically described in dermatofibrosarcoma protuberans (DFSP), but is also seen in the frequently seen dermatofibroma. DFSP is a rare, locally aggressive dermal tumor composed of interwoven bundles of spindle cells with plump nuclei arranged in a "storiform or pinwheel pattern" [56] [Figure - 23]. Storiform appearance is also seen in dermatofibroma, where histiocytes are arranged in a storiform or whorled pattern in the reticular dermis with evidence of entrapped collagen bundles at its peripheral margins (c.f. DFSP). In DFSP, the proliferation extends into the fibrous septae of subcutaneous tissue forming pseudoseptae.
 |
| Figure 23: Hematoxylin and eosin-stained specimen showing "storiform/whorled" appearance of dermatofibroma sarcoma protuberans (H and E, ×200) |
Swarm of Bees Appearance
It is a characteristic histopathological picture seen in active alopecia areata, where the perifollicular inflammation, in particular peribulbar infiltrates, is composed of predominantly lymphocytes around anagen hair follicles. This pattern of infiltrate is referred to as "swarm of bees" appearance [57] [Figure - 24]. Similar appearance has been reported in leishmaniasis, wherein giemsa stain of tissue material shows numerous amastigote (20-30 in number) arranged in a "swarm of bees" fashion within the cytoplasm of macrophages. [58]
 |
| Figure 24: Lymphocytic infiltrate around anagen follicle resembling a "swarm of bees" (H and E, ×200 and 100) |
Swiss Cheese Appearance
This appearance is reported in cases of paraffinoma (sclerosing lipogranuloma). Paraffin is a mineral oil and is not hydrolyzed by tissue lipases and, hence, is treated by the body as a foreign substance. The most common site of injecting paraffin oil is the penis and breast. [59],[60] Biopsy obtained from the infiltrated area shows presence of numerous ovoid or round cavities where the paraffin resided prior to processing, giving the "Swiss cheese" appearance.
Tadpole/Comma-Shaped Appearance
Classically seen at scanning magnification in histology of syringoma. This benign tumor of eccrine lineage comprises of numerous ducts lined by two rows of epithelial cells embedded in a fibrous stroma. The epithelial component is arranged in nests, cords or tubules of relatively uniform size. Depending upon the plane of section, some nests of syringoma can assume a morphology that closely resembles a comma or tadpole. [61] Similar tadpole appearance of epitheial strands is also reported in desmoplastic trichoepithelioma, sclerosing basal cell carcinoma and microcystic adnexal carcinoma [Figure - 25].
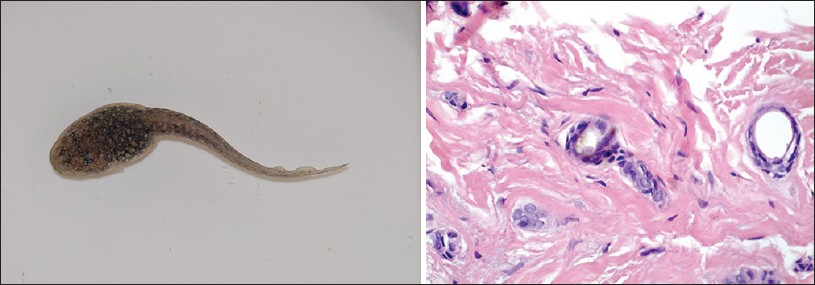 |
| Figure 25: Histology of syringoma showing typical "tadopole/ comma shaped" epithelial tumor strand (H and E, ×200) |
Telephone Handle Appearance
Another well known cellular appearance among hematologist. The deep red nucleus of an eosinophil is composed of two lobes connected by a band of nuclear material, and resembles the old-fashioned "telephone receiver" [62] [Figure - 26].
 |
| Figure 26: Bilobed nucleus of eosinophil resembling an old "telephone receiver" (H and E, ×200) |
Tissue Culture-Like Appearance
Nodular fasciitis is a self-limiting benign reactive fibroblastic growth, and is often mistaken for malignant neoplasm with its feature of rapid growth and histological appearance. Clinically, it usually presents as a solitary, rapidly developing, sometimes tender, subcutaneous nodule that reaches its ultimate size of 1-5 cm. Histology from a well-developed nodular lesion shows plump fibroblasts growing haphazardly in a vascular, myxoid stroma presenting a "tissue culture-like" appearance. [63]
Tomb Stone Appearance
Classically described in the histopathology of fresh blister of pemphigus vulgaris or drug-induced pemphigus. Suprabasal splitting of the epidermis leads to blister formation, with the basal layer still remaining adherent to the basement membrane, and gives the resemblance to the row of the tomb stone [64],[65] [Figure - 27]. Ackerman and colleagues have classified tomb stoning into two broad categories: Decorated tomb stone (discrete dermal papillae covered by a single row of basal keratinocytes that project into an intraepidermal blister) and undecorated tomb stone (discrete, well-preserved dermal papillae beneath a subepidermal blister). [1] Decorated tombstones have been described apart from pemphigus in Grover′s disease, Darier′s disease, Hailey-Hailey disease, warty dyskeratoma and solar keratosis, whereas undecorated tomb stone has been described in suction blister, porphyria, pseudoporphyria, bullous pemphigoid, herpes gestationis and epidermolysis bullosa junctional and dystrophic variant.
 |
| Figure 27: Suprabasal acantholysis in pemphigus showing the characteristic "row of tombstone" appearance (H and E, ×100) |
Trilayered/Striped Appearance
The histology picture of lichen sclerosus is commonly referred to as "tri-layered or striped" appearance. The established lesion of lichen sclerosis shows three distinct zones: (i) epidermal atrophy with surface hyperkeratosis, (ii) an underlying broad zone of subepidermal edema in the papillary dermis and (iii) homogenization and ground glass appearance of collagen, which becomes more sclerotic over time. [67]
A similar trilayered appearance can be seen in the histology of soft chancre (chancroid) caused by Hemophilus ducreyi: (i) superficial zone consisting of necrotic tissues and an acute inflammatory infiltrate, (ii) the mid-zone containing new blood vessels and regenerating granulation tissue on one hand and degenerative changes on the other and (iii) the deeper zone shows a chronic inflammatory infiltrate of plasma cells and lymphocytes. [68]
Windblown Appearance
A descriptive term for the enlarged, crowded, haphazardly arranged neoplastic cells that show loss of polarity, enlarged and hyperchromatic nuclei and atypical mitoses in the epithelium of Bowen′s disease and bowenoid papulosis of the genitalia. This overall appearance in the epithelium of Bowen′s disease is referred to as "windblown appearance" [69],[70] [Figure - 28].
 |
| Figure 28: Haphazard orientation of keratinocytes seen in Bowen's disease commonly referred to as "windblown" appearance of dysplastic cells (H and E, ×100) |
| 1. |
Bhagwat PV, Tophakhane RS, Shashikumar BM, Noronha TM, Naidu V. Three cases of Dowling Degos disease in two families. Indian J Dermatol Venereol Leprol 2009;75:398-400.
[Google Scholar]
|
| 2. |
Yanofsky VR, Mercer SE, Phelps RG. Histopathological variants of cutaneous squamous cell carcinoma: A review. J Skin Cancer 2011;2011:210813.
[Google Scholar]
|
| 3. |
Gruss CJ, Von Kobyletzki G, Behrens-Williams SC, Lininger J, Reuther T, Kerscher M, et al. Effects of low dose ultraviolet A-1 phototherapy on morphea. Photodermatol Photoimmunol Photomed 2001;17:149-55.
[Google Scholar]
|
| 4. |
Weedon D, Geoffrey S. Diagnostic clues. In: Weedon D, Geoffrey S, editors. Skin pathology. 2 nd ed. China: Churchill Livingstone; 2004. p. 20.
[Google Scholar]
|
| 5. |
IADVL Digital Lecture Series. Psoriasis. Available from: http://www.scribd.com/doc/44692083/Speaker-Notes, page 11 [Last accessed on 2012 Mar 9].
[Google Scholar]
|
| 6. |
Chakraborty S, Gharami RC, Das NK, Datta PK. Annular tufted angioma: A rare entity. Int J Dermatol 2009;48:614-6.
[Google Scholar]
|
| 7. |
Schaffer JV, Fangman W, Bossenbroek NM, Meehan SA, Kamino H. Tufted angioma. Dermatol Online J 2008;14:20.
[Google Scholar]
|
| 8. |
Darling MR, Daley T. Blistering mucocutaneous diseases of the oral mucosa-a review: Part 2. Pemphigus vulgaris. J Can Dent Assoc 2006;72:63-6.
[Google Scholar]
|
| 9. |
Fritchie KJ, Goldblum JR, Tubbs RR, Sun Y, Carver P, et al. The expanded histologic spectrum of myxoid liposarcoma with an emphasis on newly described patterns: Implications for diagnosis on small biopsy specimens. Am J Clin Pathol 2012;137:229-39.
[Google Scholar]
|
| 10. |
Bang CH, Kim HS, Park YM, Kim HO, Lee JY. Non-familial Acrokeratosis Verruciformis of Hopf. Ann Dermatol 2011;23:S61-3.
[Google Scholar]
|
| 11. |
Shall L, Marks R. Stucco keratoses. A clinico-pathological study. Acta Derm Venereol 1991;71:258-61.
[Google Scholar]
|
| 12. |
Weedon D, Geoffrey SS. An approach to the interpretation of skin biopsies. In: Weedon D, Geoffrey S, editors. Skin pathology. 2 nd ed. China: Churchill Livingstone; 2004. p. 12.
[Google Scholar]
|
| 13. |
Mehta V, Balachandran C. Generalized lichen nitidus in childhood. Indian J Dermatol 2008;53:221-2.
[Google Scholar]
|
| 14. |
Paraskevas F. B Lymphocytes. In: Greer JP, Foerster J, Rodgers GM, Paraskevas F, Glader B, Arber DA, et al. editors. Wintrobe's Clinical Hematology. 12 th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 346.
th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 346.'>[Google Scholar]
|
| 15. |
Engelkens HJ, ten Kate FJ, Vuzevski VD, van der Sluis JJ, Stolz E. Primary and secondary syphilis: A histopathological study. Int J STD AIDS 1991;2:280-4.
[Google Scholar]
|
| 16. |
Ibrahim SF, Pryor J, Tausk FA. Stress-induced erythema annulare centrifugum. Dermatol Online J 2009;15:15.
[Google Scholar]
|
| 17. |
Bettencourt MS, Prieto VG, Shea CR. Trichoepithelioma: A 19-year clinicopathologic re-evaluation. J Cutan Pathol 1999;26:398-404.
[Google Scholar]
|
| 18. |
Narbutt J, Chrusciel A, Rychter A, Fijuth J, Lesiak A, Sysa-Jedrzejowska A. Persistent improvement of previously recalcitrant Hailey-Hailey disease with electron beam radiotherapy. Acta Derm Venereol 2010;90:179-82.
[Google Scholar]
|
| 19. |
Kakar B, Kabir S, Garg VK, Bhushan P. A case of bullous Darier�s disease histologically mimicking Hailey-Hailey disease. Dermatol Online J 2007;13:28.
[Google Scholar]
|
| 20. |
Weaver J, Bergfeld WF. Grover disease (transient acantholytic dermatosis). Arch Pathol Lab Med 2009;133:1490-4
[Google Scholar]
|
| 21. |
Welsh B. Blistering skin conditions. Aust Fam Physician 2009;38:484-90.
[Google Scholar]
|
| 22. |
James WD, Berger TG, Elston DM, editors. Skin: Basic structure and function. Andrews diseases of the skin. 10 th ed. Philadelphia, PA: Saunders Elsevier; 2006. p. 9-10.
[Google Scholar]
|
| 23. |
Sweet WL, Smoller BR. Perivascular mast cells in urticaria pigmentosa. J Cutan Pathol 1996;23:247-53.
[Google Scholar]
|
| 24. |
Bhutoria B, Konar A, Chakrabarti S, Das S. Retiform hemangioendothelioma with lymph node metastasis: A rare entity. Indian J Dermatol Venereol Leprol 2009;75:60-2.
[Google Scholar]
|
| 25. |
Zhang G, Lu Q, Yin H, Wen H, Su Y, Li D, Xiao R. A case of retiform-hemangioendothelioma with unusual presentation and aggressive clinical features. Int J Clin Exp Pathol 2010;3:528-33.
[Google Scholar]
|
| 26. |
Karabudak O, Taskapan O, Bozdogan O, Dogan B. Angiolymphoid hyperplasia with eosinophilia: Atypical appearance in an older patient. Indian J Dermatol 2008;53:144-5
[Google Scholar]
|
| 27. |
Massoumi R, Podda M, Fässler R, Paus R. Cylindroma as tumor of hair follicle origin. J Invest Dermatol 2006;126:1182-4.
[Google Scholar]
|
| 28. |
Englander L, Emer JJ, McClain D, Amin B, Turner RB. A Rare Case of Multiple Segmental Eccrine Spiradenomas. J Clin Aesthet Dermatol 2011;4:38-44.
[Google Scholar]
|
| 29. |
Godoy H, Reichart PA. Oral manifestations of paracoccidioidomycosis. Report of 21 cases from Argentina. Mycoses 2003;46:412-7.
[Google Scholar]
|
| 30. |
Lu S, Xi L, Qin W, Luo Y, Lu C, Li X. Cutaneous protothecosis: Two new cases in China and literature review. Int J Dermatol 2012;51:328-31.
[Google Scholar]
|
| 31. |
Cho BK, Ham SH, Lee JY, Choi JH. Cutaneous protothecosis. Int J Dermatol 2002;41:304-6.
[Google Scholar]
|
| 32. |
Bell J, Bolanowski S, Holmes MH. The structure and function of Pacinian corpuscles: A review. Prog Neurobiol 1994;42:79-128.
[Google Scholar]
|
| 33. |
Lever WF, Schaumberg-Lever G. Histopathology of the Skin. 6 th ed. Philadelphia: J.B. Lippincott Company; 1983. p. 673-4.
[Google Scholar]
|
| 34. |
Provitera V, Nolano M, Pagano A, Caporaso G, Stancanelli A, Santoro L. Myelinated nerve endings in human skin. Muscle Nerve 2007;35:767-75.
[Google Scholar]
|
| 35. |
Gupta R, Singal A, Pandhi D. Genital involvement and type I reaction in childhood leprosy. Lepr Rev 2005;76:253-7.
[Google Scholar]
|
| 36. |
John SS, Philip SS, Premkumar AJ, David S. Chronic localized fibrosing vasculitis of the eyelid. Arch Ophthalmol 2009;127:1396-7.
[Google Scholar]
|
| 37. |
Pavithra S, Mallya H, Pai GS. Extensive presentation of verruca plana in a healthy individual. Indian J Dermatol 2011;56:324-5
[Google Scholar]
|
| 38. |
Sequeira F, Gandhi S, Kini U, Bhat I. Named cells in dermatology. Indian J Dermatol Venereol Leprol 2012;78:207-16
[Google Scholar]
|
| 39. |
Wong SY, Wong KF. Penicillium marneffei Infection in AIDS. Patholog Res Int 2001;2011:764293.
[Google Scholar]
|
| 40. |
Jung JY, Jo GH, Kim HS, Park MY, Shin JH, Chin BS, Bang JH, Shin HS. Disseminated penicilliosis in a Korean human immunodeficiency virus infected patient from Laos. J Korean Med Sci 2012;27:697-700.
[Google Scholar]
|
| 41. |
Moneghini L, Falleni M, Romagnoli S, Bombonato C, Gualandri L. Central nuclear palisading in nodular basal cell carcinoma: Morphological and immunohisto-chemical concerns. Acta Derm Venereol 2011;91:76-7.
[Google Scholar]
|
| 42. |
Chaitra V, Inchara YK, Rajalakshmi T, Antony M. Granuloma annulare-histology reconsidered. Indian J Dermatol Venereol Leprol 2010;76:568-9.
[Google Scholar]
|
| 43. |
Gupta D, Hess B. Granuloma annulare. Sci World J 2010;10:384-6.
[Google Scholar]
|
| 44. |
Gutte R, Garg G, Doshi B, Kharkar V, Khopkar U. SkIndia Quiz 4-Asymptomatic sessile skin colored nodule over columella of nose. Indian Dermatol Online J 2011;2:131-2.
[Google Scholar]
|
| 45. |
Brecher A. Palisaded neutrophilic and granulomatous dermatitis. Dermatol Online J 2003;9:1.
[Google Scholar]
|
| 46. |
Gutte R, Khopkar U. Isolated unilateral palisaded neutrophilic and granulomatous dermatitis. Indian J Dermatol Venereol Leprol 2011;77:615-7.
[Google Scholar]
|
| 47. |
Magro CM, Crowson AN, Regauer S. Granuloma annulare and necrobiosis lipoidica tissue reactions as a manifestation of systemic disease. Hum Pathol 1996;27:50-6.
[Google Scholar]
|
| 48. |
Mysore V. Granulomas. In: Mysore V, editor. Fundamentals in Dermatopathology. 1 st ed. Bahrain: Oriental Press; 2002. p. 80.
[Google Scholar]
|
| 49. |
James WD, Berger TG, Elston DM, editors. Chronic Blistering Dermatoses. Andrews diseases of the skin. 10 th ed. Philadelphia, PA: Saunders Elsevier; 2006. p. 475.
[Google Scholar]
|
| 50. |
Mehta B, Amladi S, Nayak C, Savant S. An unusual periumbilical plaque. Indian J Dermatol Venereol Leprol 2008;74:697-8.
[Google Scholar]
|
| 51. |
Bécuwe C, Dalle S, Ronger-Savlé S, Skowron F, Balme B, Kanitakis J, et al. Elastosis perforans serpiginosa associated with pseudo-pseudoxanthoma elasticum during treatment of Wilson's disease with penicillamine. Dermatology 2005;210:60-3.
[Google Scholar]
|
| 52. |
Carter J, Hutton S, Sriprakash KS, Kemp DJ, Lum G, Savage J, et al. Culture of the causative organism of donovanosis (Calymmatobacterium granulomatis) in HEp-2 cells. J Clin Microbiol 1997;35:2915-7.
[Google Scholar]
|
| 53. |
Gül U, Soylu S, Demiriz M. Colocalization of lichen planus and vitiligo associated with selective IgA deficiency. Skin Med 2007;6:202-3.
[Google Scholar]
|
| 54. |
Grayson W, Pantanowitz L. Histological variants of cutaneous Kaposi sarcoma. Diagn Pathol 2008;3:31.
[Google Scholar]
|
| 55. |
Chaudhary R, Singh S, Banerjee T, Tilak R. Prevalence of different Malassezia species in pityriasis versicolor in central India. Indian J Dermatol Venereol Leprol 2010;76:159-64.
[Google Scholar]
|
| 56. |
Sathyanarayana BD. Childhood onset dermatofibrosarcoma protuberans. Indian J Dermatol Venereol Leprol 2004;70:310-2.
[Google Scholar]
|
| 57. |
Hordinsky MK. Treatment of alopecia areata: "What is new on the horizon?" Dermatol Ther 2011;24:364-8.
[Google Scholar]
|
| 58. |
Gupta LK, Singhi MK. Tzanck smear: A useful diagnostic tool. Indian J Dermatol Venereol Leprol 2005;71:295-9.
[Google Scholar]
|
| 59. |
Khong PL, Ho LW, Chan JH, Leong LL. MR imaging of breast paraffinomas. AJR Am J Roentgenol 1999;173:929-32.
[Google Scholar]
|
| 60. |
Lee T, Choi HR, Lee YT, Lee YH. Paraffinoma of the penis. Yonsei Med J. 1994;35:344-8.
[Google Scholar]
|
| 61. |
Obaidat NA, Alsaad KO, Ghazarian D. Skin adnexal neoplasms--part 2: An approach to tumours of cutaneous sweat glands. J Clin Pathol 2007;60:145-59.
[Google Scholar]
|
| 62. |
Wiki answers. What are granulocytes and agranulocytes? Available from: http://wiki.answers.com/Q/What_are_granulocytes_and_agranulocytes [Last accessed on 2012 Mar 14].
[Google Scholar]
|
| 63. |
Sano K, Hashimoto T, Kimura K, Ozeki S. A rare nodular fasciitis involving the finger: A case report. Hand (N Y) 2009;4:327-9.
[Google Scholar]
|
| 64. |
Venugopal SS, Murrell DF. Diagnosis and clinical features of pemphigus vulgaris. Dermatol Clin 2011;29:373-80.
[Google Scholar]
|
| 65. |
Gharami RC, Kumar P, Mondal A, Ghosh K. Dyshidrosiform Pemphigus vulgaris: Report of an unusual case. Dermatol Online J 2010;16:10.
[Google Scholar]
|
| 66. |
Derm 101. In: Ackerman AB, Böer A, Bennin B, Gottlieb GJ, editors. Histologic Diagnosis of Inflammatory Skin Diseases (An Algorithmic Method Based on Pattern Analysis). Algorithm seven. Available from: http://derm101.com/content/14822 [Last accessed on 2012 Jun 20].
[Google Scholar]
|
| 67. |
Clouston D, Hall A, Lawrentschuk N. Penile lichen sclerosus (balanitis xerotica obliterans). BJU Int 2011;108:14-9.
[Google Scholar]
|
| 68. |
Sehgal VN, Srivastava G. Chancroid: Contemporary appraisal. Int J Dermatol 2003;42:182-90.
[Google Scholar]
|
| 69. |
Cassarino DS, Derienzo DP, Barr RJ. Cutaneous squamous cell carcinoma: A clinicopathologic classification--part two. J Cutan Pathol 2006;33:261-79.
[Google Scholar]
|
| 70. |
Cassarino DS, Derienzo DP, Barr RJ. Cutaneous squamous cell carcinoma: A comprehensive clinicopathologic classification. Part one. J Cutan Pathol 2006;33:191-206.
[Google Scholar]
|





