Translate this page into:
Assessing the impact of childhood and adolescent chronic plaque psoriasis on parents/caregivers using the Family Dermatology Life Quality Index (FDLQI): A cross-sectional study
Corresponding author: Dr. Tarun Narang, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. narangtarun@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Bhandari A, Narang T, Panjiyar R, Dogra S, Handa S. Assessing the impact of childhood and adolescent chronic plaque psoriasis on parents/caregivers using the Family Dermatology Life Quality Index (FDLQI): A cross-sectional study. Indian J Dermatol Venereol Leprol. 2025;91:287-93. doi: 10.25259/IJDVL_631_2023
Abstract
Background
Chronic childhood diseases are a burden for paediatric patients and their caregivers. Limited data are available on the effect of paediatric psoriasis on the caregiver’s well-being and quality of life.
Objective
To assess the impact of childhood and adolescent chronic plaque psoriasis on parents/caregivers quality of life.
Methods
A single-centre cross-sectional study was performed which included 102 children with psoriasis and their caregivers. Clinico-demographic data of children and socio-demographic details of primary caregivers were collected. Out of pocket expenditure for treatment was calculated for all the patients. The quality of life of children was assessed using the Children’s Dermatology Life Quality Index (CDLQI) and the caregiver’s quality of life was assessed using the Family Dermatology Life Quality Index (FDLQI).
Results
CDLQI was impaired in 85.29 % of children with a median score of 7. The item ‘symptoms’ was most commonly affected (87.2%), followed by ‘self-conscious’ (70.5%) and ‘treatment’ (65.6%). FDLQI was impaired in 96.1% of caregivers with a median value of 11. The most affected FDLQI items were ‘emotional’ in 95%, followed by ‘time-spent’ in 78.4%. Almost 40% of patients had catastrophic health expenditure (CHE) and their FDLQI was significantly higher (p−0.014) compared to caregivers who did not experience catastrophic health expenditure. FDLQI had a positive relationship with the involvement of exposed body sites (p−0.003), CDLQI (p−0.000), treatment expense (p−0.031) and a negative correlation with duration of illness (p−0.04).
Conclusion
Childhood psoriasis has a negative impact on the quality of life of the children and caregivers highlighting the need for intervention strategies for both.
Keywords
Childhood psoriasis
CDLQI
FDLQI
catastrophic health expenditure
Introduction
Chronic childhood skin diseases like psoriasis require prolonged treatment and multiple visits to the hospital can have a considerable impact on the psychological and social health of children and their caregivers.1 About 33% of psoriasis patients develop the disease in the first two decades of life. Incidence increases with age and is reported to be 0.55% in the first decade and 1.37% in the second decade of life.2,3 Caregivers are often anxious and stressed about the future of their child and it has a deep impact on the physical, functional and psychosocial aspects of their lives.4,5 The psychosocial impact of the disease and the continuous care it demands may in turn affect the care rendered by caregivers for the child. Basra & Finlay developed the Family Dermatology Life Quality Index (FDLQI) to assess the impact of a patient’s dermatologic condition on family members’ quality of life (QoL).6,7 The present study estimates the impact of childhood and adolescent chronic plaque psoriasis on cohabitating first-degree caregivers and identifies the level and domains in which the lives of children and their family members are affected.
Methods
A cross-sectional study was performed to investigate the impact of paediatric psoriasis on the quality of life of affected children and their primary caregivers. Approval was obtained from the institutional ethics committee (Ethical reference number: NK/7152/Study/106). Patients with psoriasis suffering for ≥6 months, aged 4–16 years and their attending primary caregivers aged ≥18 years who presented to the dermatology out-patient department between July 2021 and June 2022 were enrolled after written informed assent and consent were provided by the patients and caregivers, respectively. The sample size of 168 was calculated using the formula [N = z2*p*(1−p)/d2)] with ‘N’ being the sample size, z of 1.96 for 95% confidence interval, prevalence (p) of 12.5% and margin of error (d) of 5%; however, 102 patients and caregivers agreed to participate during the study period.8 Caregivers were excluded if they did not live in the same household or reported having any skin diseases or other significant illnesses that could affect their quality of life.
Data regarding patient’s characteristics like age, sex, education, duration of illness, treatment received and response to the treatment, history of relapse, family history of psoriasis, comorbidities, site of involvement, nail and joint involvement and treatment expense were recorded along with the socio-demographic details of the primary caregiver. Expenses were considered catastrophic when annual treatment expenditure was greater than 10% of annual income.9 Response to treatment with current therapy was patient-reported and arbitrarily considered to be minimal, moderate and good. The severity of psoriasis was assessed based on the body-surface-area (BSA) affected and the psoriasis area severity index (PASI).
The impact of psoriasis on the QoL of the children over the last week was determined by using the Children’s Dermatology Life Quality Index (CDLQI).10 The cartoon format and text-only format were used for younger children and older children, respectively. Similarly, the validated English and Hindi (local language) versions of the FDLQI questionnaire were used to assess the QoL of caregivers over the last month.6 The CDLQI and FDLQI forms were provided to the patient and caregiver and questions were explained to them in a quiet area. Younger children who were unable to complete the form by themselves were assisted by parents.
Both scales are self-reporting 10-item questionnaires used to assess the impact of skin disease on the QoL with a scoring range from 0 to 30. Higher scores represent greater impairment in the QoL. Each question is scored from 0 to 3 points and requires one response from four separate options, i.e., not at all/not relevant with a score given 0; a little with a score given 1; quite a lot with a score given 2; very much with a score given 3. Final scores are calculated by the sum of ten items. A score between 0 and 1 was considered to have no effect, a score between 2 and 6 was considered to have a small effect, a score between 7 and 12 was considered to have a moderate effect, a score between 13 and 18 was considered to have a very large effect and a score between 19 and 30 was considered to have an extremely large effect.
In the descriptive statistics mean, standard deviation (SD), median, frequency and ratio values were calculated. The normality of distribution of variables was measured with the Kolmogorov–Smirnov test. The Mann–Whitney test and Kruskal–Wallis test were used to analyse differences between independent samples. Spearman’s correlation analysis was used for correlations. Chi-square was used for the association between ordinal variables. Multiple linear regression was used to analyse factors affecting dependent continuous variables. P-values <0.05 were considered statistically significant. The statistical analyses were performed using IBM SPSS Statistics for Windows, version 23(IBM Corp., Armonk, N.Y., USA).
Results
A total of 102 patients (65 boys, 37 girls) and their caregivers participated during the study period. Median age of children was 13 with an interquartile range (IQR) of 9–16 years, while the median age of caregivers was 29 (IQR 25–32). Sixty-two of them were mothers and forty were fathers of the affected children. Median duration of illness was 3 years (IQR 1.5–4), median percentage body-surface-area of involvement was 5 (IQR 2–10) and median PASI score was 3.4 (IQR 2.2–6.9) [Table 1]. Joint involvement was present in 12 (11.7%) children. Forty-one (40.2%) patients reported good response to treatment, 38 (37.2%) reported moderate response, 21(20.6%) reported minimal response and 2 (1.9%) reported no response to the current drug therapy. Thirty-nine (38.2%) patients received systemic therapy and the rest received topical therapy. In the systemic treatments, fifteen (14.7%) patients received methotrexate, fourteen (13.7%) acitretin, four (3.9%) apremilast and three (2.9%) were treated with cyclosporine.
| Patients | Family members |
|---|---|
|
Gender Male: 65 Female: 37 |
Relationship Father: 40 Mother: 62 |
|
Age (years): Mean: 12.05 ± 3.6 Median: 13 (IQR 9–16) Range: 4–16 |
Age (years): Mean: 29.60 ± 5.30 Median: 29 IQR (25–32) Range: 22–46 |
|
Education Pre-Primary: 6 Primary: 24 Middle School: 28 High school: 21 Higher Secondary: 23 |
Education Illiterate: 4 Can read and write: 23 High school: 26 Graduate: 40 Post-graduate: 9 |
|
Duration of illness (years) Mean: 3.43 Median: 3 (IQR 1.5–4) Range: 0.5–15 |
Occupation Housewife 52 Daily-wager 8 Private job 17 Government job 12 Business 13 |
|
PASI Mean: 6.38 ± 7.66 Median: 3.4 (IQR 2.2–6.9) Range: 1.2–41.8 |
|
|
BSA Mean: 10.84 ± 15.49 Median: 5 (IQR 2–10) Range: 1–70 |
|
| Exposed area affected 68 | |
| Nail Involvement 39 | |
| Joint Involvement 12 | |
|
CDLQI Mean: 9.50 ± 8.34 Median: 7 (IQR 2–15.25) Range: 0–29 |
FDLQI Mean: 12.08 ± 8.31 Median: 11 (IQR 4–19) Range: 1–30 |
IQR: Inter quartile range, PASI: Psoriasis area severity index, BSA: Body surface area, CDLQI: Children’s dermatology life quality index, FDLQI: Family dermatology life quality index.
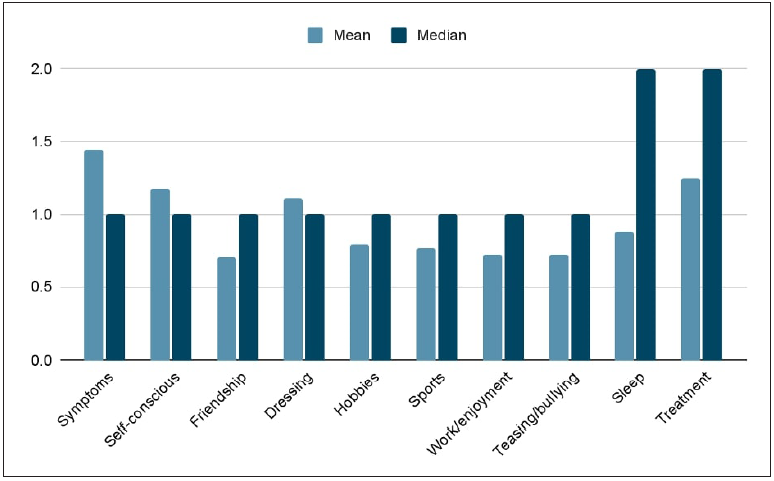
Overall, 87 (85.29%) children had impairment in the CDLQI (represented by a score of ≥2). Children had a median CDLQI of 7 with a range of 0–29 (IQR 2–15.2). Small effect on CDLQI was seen in 35 (34.3%) patients, followed by an extremely large effect in 19 (18.6%) patients [Table 2]. CDLQI n items such as ‘symptoms’ in 89 (87.2%), followed by ‘self-conscious’ in 72 (70.5%) and ‘treatment’ in 67 (65.6%) were the most affected domains. ‘Schooling/work’ was affected in 37 (36.2%) children [Figure 1].
| Severity strata | CDLQI score (n) % | FDLQI score (n) % |
|---|---|---|
| No effect (0–1) | 15 (14.7) | 4 (03.9) |
| Small effect (2–6) | 35 (34.3) | 31 (30.3) |
| Moderate effect (7–12) | 17 (16.6) | 21 (20.5) |
| Very large effect (13–18) | 16 (15.6) | 20 (19.6) |
| Extremely large effect (19–30) | 19 (18.6) | 26 (25.4) |
CDLQI: Children’s dermatology life quality index, FDLQI: Family dermatology life quality index.

- Children’s Dermatology Life Quality Index (CDLQI) items’ frequency in the study population.
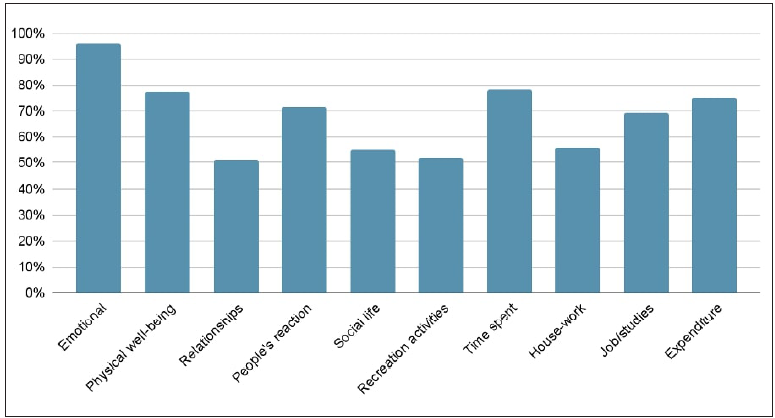
Item ‘symptoms’ had the highest mean (1.44 ± 0.96) score among all the CDLQI items, while schooling/work had a mean score of 0.62 ± 0.99. The median scores were the highest for sleep and treatment items with a value of two for both [Figure 2]. Comparison of male with female patients and of those aged ≤10 with more than 10 showed no statistically significant differences in the CDLQI scores.
- Mean/median Children’s Dermatology Life Quality Index (CDLQI) scores of individual items.
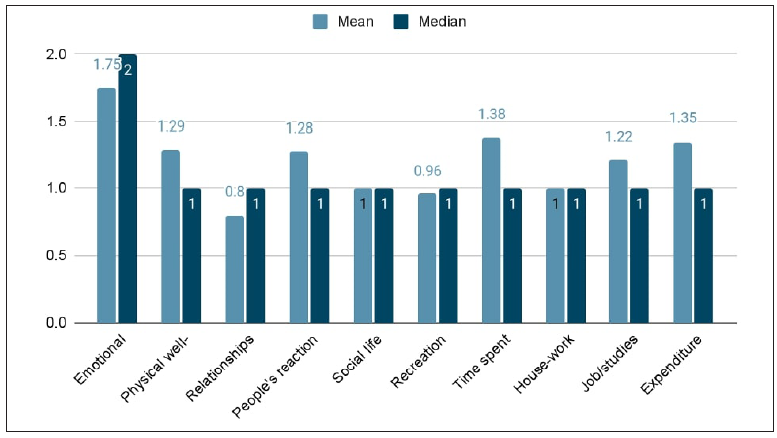
FDLQI was impaired in 98 (96.1%) caregivers (represented by a score of ≥2). The Median FDLQI score was 11 (IQR 4–19). Small effect was seen in 31 (30.3%) caregivers followed by extremely large effect in 26 (25.4%). Most affected FDLQI items were ‘emotional’ in 97 (95%), followed by ‘time spent’ in 80 (78.4%) and ‘physical well-being’ in 79 (77.4%) caregivers [Figure 3]. The highest score was with the emotional item of FDLQI (mean −1.75 ± 0.88; median −2), followed by ‘time spent/ burden of care’ (mean 1.38 ± 1.01; median −1) [Figure 4].
- Individual item frequency of Family Dermatology Life Quality Index (FDLQI) in caregivers.
- Mean/median Family Dermatology Life Quality Index (FDLQI) scores of individual items. (One is the median value score of FDLQI questionnaire, similarly 2 is the median value score of emotional questionnaire. Median value scores are represented with dark color bars and mean value scores are represented with light color bars. Hence they are actually scores.)
A statistically significant correlation was noted between the overall CDLQI score and the overall FDLQI score (p–0.001; rs = 0.790). The Median FDLQI for male children was 11, while for female children it was 9. Similarly, the median CDLQI for the male and female children was 7 and 9 respectively and the differences in the median of FDLQI (p-0.793) and CDLQI (p-0.736) was not significant. The median score of FDLQI in mothers versus fathers was not found to be significant (p-0.717).
PASI had a significant correlation with overall CDLQI score [p-0.001; rs (spearman correlation coefficient) = 0.549] and FDLQI score (p-0.001; rs = 0.609). Similarly, joint involvement correlated significantly with nail involvement (p–0.031; rs = 0.214), CDLQI (p-0.007; rs = 0.196) and FDLQI (p-0.049; rs = 0.196). However, nail involvement did not correlate significantly with CDLQI and FDLQI. Joint involvement was associated with a significant impairment in the CDLQI domains of ‘self-consciousness’ (χ2 - 11.07, p-0.01), ‘hobbies’ (χ2 - 16.82, p-0.01) and ‘sports’ (χ2 - 11.79, p-0.08). Median FDLQI scores of caregivers with children having joint involvement was 19 (IQR 8–24.5) and for those without joint involvement was 9.5 (IQR 4–18); however, scores could not reach a significant difference between the two groups (p-0.32).
Duration of illness had a negative correlation with CDLQI (p-0.16; rs = −0.13) and FDLQI (p-0.185; rs = −0.19) scores but wasn’t found to be statistically significant. Higher treatment expenditure had a significant positive correlation with overall FDLQI score (p-0.000; rs = 0.483). Median yearly income of the caregivers was 2,40,000 rupees (2941.7USD) approximately and median yearly expenditure was 1,80,000 rupees (2206.2USD) approximately, while median yearly treatment expenditure was 18,500 rupees (226.7USD) approximately. Catastrophic health expenditure was seen in 41 (40.1%) patients and their FDLQI was significantly higher (p-0.014) in comparison to caregivers who did not experience catastrophic health expenditure [Figure 5].
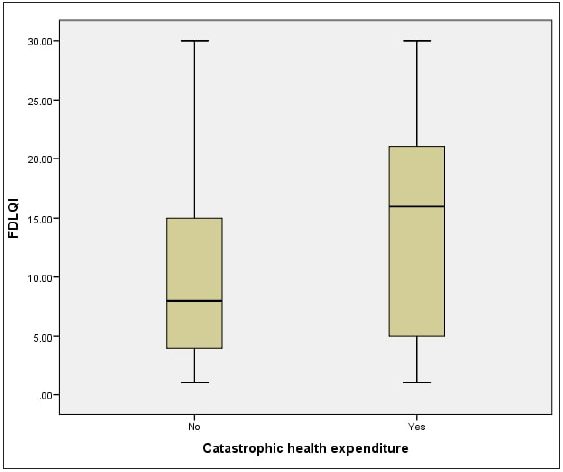
- Distribution of Family Dermatology Life Quality Index (FDLQI) with catastrophic health expenditure.
The median distribution of CDLQI was not significantly different among children with the involvement of exposed and non-exposed body sites. However, median distribution of FDLQI was significantly higher in caregivers whose children had involvement of exposed body sites (p-0.003). Higher FDLQI scores were noted in caregivers of children who received systemic drugs compared to those who received only topical treatment (p-0.008). However no significant difference in FDLQI was noted among different oral drugs. Response to treatment had a negative correlation with FDLQI (p-0.001; rs = −0.333); however, this did not meet significance on linear regression.
Multiple linear regression analysis revealed a positive correlation of FDLQI with exposed body sites affected (p-0.003), CDLQI (p-0.000), treatment expense (p-0.031) and negative relation with duration of illness (p-0.04) [Table 3].
| Coefficientsa | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | Unstandardised coefficients | Standardised coefficients | t | P-value | Collinearity statistics | |||
| B | Std. error | Beta | Tolerance | VIF | ||||
| 1 | (Constant) | 9.211 | 3.603 | 2.557 | 0.012 | |||
| Patient’s age | −0.224 | .271 | −0.098 | −0.825 | 0.412 | 0.223 | 4.486 | |
| Patient’s gender | 1.418 | 1.064 | 0.082 | 1.334 | 0.186 | 0.828 | 1.208 | |
| Duration of illness | −0.433 | 0.210 | −0.138 | −2.062 | 0.042 | 0.702 | 1.425 | |
| Response to treatment | −0.774 | 0.708 | −0.071 | −1.093 | 0.277 | 0.718 | 1.392 | |
| Nail involvement | −0.383 | 1.078 | −0.022 | −0.355 | 0.724 | 0.788 | 1.268 | |
| Exposed area affected | 2.977 | 0.956 | 0.180 | 3.116 | 0.003 | 0.846 | 1.182 | |
| BSA | −0.040 | 0.076 | −0.075 | −0.533 | 0.595 | 0.158 | 6.326 | |
| PASI | 0.177 | 0.145 | 0.163 | 1.225 | 0.224 | 0.178 | 5.615 | |
| CDLQI | 0.616 | 0.087 | 0.619 | 7.092 | 0.000 | 0.415 | 2.408 | |
| Caregiver gender | −1.385 | 1.581 | −0.082 | −0.876 | 0.383 | 0.363 | 2.753 | |
| Caregiver education | −0.840 | 0.615 | −0.104 | −1.366 | 0.176 | 0.541 | 1.847 | |
| Occupation | 0.104 | 0.516 | 0.019 | 0.201 | 0.841 | 0.367 | 2.727 | |
| Treatment expense | 0.001 | 0.000 | 0.149 | 2.198 | 0.031 | 0.685 | 1.461 | |
a. Dependent Variable: FDLQI; * Values in bold are significant; VIF: Variance inflation factor, BSA: Body surface area, PASI: Psoriasis area severity index, CDLQI: Children’s dermatology life quality index, FDLQI: Family dermatology life quality index, B: Its just a way of representing unstandardised coefficient.
Discussion
Of the 102 patients enrolled, 85.29 % of children had impairment in the CDLQI scores due to psoriasis. As a secondary impact, 96.1% of caregivers reported impairment in FDLQI scores. The median scores of PASI, CDLQI and FDLQI were 3.4, 7 and 11, respectively. The ‘emotional distress’ was the most affected FDLQI item, followed by ‘time spent/burden of care’ and ‘physical well-being’. In the CDLQI , the item ‘symptoms’ was most affected, followed by ‘self-consciousness’ and ‘treatment’ items. The FDLQI score had a significant correlation with CDLQI and PASI. We observed that the PASI correlated well with CDLQI scores; this has also been shown by other studies.11,12
In an Australian study, similar results were observed where the median PASI was 4.2, median FDLQI was 12 and the correlation coefficient between PASI and FDLQI was 0.44 (P-0.001). However, unlike our study in which the item ‘emotional’ was most impacted with highest mean, they found ‘burden of care’ to be the most affected item with a mean value of 2.05, followed by the item ‘emotional’ having a mean value of 1.54.13
A multicentre study from Turkey observed a median CDLQI score of 6 (IQR 0–24); ‘symptoms’ and ‘feelings’ were the most severely impaired domains of the CDLQI and ‘emotions’ was the most severely impaired domain of the FDLQI.7 Likewise, Tollefson and colleagues found the item ‘emotional’ to be the most impaired among the FDLQI. These results were in consonance with our findings.4
Our study did not find a significant difference in the mean scores of CDLQI and FDLQI for male versus female children or between children ≤10 years versus >10 years.7,14 Similarly, the median FDLQI scores of mothers and fathers were not significantly different for male versus female children. However, Tekin et al. found a greater QoL impairment in caregivers of boys than in caregivers of girls proposing mothers may be more ‘attached’ and worried about their sons owing to cultural practices.7 Zychowska et al. found mothers to have a significantly higher impact on domains of emotions, people’s reactions, social life, time spent, housework and overall FDLQI scores than fathers. These findings were explained based on mothers having a higher emotional attachment with children as they are more involved during illness and daily routine care, resultantly spending extra time with them.14 Salman et al. categorised children into age groups ≤12 years and >12 years; however, similar to our study, they found no significant difference in the median PASI, duration of disease, CDLQI and FDLQI scores.15
Joint involvement significantly affected the quality of life of patients and caregivers and made children more self-conscious about the disease. The FDLQI scores of caregivers of children with joint involvement and without joint involvement were not found to be significantly different in our study, possibly due to a smaller sample size of children with joint involvement. Meneghetti et al. found the CDLQI scores to be significantly higher in children with musculoskeletal involvement and the risk of impaired health-related quality of life (HRQoL) was eight times higher in the presence of musculoskeletal pain.16 Ganemo et al. found children with joint complaints having higher Dermatitis Family Impact (DFI) scores.17
We observed higher FDLQI scores when the children received systemic drugs compared to only topical treatment. However, they were likely to have more severe disease involvement as reported by others too.13 Treatment expense was found to have a significant linear correlation with FDLQI scores. Considering India is a low-income country with an under-penetration of insurance, most of the treatment expenditure is out-of-pocket. Hence, unlike other studies, we performed a cost analysis and found that 40% of the households experienced catastrophic health expenditure. The FDLQI correlation with treatment expense was stronger with caregivers experiencing catastrophic health expenditure. Psoriasis treatment imposes a significant financial burden on the families of the patients; however, chronic skin diseases such as psoriasis are not given due importance in India’s national health care policies. In order to reduce the economic burden related to health expenditure, treatment may require government support under community-based health insurance schemes to improve standard of care as well as the quality of life of patients and caregivers.18,19
The involvement of visible body sites can affect social life and inflict psychological morbidity in children and caregivers.20 Significantly higher FDLQI scores were observed in caregivers whose children had involvement of exposed body sites in comparison to children only with involvement of unexposed sites. However, CDLQI was not significantly different between the two groups.20 Tekin et al. found a higher CDLQI score in patients with scalp involvement than those without scalp involvement, but not statistically significant (P-0.138). Scalp involvement leads to difficulty in combing and easy visibility of scales over the clothes, impacting the psychosocial well-being of a child.7
There is a higher prevalence of stigma, anxiety and depression among caregivers of patients with psoriasis.5,21 CDLQI and FDLQI indirectly assess the severity of the patient’s disease and may help in the early identification of the mental status of the patient and caregiver. Hence, early evaluation of children’s quality of life may help provide better treatment and psychological support for the children and the caregivers.22
Limitation
This study had a small sample size and psychological morbidity was not assessed.
Conclusion
Psoriasis has a deleterious effect on the psycho-social aspects of quality of life of children and their caregivers. The items ‘emotional’ followed by ‘burden of care’ were the most impacted and most affected among Family Dermatology Life Quality Index. Education and counselling about the disease may help in improving the quality of life of patients and caregivers.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at Postgraduate Institute of Medical Education and Research, Chandigarh, number NK/7152/Study/106, dated 12th March 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Care for children with severe chronic skin diseases. Eur J Pediatr. 2019;178:1095-103.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and treatment of psoriasis in the United Kingdom: A population-based study. Arch Dermatol. 2005;141:1537-41.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and comorbidity of psoriasis in children. Br J Dermatol. 2010;162:633-6.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of childhood psoriasis on parents of affected children. J Am Acad Dermatol. 2017;76:286-289.e5.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing depression and anxiety in the caregivers of paediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The family dermatology life quality index: Measuring the secondary impact of skin disease. Br J Dermatol. 2007;156:528-38.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of quality of life in turkish children with psoriasis and their caregivers. Pediatr Dermatol. 2018;35:651-9.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of childhood psoriasis: A study of 419 patients from northern India. Int J Dermatol. 2004;43:654-8.
- [CrossRef] [PubMed] [Google Scholar]
- Catastrophic Health Spending and Impoverishment of Households While Seeking Hospital Treatment of Children (0–4 years) in India. Available from: https://www.niti.gov.in/catastrophic-health-spending-and-impoverishment-households-while-seeking-hospital-treatment. Accessed Dec 22, 2022.
- The children’s dermatology life quality index (CDLQI): Initial validation and practical use. Br J Dermatol. 1995;132:942-9.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of treatments in daily clinical practice on the children’s dermatology life quality index in juvenile psoriasis: A longitudinal study from the child-CAPTURE patient registry. Br J Dermatol. 2012;167:145-9.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of psoriasis on quality of life of children and their caregivers: An Italian experience. Eur J Dermatol. 2021;31:649-50.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between PASI and FDLQI in pediatric psoriasis, and treatments used in daily clinical practice. Australas J Dermatol. 2021;62:190-4.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of childhood psoriasis on caregivers’ quality of life, measured with family dermatology life quality index. Acta Derm Venereol. 2020;100:adv00244.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of psoriasis in the quality of life of children, adolescents and their families: A cross-sectional study. An Bras Dermatol. 2018;93:819-23.
- [CrossRef] [PubMed] [Google Scholar]
- The musculoskeletal impairment negatively impacts the quality of life of children and adolescents with psoriasis. Adv Rheumatol. 2020;60:33.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and clinical features in Swedish children with psoriasis. Pediatr Dermatol. 2011;28:375-9.
- [CrossRef] [PubMed] [Google Scholar]
- Disease-specific out-of-pocket payments, catastrophic health expenditure and impoverishment effects in India: An analysis of national health survey data. Appl Health Econ Health Policy. 2021;19:769-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparative assessment of economic burden of disease in relation to out of pocket expenditure. Front Public Health. 2019;7:9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of psoriasis with psychiatric hospitalization in United States Children and Adults. Dermatol (Basel Switz). 2019;235:276-86.
- [Google Scholar]
- Stigma experienced by the caregivers of patients with chronic plaque psoriasis. Indian Dermatol Online J. 2021;12:110-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life in persons living with psoriasis patients. J Am Acad Dermatol. 2014;71:302-7.
- [CrossRef] [PubMed] [Google Scholar]






