Translate this page into:
Association of type 2 lepra reaction with filariasis and malaria
2 Department of Microbiology, Institute of Medical Sciences, Banaras Hindu University, Uttar Pradesh, India
3 Department of Community Medicine, Institute of Medical Sciences, Banaras Hindu University, Uttar Pradesh, India
4 Department of General Medicine, Kashi Medicare Centre, Varanasi, Uttar Pradesh, India
Correspondence Address:
Taniya Sharma
Department of Dermatology and Venereology, Institute of Medical Sciences, Banaras Hindu University, Varanasi - 221 005, Uttar Pradesh
India
| How to cite this article: Singh SK, Sharma T, Nath G, Singh TB, Shrivastava MK. Association of type 2 lepra reaction with filariasis and malaria. Indian J Dermatol Venereol Leprol 2015;81:224 |
Sir,
Type 2 lepra reaction (T2R) is a Gell and Coomb′s type 3 hypersensitivity reaction characterized by high grade fever, erythema nodosum leprosum, arthralgia, myalgia, uveitis, orchitis, neuritis and various other complications due to deposition of immune complexes in blood vessels all over the body. [1] It has been postulated that type 2 lepra reactions can be precipitated by various physical and mental stressors, infections, pregnancy, lactation, vaccination, drugs, etc., Even though mentioned by most text books, there are very few studies showing an association between infections and type 2 lepra reaction. The various infections probably precipitating this reaction reported till date are filariasis, [2] human immunodeficiency virus infections [3] and chromoblastomycosis. [4] Our area is endemic for leprosy, malaria as well as filariasis and all the three infections can present with high grade fever during their course. So we undertook a study to evaluate the presence of filarial and malarial infections in patients of leprosy with type 2 lepra reactions and assessed whether a significant association occurs between these infections.
Our study was a cross-sectional study that included patients of leprosy presenting with type 2 lepra reactions while controls were cases of leprosy without reaction. Type 2 lepra reaction was diagnosed in cases of leprosy presenting with high grade fever and lesions of erythema nodosum leprosum with/without arthralgia, myalgia, neuritis, orchitis, iridocyclitis, periostitis and neutrophilia. Filariasis was diagnosed using filarial dipstick enzyme-linked immunosorbent assay (ELISA) for WBSX1 antigen. This test has a sensitivity of 99-100% and specificity of 95%. [5] Malaria was diagnosed by means of microscopic examination for the malaria parasite using both thick and thin smears of peripheral blood.
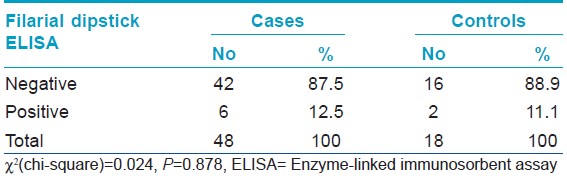
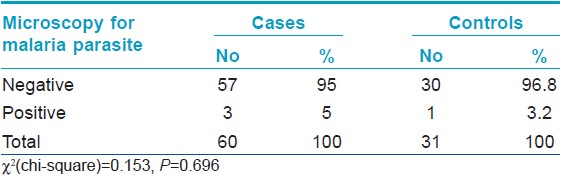
Out of 48 cases investigated for filaria using filarial dipstick ELISA, 6 (12.5%) patients tested positive. Among the 18 patients in the control group, the test was positive in 2 (11.1%) cases. The difference was not statistically significant (P = 0.878) [Table - 1]. Sixty cases were examined for malaria parasite and 3 (5%) were found to be positive while 1 (3.2%) out of 31 patients in the control group was positive. This difference was again statistically non-significant (P = 0.696) [Table - 2]. The filarial dipstick ELISA was not done on all the patients because not all of them could afford it.
Malaria and filariasis are frequently found in our region. Although leprosy has been eliminated in most states of India, there are still many endemic districts where prevalence is >1/10000 population and Varanasi is one of the districts endemic for leprosy.
We were unable to find any previous study regarding an association of filariasis and malaria with type 2 lepra reactions. The earliest description of an infection precipitating type 2 lepra reaction was a case series by Nigam et al. of five patients in whom filarial infection precipitated the reaction. [2] However, we found no statistically significant association between type 2 lepra reaction and filariasis and malaria.
| 1. |
Jopling WH, McDougall AC. The Disease. Handbook of Leprosy. 5 th ed. Vol. 2. New Delhi: CBS; 1996. p. 10-53.
[Google Scholar]
|
| 2. |
Nigam P, Goyal BM, Mishra DN, Samuel KC. Reaction in leprosy complicated by filariasis. Lepr India1977:49:344-8.
[Google Scholar]
|
| 3. |
Sharma NL, Mahajan VK, Sharma VC, Sarin S, Sharma RC. Erythema nodosumleprosum and HIV infection: A therapeutic experience. Int J Lepr Other Mycobact Dis 2005;73:189-93.
[Google Scholar]
|
| 4. |
Apte G, Gedam JR, Poojary S, Nagpur NG, Pai VV, Ganapathi R. Chromoblastomycosis in a case of borderline lepromatous leprosy with recurrent type II lepra reaction. Lepr Rev 2011;82:310-5.
[Google Scholar]
|
| 5. |
Abdul Rahman R, Hwen-Yee C, Noordin R. Pan LF-ELISA using BmR1 and BmSXPrecombinant antigens for detection of lymphatic filariasis. Filaria J 2007;6:10.
[Google Scholar]
|
Fulltext Views
2,370
PDF downloads
2,749





