Translate this page into:
Association between high-risk human papillomavirus and cervico-vaginal infections in tribal women screened for cervical precancers and cancers in Maharashtra, India: A cross-sectional study
Corresponding author: Dr. Anushree Patil, Department of Clinical Research, ICMR-National Institute for Research in Reproductive and Child Health (NIRRCH), Mumbai, Maharashtra, India. patila@nirrch.res.in
-
Received: ,
Accepted: ,
How to cite this article: Munne KR, Birje S, Patil AD, Akula A, Mayekar A, Bhekare G, et al. Association between high-risk human papillomavirus and cervico-vaginal infections in tribal women screened for cervical precancers and cancers in Maharashtra, India: A cross-sectional study. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1501_2024
Abstract
Background
The vaginal microenvironment is thought to impact infection and persistence of the human papillomavirus which is a necessity for cervical carcinogenesis. Tribal women are at risk for human papillomavirus and cervicovaginal infections due to polygamy, poor hygiene, and illiteracy.
Aims
We evaluated the association of common cervico-vaginal infections with human papillomavirus infection and cervical precancers among the tribal women of Dahanu taluka, Maharashtra, India.
Methods
For this cross-sectional study, tribal women from Dahanu taluka were recruited. Cervical brushing samples were collected from them and tested for human papillomavirus by the Hybrid Capture 2 method and polymerase chain reaction for Chlamydia trachomatis. Vaginal samples were collected for gram staining and examined for candidiasis and bacterial vaginosis, followed by visual inspection of the cervix with acetic acid.
Results
A total of 501 sexually active tribal women were recruited, among whom the human papillomavirus infection rate was 6.5%. Evaluation of vaginal smears by Nugent’s scoring revealed bacterial vaginosis in 208 (41.5%), candidiasis in 30 (5.98%), and chlamydia in five (1%) participants. Bacterial vaginosis prevalence was higher in high-risk human papillomavirus-positive women. The presence of clue cells was associated with human papillomavirus positivity, suggesting an association between bacterial vaginosis and human papillomavirus infection and indicating an increased risk of human papillomavirus infection on co-infection with bacterial vaginosis.
Limitations
Only tribal women were screened, with no screening for other sexually transmitted infections. Since participants were recruited from healthcare centres instead of random sampling, this may have affected infection rate estimates. Due to regional differences in sexual behaviours and gynaecological morbidities, our findings cannot be generalised to tribal women from other regions.
Conclusion
Early detection and management of reproductive tract and sexually transmitted infections is paramount for preventing co-infections and reduces the risk of cervical carcinogenesis.
Keywords
Cervico-vaginal infections
HPV
tribal
India
cervical cancer
Introduction
Cervical cancer (77,348 deaths; 9.1%) succeeds breast cancer (90,408 deaths; 10.6%) with regards to mortality among Indian women.1 While persistent high-risk oncogenic human papillomavirus infection is essential for cervical carcinogenesis, risk factors like overconsumption of contraceptive pills, tobacco, sexually transmitted pathogens, gene polymorphisms in antigen-processing proteins, host genetic/immunologic responses, lifestyle factors, low socio-economic status, immunosuppression, and poor genital hygiene can exacerbate the risk. Although few women develop persistent human papillomavirus infection, most infections appear to be transient.2–5 Primary screening methods like visual inspection with acetic acid, Pap smear, and human papillomavirus DNA assay are used to detect human papillomavirus and cervical intraepithelial neoplasia.
Apart from human papillomavirus, reproductive tract (RTI) and sexually transmitted infections (STI) like Chlamydia, Candidiasis, and bacterial vaginosis are important factors for cervical carcinogenesis. Recurrent inflammation can result in cellular proliferation and shedding of epithelium, leading to the growth of malignant clone of cells, with cytokines, chemokines, free radicals, and growth factors helping in the colonisation of microbes.6 Cells become malignant if the pathogenic genetic material integrated within them evades normal cell cycle control mechanisms. Studies have highlighted the connection between human papillomavirus and these infections towards the progression of cervical intraepithelial neoplasia. While a study from Karnataka observed candidiasis and bacterial vaginosis in 6.1% and 2.5% tribal women,7 a West Bengal study noted 88.6% and 14.3% prevalence of Candidiasis and Chlamydia in human papillomavirus-infected female sex workers.8 Co-existence of these three infections with human papillomavirus was seen in 6.2% women in Mumbai.9
With a population of 104,281,034 (8.6%), 705 tribes and 75 particularly vulnerable tribal groups, the indigenous tribal groups (Adivasis) are designated as Scheduled Tribes by the Constitution of India.10 While Maharashtra has 9.4% (10 million) of the Scheduled Tribes population, Palghar district in Maharashtra has 37.4% population belonging to the Warli, Katkari, and Malhar Koli tribal groups.11 A rift between tribal and non-tribal population regarding healthcare exists due to barriers like discrimination, exclusion, social norms, and values, prejudice, and intolerance.11–13 Widespread poverty, illiteracy, malnutrition, polygamy, poor hygiene, delayed health-seeking behaviour and ineffective coverage of communication, transportation, and national health facilities are possible co-factors for dismal health conditions among Indian tribals.11,13 We reported the openly condoned yet highly prevalent polygamy among tribal men and women.11 The subcultures with relaxed marital institution or tolerance for high-risk sexual practices like polygamy due to faulty perceptions are vulnerable to various reproductive tract/sexually transmitted infections.14
Although the association between human papillomavirus and co-infections in cervical cancer has been explored, very few studies have explored this subject among vulnerable tribal women. This study aims to understand the prevalence, co-infection, and association of risk factors between human papillomavirus and RTI/STIs like Chlamydia, bacterial vaginosis, and Candidiasis among tribal women in Palghar.
Methods
Recruitment of study participants
This cross-sectional study was approved by the Institutional Ethics Committee for Human Studies (D/ICEC/Sci-150/159/2019) and was conducted in healthcare centres in a tribal block of Dahanu taluka in the Palghar district of Maharashtra, India, from December 2020 to October 2022. Sexually active women aged 30–59 who had not undergone hysterectomy or cervical cancer screening were included in the study, while women who were pregnant or menstruating or had an abortion or delivery in the past three months were excluded from the study. Menstruating women were allowed to participate after the seventh day of menstruation. The participants were enrolled after counselling them and obtaining their written consent. The study questionnaire used permitted information on identification and socio-demographic details, menstrual-obstetric-sexual-contraception history, genital hygiene, and gynaecological complaints.
Collection of patient samples
Three samples were collected: (1) vaginal smear for Gram’s staining, (2) cervical brushing sample in sample transport medium (Digene HC2 DNA Collection Device, 990332) for human papillomavirus DNA testing using Hybrid Capture 2 test (HC2, Qiagen, Germantown, MD, USA) and (3) cervical swab for polymerase chain reaction detecting Chlamydia trachomatis, followed by visual inspection with acetic acid.
Laboratory investigations
Gram’s staining for screening reproductive tract/sexually transmitted infections
Gram’s staining (HiMedia Gram’s Stains-Kit, K001-1KT) was performed for vaginal smears to diagnose bacterial vaginosis and candidiasis, as described in the National AIDS Control Organisation guidelines. Bacterial vaginosis was diagnosed using Nugent’s score and clue cells. Gram-stained smears were examined and graded as per the morphological classification developed by Nugent, as per the scoring of different morphotypes such as lactobacillus, Mobiluncus, and Gardnerella vaginalis. Total score of ≥ 7 was considered positive for bacterial vaginosis, 4–6 as intermediate, and ≤ 3 as normal. Gram-stained smears of vaginal discharge were examined for pus cells and clue cells. Vaginal candidiasis was diagnosed based on the presence of pseudohyphae and/or budding yeast cells. Women who were screened positive were referred to the collaborating tertiary cancer care centre for further management.
Human papillomavirus DNA detection using Hybrid Capture 2 test
The Hybrid Capture 2 specimen was stored at 4 ̊C until the assay was performed. The Hybrid Capture 2 assay involves nucleic acid hybridisation (formation of DNA-ribonucleic acid hybrids) with signal amplification utilising microplate chemiluminescent detection, thereby enabling detection of 13 high-risk human papillomavirus types (human papillomavirus 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68). The assay was performed according to the manufacturer’s instructions.
Extraction of DNA using QIAamp DNA mini kit
Cervical swab samples were utilised for the extraction of DNA for the Chlamydia trachomatis polymerase chain reaction. These samples were stored at –20 ̊C until extraction. QIAamp DNA Mini Kit (Qiagen, Germantown, MD, USA, 56304) was used for DNA extraction. The quality and quantity of extracted DNA was checked using a spectrophotometer (BioTek, Model: EPOCH2C).
Polymerase chain reaction and Southern blotting for Chlamydia trachomatis
The extracted DNA was used to detect Chlamydia trachomatis by indigenous polymerase chain reaction assay (Chlamydia trachomatis – National Institute for Research in Reproductive Health).15 Polymerase chain reaction was performed using extracted DNA and primers designed from the conserved region of the major outer membrane protein gene of Chlamydia trachomatis (designed by Sigma). The amplified products were run on 2% Agarose gel (Genei, Catalogue Number 105193) and observed under an ultraviolet transilluminator (Biorad ChemiDoc MP Imaging System, 12003154) [Figure 1]. The presence of 200 bp repeat sequences in other clinical specimens indicated the presence of Chlamydia trachomatis infection. Further confirmation of these amplified products was done using a specific Chlamydia trachomatis probe (Roche DIG Oligonucleotide 3’ End Labelling Kit, 2nd generation, 03353575910, Roche polymerase chain reaction DIG Probe Synthesis Kit, 11636090910, Roche DIG Luminescent Detection Kit, 11363514910) in Southern blotting.15,16
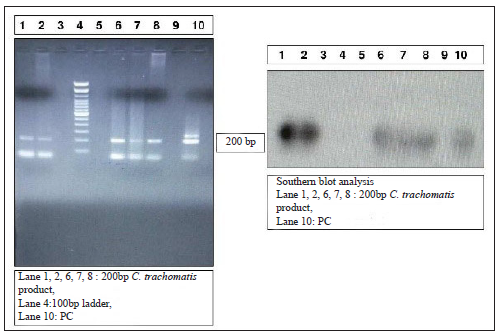
- Polymerase chain reaction and Southern blotting for C. trachomatis.
Cervical cytology by Pap smear
To understand the association of the RTI/STIs with cytological abnormalities, Pap smear findings of these participants were obtained from their Pap smear reports.
Statistical analysis
Data was entered using Microsoft Excel 2016 and analysed using SPSS version 27 (IBM, Chicago, IL, USA). Data regarding socio-demographic characteristics and variables were represented as frequency and percentage while the age of the participants were represented as median. Association between human papillomavirus and socio-demographic, sexual health, and gynaecological factors like age, marital status; cancer risk factors like consumption of alcohol and tobacco; number of sexual partners in lifetime, age at menarche and first sexual intercourse; contraception method used and RTI/STIs like Candida, Chlamydia trachomatis and bacterial vaginosis was studied using the Chi-square test (X2), wherein p-value < 0.05 was considered as statistically significant.
Results
Socio-demographic profile of study participants
Total 501 participants were enrolled. Many (264; 52.38%) were aged 30–39. Median age of the participants was 38 years between the range of 30 and 59. Four hundred and sixty-six (93.01%) were Marathi and 399 (79.64%) belonged to the Warli tribe. Three hundred and ninety-nine (79.64%) were married, 253 (50.49%) were illiterate and 223 (44.51%) were housewives. Out of the 501 participants, 361 (72.05%) belonged to the upper-lower socio-economic class, according to Kuppuswamy’s modified scale for 2020. A complete socio-demographic profile of participants is presented in Table 1.
| Socio-demographic characteristics | Frequency (n) | Percentage (%) |
|---|---|---|
| Age group | ||
| 30–39 | 264 | 52.69% |
| 40–49 | 165 | 33.00% |
| 50–59 | 72 | 14.37% |
| Study site | ||
| Primary health centre | 6 | 1.19% |
| Sub district hospital | 113 | 22.55% |
| Health and wellness centre 1 | 148 | 29.54% |
| Health and wellness centre 2 | 131 | 26.14% |
| Health and wellness centre 3 | 59 | 11.77% |
| Health and wellness centre 4 | 44 | 8.78% |
| Marital status | ||
| Married | 399 | 79.64% |
| Widow | 72 | 14.37% |
| Separated | 6 | 1.19% |
| Unmarried but sexually active | 24 | 4.79% |
| Education | ||
| Illiterate | 253 | 50.49% |
| Primary school | 62 | 12.37% |
| Middle school | 76 | 15.16% |
| High school | 82 | 16.36% |
| Intermediate | 14 | 2.79% |
| Graduate and postgraduate | 14 | 2.79% |
| Occupation | ||
| Housewife | 223 | 44.51% |
| Service | 16 | 3.19% |
| Teacher | 5 | 1.00% |
| Skilled worker | 64 | 12.77% |
| Unskilled worker | 193 | 38.52% |
| Socio-economic class | ||
| Upper (I) | 0 | 0% |
| Upper middle (II) | 36 | 7.18% |
| Lower middle (III) | 67 | 13.37% |
| Upper lower (IV) | 361 | 72.05% |
| Lower (V) | 37 | 7.38% |
Gynaecologic examination findings
While most participants did not experience any gynaecological issues (322; 64.27%), vaginal discharge was the most common complaint among 110 participants (22.08%). Complaints of lower abdominal pain, dyspareunia, and intermenstrual bleeding were reported by 28 (5.58%), four (0.79%), and one (0.19%) participants, respectively.
Prior to sample collection, the participants underwent a gynaecologic examination. Cervical polyps were observed in 31 (6.18%), cervical ectropion in 111 (22.15%), Nabothian follicles in 24 (4.79%), and leukoplakia in four (0.79%) participants, respectively.
Risk factors for RTI/STIs and cervical cancer
Among the 501 participants for whom data was analysed, 44 (8.78%) and 19 (3.79%) participants consumed smokeless tobacco and alcohol, respectively. Sanitary napkin usage was mentioned by 260 participants (51.89%). Most (384; 77.64%) participants were married at an early age (aged 11–20). While 483 (96.40%) participants had only one sexual partner, 18 (3.59%) practised polygamy, and 24 (4.79%) were unmarried yet sexually active. Among unmarried women with multiple sexual partners, seven widows out of 72 (9.72%) and three out of six participants who separated from their spouses (50%) reported two sexual partners. Almost half the participants (257; 51.29%) had a parity of more than three. Tubal ligation was the preferred contraceptive method for many participants (330; 66%). Human papillomavirus positivity was more (p-value = 0.019) in widows/separated and unmarried sexually active women than married women [Table 2]. Also, human papillomavirus prevalence was more in women, with two or more sexual partners in their lifetime.
| Variables | High-risk human papillomavirus infection | p-value | |||
|---|---|---|---|---|---|
|
Positive N (%) |
Negative N (%) |
Total N (%) |
|||
| Age | 31–40 | 14 (4.7) | 286 (95.3) | 300 (100) | 0.105 |
| 41–50 | 14 (4.7) | 131 (90.3) | 145 (100) | ||
| 51–60 | 5 (8.9) | 51 (91.1) | 56 (100) | ||
| Marital status | Married | 20 (5) | 379 (95) | 399 (100) | 0.019* |
| Widow/separated | 10 (12.8) | 68 (87.2) | 78 (100) | ||
| Unmarried sexually active | 3 (12.5) | 21 (87.5) | 24 (100) | ||
| Tobacco (any form) | Yes | 5 (11.4) | 39 (88.6) | 44 (100) | 0.181 |
| No | 28 (6.1) | 429 (93.9) | 457 (100) | ||
| Alcohol | Yes | 3 (15.8) | 16 (84.2) | 19 (100) | 0.133 |
| No | 30 (6.5) | 432 (93.5) | 462 (100) | ||
| Total number of partners in lifetime | 1 | 30 (6.2) | 453 (93.8) | 483 (100) | 0.079 |
| ≥ 2 | 3 (16.7) | 15 (83.3) | 18 (100) | ||
| Approximate age at first sexual intercourse | ≤ 17 | 15 (7.3) | 190 (92.7) | 205 (100) | 0.583 |
| > 17 | 18 (6.1) | 278 (93.9) | 296 (100) | ||
| Age at menarche | < 12 | 1 (2.9) | 33 (97.1) | 34 (100) | 0.375 |
| ≥ 12 | 32 (6.9) | 435 (93.1) | 34 (100) | ||
| Contraception method | Oral contraceptive pills | 0 | 1 (100) | 1 (100) | 0.691 |
| Intrauterine contraceptive device | 0 | 5 (100) | 5 (100) | ||
| Female sterilisation | 19 (5.8) | 311 (94.2) | 330 (100) | ||
Distribution of reproductive tract/sexually transmitted infection pathogens
The presence of high-risk human papillomavirus DNA was observed in 33 participants (6.58%) by the Hybrid Capture 2 test [Figure 2]. While a positive result for Chlamydia trachomatis polymerase chain reaction was observed in five (1%) participants, the human papillomavirus-Chlamydia trachomatis co-infection was absent. Evaluation of vaginal smears by Gram’s staining revealed bacterial vaginosis in 208 (41.51%) participants by Nugent scoring, while clue cells which are diagnostic of bacterial vaginosis were seen in 125 (25%) cases. Vaginal candidiasis was observed in 30 (5.98%) participants [Figure 3]. Co-infection of bacterial vaginosis with human papillomavirus was observed in 17 (3.39%) participants, while human papillomavirus and Candida co-infection was observed in only one (0.19%) participant.
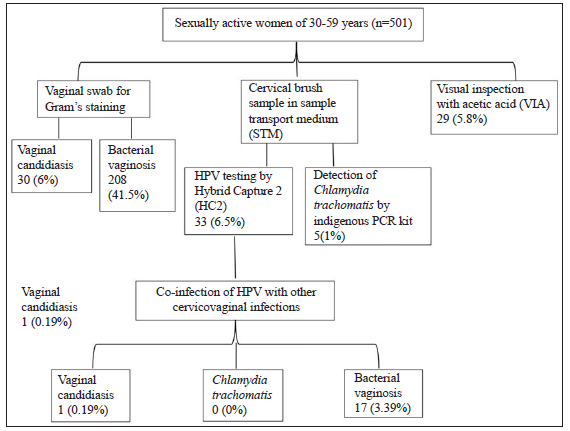
- Flow chart for screening of reproductive tract/sexually transmitted infections and cervical cancer.
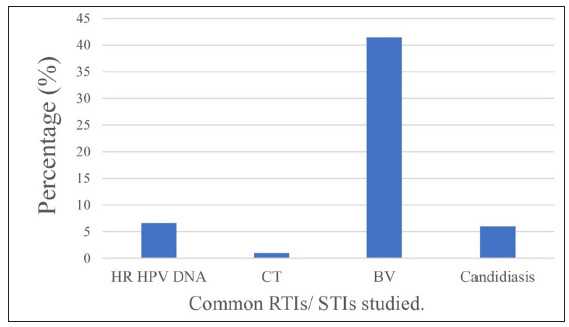
- Prevalence of reproductive tract/sexually transmitted infections among study participants. (HR: High risk; CT: Chlamydia trachomatis; BV: Bacterial vaginosis; RTIs/STIs: Reproductive tract infections/Sexually transmitted infection)
Highest prevalence of human papillomavirus and RTI/STIs was observed in the 31–40 age group. In this age group, human papillomavirus positivity was 14 (42.42%) while prevalence for other infections was as follows: four (80%) cases of Chlamydia, 18 (60%) of Candida and 124 (59.61%) of bacterial vaginosis.
We also compared the prevalence of various RTI/STIs in participants with the contraception they used. Among participants positive for RTI/STIs studied, the majority had undergone tubal ligation (65.8% for bacterial vaginosis, 66.7% for Candida, 60% for Chlamydia trachomatis, and 57.5% for human papillomavirus). Among participants diagnosed with bacterial vaginosis, only 2.4% reported usage of condoms by their male partners, 1.4% reported usage of intrauterine contraceptive device, and 0.5% used oral contraceptives. Among participants diagnosed with Chlamydia trachomatis, 20% reported usage of intrauterine contraceptive device while no participant reported usage of condoms by their male partners. None of the participants diagnosed with either Candida or human papillomavirus reported usage of oral contraceptive pills or intrauterine contraceptive device or condoms. A significant positivity for RTI/STIs among women not using any contraceptive method was observed.
Analysis of various RTI/STIs with human papillomavirus positivity is shown in Table 3. The presence of clue cells, which are diagnostic for bacterial vaginosis, were significantly associated with human papillomavirus positivity. No association was found among Candida and Chlamydia trachomatis infection with human papillomavirus positivity.
| Variables | High-risk human papillomavirus infection | p-value | ||||
|---|---|---|---|---|---|---|
| Positive N (%) | Negative N (%) | Total N (%) | ||||
| Candida | Present | 1 (3.3) | 29 (96.7) | 30 (100) | 0.472 | |
| Absent | 31 (6.7) | 434 (93.3) | 465 (100) | |||
| Chlamydia trachomatis | Positive | 0 (0) | 5 (100) | 5 (100) | 0.583 | |
| Negative | 28 (5.7) | 463 (94.3) | 491 (100) | |||
| Bacterial Vaginosis | Nugent score | Normal (≤ 3) | 9 (5.3) | 161 (94.7) | 170 (100) | 0.222 |
| Intermediate | 5 (4.2) | 113 (95.8) | 118 (100) | |||
| Bacterial vaginosis (≥ 7) | 18 (8.7) | 190 (91.3) | 208 (100) | |||
| Clue cells | Present | 15 (12) | 110 (88) | 125 (100) | 0.04* | |
| Absent | 17 (4.6) | 352 (95.4) | 369 (100) | |||
| Pus cells | Present | 19 (5.9) | 305 (94.1) | 324 (100) | 0.434 | |
| Absent | 13 (7.7) | 156 (92.3) | 169 (100) | |||
The presence of RTI/STIs and their distribution with cytological abnormalities have been analysed in Table 4. Subjects negative for human papillomavirus and RTI/STIs had a higher probability of a normal cytology. Human papillomavirus-bacterial vaginosis co-infection was observed in two participants (11.8%) with high-grade squamous intraepithelial lesion. All the participants diagnosed with Chlamydia trachomatis had normal cytological findings.
| Pathogen |
Total N (%) |
Atypical squamous cells of undetermined significance N (%) | Low-grade squamous intraepithelial lesion N (%) | High-grade squamous intraepithelial lesion N (%) | Any cytological abnormality | Negative for intraepithelial lesion or malignancy (NILM) | |
|---|---|---|---|---|---|---|---|
| 501 (100%) | 3 (0.6%) | 3 (0.6%) | 2 (0.4%) | 8 (1.6%) | |||
| Chlamydia trachomatis | 5 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 5 (100%) | |
| Candidiasis | 30 (5.98%) | 0 (0%) | 1 (3.33%) | 0 (0%) | 1 (3.33%) | 28 (93.33%) | |
| Bacterial vaginosis | 208 (41.51%) | 1 (0.48%) | 1 (0.48%) | 0 (0%) | 2 (0.96%) | 204 (98.07%) | |
| Human papillomavirus | 33 (6.58%) | 1 (3.03%) | 1 (3.03%) | 2 (6.06%) | 4 (12.12%) | 25 (76%) | |
| *Co-infection of human papillomavirus with other pathogens: | |||||||
| Human papillomavirus | Candidiasis | 1 (0.19%) | 0 (0%) | 1 (0.19%) | 0 (0%) | 1 (0.19%) | 1 (0.19%) |
| Bacterial vaginosis | 17 (3.39%) | 0 (0%) | 0 (0%) | 2 (11.8%) | 2 (11.8%) | 13 (76.47%) | |
Discussion
While reproductive tract/sexually transmitted infections (RTI/STIs) are a significant health, social, and economic problem in India due to their risk of asymptomatic presentation, tribal women are at a higher risk due to poor knowledge and dearth of health services.17 Hence, understanding the prevalence of RTI/STIs like human papillomavirus, chlamydia, bacterial vaginosis, and candidiasis among tribal women and an association between them was important.
In our study, 22.08% participants cited vaginal discharge as the most common gynaecological complaint. Our finding is higher compared to Central and eastern Indian studies where vaginal discharge was most common in 13.9% and 14.03% tribal women, respectively,17,18 and from Puducherry where 3.3% participants with vaginal discharge were diagnosed with cervical cancer in situ and invasive cervical cancers.19 While vaginal discharge is a common reason for gynaecological consultation and could be attributed to bacterial vaginosis, identifying its cause, especially infectious ones, is crucial to eliminate any underlying pathological abnormality and initiating treatment.
We noted a low prevalence rate of 6.5% for high-risk human papillomavirus infection. This contrasted with human papillomavirus prevalence among the tribal women of Karnataka, India (40.6%, diagnosed by polymerase chain reaction).20 This could be due to the overall declining human papillomavirus infection rates (6.6%)21 in India and the fact that human papillomavirus prevalence in our study region was not evaluated before. While more than three-fourths (77.64%) of the participants revealed getting married between the ages of 11 and 20, half the participants reported a parity of more than three. Our observation is akin to studies from Chandigarh and Himachal Pradesh where early marriage and multiparity showed a significant association with cervical cancer.22,23 We also noted high-risk human papillomavirus infection in widows/separated and unmarried yet sexually active women (25.3%) and a significant association between the two variables. Our findings were higher than an Indian study which observed a human papillomavirus prevalence of 12.9% among unmarried yet sexually active tribal girls.24 Hence, educating tribal women about safe sexual practices to curb the growing threat of RTI/STIs is indispensable.
Maximum prevalence of human papillomavirus (42.42%), Candida (60%), Chlamydia trachomatis (80%), and bacterial vaginosis (59.61%) was seen in tribal women between 31 and 40 years (300; 59.88%). Our observation is in line with other studies7,17,18 which reported RTI/STIs prevalence in this age group. More than half of the participants (330; 66%) reported tubal ligation as the preferred contraceptive method; however, maximum RTI/STIs prevalence was seen in participants who underwent tubal ligation. High prevalence of bacterial vaginosis (65.8%), Candida (66.7%), Chlamydia trachomatis (60%), and human papillomavirus (57.5%) was observed in tubal ligation cases. Studies from Mumbai25 and Delhi26 reported similar results where tubal ligation was the preferred contraceptive method (37.9% and 70.3%, respectively) and bacterial vaginosis and Candidiasis as the common RTI/STIs among women opting for tubal ligation. The high reproductive tract/sexually transmitted infection prevalence could be due to terminating the usage of barrier contraceptives like condoms post-tubal ligation by tribal women. However, informing them that tubal ligation is only a contraceptive method without offering any protection to the cervix and lower genital tract against RTI/STIs is essential, and promoting condom usage is recommended.
We observed a low prevalence of Chlamydia trachomatis (1%) and an absence of co-infection and association between human papillomavirus and Chlamydia trachomatis among our participants. Chlamydia was absent in patients diagnosed with atypical squamous cells of undetermined significance, low-grade squamous intraepithelial lesion, high-grade squamous intraepithelial lesion, or other cytological abnormality. This could be due to the syndromic treatment approach employed by healthcare providers in treating RTI/STIs in patients. While few articles report an association between human papillomavirus-induced squamous cell carcinoma and Chlamydia trachomatis,27,28 some report, the absence of association between human papillomavirus and Chlamydia trachomatis3,29; hence, there still exists a gap in understanding the underlying mechanisms of cervical carcinogenesis with Chlamydia trachomatis. A trivial number of participants were diagnosed with Candidiasis (5.98%) in our study. Out of four participants with low-grade squamous intraepithelial lesion and cytological abnormality, two were diagnosed with Candidiasis and two with concurrent Candida and human papillomavirus infection. While our observation is consistent with other Indian studies7,9,19 noting low Candidiasis prevalence rates, we did not observe any association between human papillomavirus and Candida. Although it has been hypothesised that cases of recurrent Vulvovaginal Candidiasis caused by pathogenic Candida spp. strains allow mucosal penetration, induce erythema and cell exfoliation,30 it has been established that there is a lack of association between Candida spp. and high-risk human papillomavirus.31
Bacterial vaginosis was diagnosed in 41.51% participants, while intermediate bacterial vaginosis score was observed in 56.73%. Past studies among Kannadiga tribal women7 and urban women from Mumbai9 and Puducherry19 reported low prevalence rates for bacterial vaginosis as 2.5%, 7.4%, and 26.25%, respectively, while another Mumbai study32 reported a high bacterial vaginosis prevalence of 44.1%. Evaluation of cytological abnormalities by Pap smear revealed bacterial vaginosis in patients with atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion (0.5% each), and co-infection with human papillomavirus in four patients with high-grade squamous intraepithelial lesion and any cytological abnormalities. Although we noted slightly high bacterial vaginosis prevalence rates, we observed a statistically significant correlation between high-risk human papillomavirus infection and clue cells observed while diagnosing bacterial vaginosis (p-value: 0.04). This is supported with Chinese33 and Albanian34 studies and a systematic review35 which observed a significant association between bacterial vaginosis and high-risk human papillomavirus infections. Bacterial vaginosis has been hypothesised in acquiring and transmitting human papillomavirus infection due to altered vaginal flora and associated inflammation. While it is suggested that the entry of human papillomavirus in the actively proliferating basal cells of the cervical epithelium due to inflammation-induced rupturing of the cervical epithelium,32 another study suggests loss of mucous layer protecting the vagina due to lytic enzyme release from the bacteria resulting in micro- abrasions of epithelia, thereby increasing virulence and adhesiveness of human papillomavirus and promoting the integration of viral genome in epithelia of the transformation zone.34 Due to this association in ours and past studies, we suggest treating bacterial vaginosis to reduce the threat of co-infection with human papillomavirus.
Our study is the first to report human papillomavirus and reproductive tract/sexually transmitted infection prevalence among tribal women in Maharashtra. It provides valuable insights for policymakers to address RTI/STIs in this vulnerable group. Our findings can help in formulating health education strategies, like health talks in local dialect and tailored information, education, communication (IEC), materials, to improve awareness and practices around reproductive tract/sexually transmitted infections, screening, prevention, and hygiene.
Limitations
Reproductive tract/sexually transmitted infection evaluation among tribal men was not done and only a subset of tribal women could be screened due to sample size constraints, so the actual prevalence may be higher. We did not screen for other sexually transmitted pathogens or characterise bacterial vaginosis and Candida species. Additionally, recruiting women from healthcare centres rather than using random sampling may affect infection rate estimates. Finally, since sexual behaviours and gynaecological morbidities differ from region to region, our findings will be different from tribal women belonging to other regions.
Conclusion
To conclude, we noted contrasting infection rates of human papillomavirus, bacterial vaginosis, Candida, and Chlamydia trachomatis among tribal women. However, a significant association between bacterial vaginosis and human papillomavirus was observed, suggesting that bacterial vaginosis might play a role as a co-factor in human papillomavirus-mediated cervical carcinogenesis. This highlights the importance of screening women for the simultaneous presence of different co-infections with human papillomavirus. Since routine human papillomavirus and cervico-vaginal infection testing is not a standard practice in such resource-poor regions, our findings contribute to the limited body of knowledge concerning these pathogens among tribal populations in the form of epidemiological data which may play a role in formulating testing and screening guidelines.
Acknowledgement
We acknowledge Dr. Geetanjali Sachdeva, Dr. Smita Mahale, Dr. Ragini Kulkarni, Dr. Dayanand Suryavanshi, and Dr. Bontha V. Babu for their guidance and support. We thank all the clinical trial co-ordinators and laboratory staff at the collaborating institute for their assistance. We also thank the Accredited Social Health Activists Mrs. Roshni Gothankar and Mrs. Roshni Kadu for their help while recruiting the participants. Finally, we thank all the study participants for their participation.
Ethical approval
The research/study was approved by the Institutional Review Board at ICMR NIRRCH ethics committee for Human studies, number (D/ICEC/Sci-150/159/2019), dated 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Indian Council of Medical Research, Grant (RFC No. (P-31) SBHSR/Ad-hoc/28/2019-20).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- International Agency for Research on Cancer. Globocan 2020 India Factsheet. https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf. last accessed 21 March 2023.
- Cancer cervix: Epidemiology and disease burden. Cytojournal. 2022;19:21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of Chlamydia trachomatis infection with human papillomavirus (HPV) & cervical intraepithelial neoplasia - A pilot study. Indian J Med Res. 2013;137:533-9.
- [PubMed] [PubMed Central] [Google Scholar]
- Potential opportunities to reduce cervical cancer by addressing risk factors other than HPV. J Gynecol Oncol. 2013;24:295-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Burden and associated genotype patterns of high-risk human papilloma virus infection and cervical cytology abnormalities among women in central India. Infect Dis Obstet Gynecol. 2022;2022:3932110.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mechanisms of disease: Inflammation and the origins of cancer. Nat Clin Pract Oncol. 2005;2:90-7; quiz 1 p following 113.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical cytology and associated factors among tribal women of Karnataka, India. PLoS One. 2021;16:e0248963.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of human papillomavirus and co-existent sexually transmitted infections among female sex workers, men having sex with men and injectable drug abusers from eastern India. Asian Pac J Cancer Prev. 2012;13:799-802.
- [CrossRef] [PubMed] [Google Scholar]
- Genital discharge, human papillomavirus screening and contraceptive use in a tertiary care hospital in Mumbai, India. Indian J Dermatol Venereol Leprol. 2020;86:583-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tribal research and training institute, government of Maharashtra. division wise total & tribal population. https://trti.maharashtra.gov.in/index.php/en/divisionwise-total-tribal-population. last accessed 30 March 2023.
- Enablers & challenges of tribal women & health system for implementation of screening of non-communicable diseases & common cancers: A mixed-methods study in Palghar district of Maharashtra, India. Indian J Med Res. 2022;156:319-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Reproductive health care status of the displaced tribal women in India: An analysis using Nussbaum Central human capabilities. Health Care Women Int. 2021;42:390-419.
- [CrossRef] [PubMed] [Google Scholar]
- Changing perspectives of tribal health in the context of increasing lifestyle diseases in India. J Environ Soc Sci. 2014;1:101.
- [Google Scholar]
- Sexual risk behaviour among migrant tribals living in urban slums of an eastern Indian city: Implications on the spread of HIV. Coll Antropol. 2008;32:1-4.
- [PubMed] [Google Scholar]
- Current Chlamydia trachomatis Infection: A major cause of infertility. J Reprod Infertil. 2012;13:204-10.
- [PubMed] [PubMed Central] [Google Scholar]
- Sequence analysis of the major outer membrane protein gene from Chlamydia trachomatis serovar L2. J Bacteriol. 1986;168:1277-82.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of sexually transmitted disease syndromes in tribal population of central India. J Epidemiol Community Health. 2009;63:805-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of sexually transmitted infections: A profile from a rural- and tribal-based sexually transmitted infections clinic of a tertiary care hospital of Eastern India. J Family Med Prim Care. 2018;7:1042-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Spectrum of vaginal discharge in a tertiary care setting. Trop Parasitol. 2013;3:135-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Human papilloma and other DNA virus infections of the cervix: A population based comparative study among tribal and general population in India. PLoS One. 2019;14:e0219173.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HPV vaccination of girl child in India: Intervention for primary prevention of cervical cancer. Asian Pac J Cancer Prev. 2018;19:2357-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors of cervical cancer: A case-control study. Asia Pac J Oncol Nurs. 2019;6:308-14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors for cancer cervix among rural women of a hilly state: A case-control study. Indian J Public Health. 2015;59:45-8.
- [CrossRef] [PubMed] [Google Scholar]
- Higher prevalence of human papillomavirus infection in adolescent and young adult girls belonging to different Indian tribes with varied socio-sexual lifestyle. PLoS One. 2015;10:e0125693.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Reproductive tract infections, gynaecological morbidity and HIV seroprevalence among women in Mumbai, India. Bull World Health Organ. 1998;76:277-87.
- [PubMed] [PubMed Central] [Google Scholar]
- Aetiology & risk factors of recurrent vaginitis & its association with various contraceptive methods. Indian J Med Res. 2010;131:83-7.
- [PubMed] [Google Scholar]
- Co-expression of HSV2 and Chlamydia trachomatis in HPV-positive cervical cancer and cervical intraepithelial neoplasia lesions is associated with aberrations in key intracellular pathways. Intervirology. 2008;51:230-4.
- [CrossRef] [PubMed] [Google Scholar]
- Human Papillomaviruses and genital co-infections in gynaecological outpatients. BMC Infect Dis. 2009;9:16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Molecular detection of Chlamydia trachomatis and HPV infections in cervical samples with normal and abnormal cytopathological findings. Diagn Cytopathol. 2007;35:198-202.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of association between vaginal infections and high-risk human papillomavirus types in female sex workers in Spain. ISRN Obstet Gynecol. 2012;2012:240190.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Candida and squamous (pre)neoplasia of immigrants and Dutch women as established in population-based cervical screening. Int J Gynecol Cancer. 2006;16:1596-600.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of conventional papanicolaou smear in diagnosing bacterial vaginosis among women with clinical genital infection. South Asian J Cancer. 2020;9:13-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The prevalence of human papillomavirus and bacterial vaginosis among young women in China: A cross-sectional study. BMC Womens Health. 2021;21:409.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vaginal infections of Albanian women infected with HPV and their impact in intraepithelial cervical lesions evidenced by Pap test. J Cytol. 2017;34:16-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bacterial vaginosis is associated with uterine cervical human papillomavirus infection: A meta-analysis. BMC Infect Dis. 2011;11:10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






