Translate this page into:
Association of various risk factors with childhood herpes zoster: A case–control study in Indian patients
Corresponding author: Dr. Priyadarshini Sahu, Department of Dermatology, Venereology and Leprology, Pandit Bhagwat Dayal Sharma University of Health Sciences, Rohtak, Haryana, India. priyadarshini.sahu.9@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahu P, Dayal S. Association of various risk factors with childhood herpes zoster: A case–control study in Indian patients. Indian J Dermatol Venereol Leprol 2021;87:725-8.
Sir,
Recent studies from Indian set up are showing a conspicuous rise in cases of childhood herpes zoster in immunocompetent children.1 The aim was to study the clinical presentation, complications and the association of various risk factors with childhood zoster by conducting age- and sex-matched case– control study in Indian patients.
The study was ethically approved by Institutional Ethics Committee and patients were recruited from the Department of Dermatology, Pandit B. D. Sharma, PGIMS, Rohtak, Haryana. Guardians of patients and controls gave their voluntary informed consent. Convenience sample size was selected which included 30 patients of age ≤14 years, who were clinically diagnosed as a case of herpes zoster and had multinucleated giant cells on Tzanck smear. Equal number of age- and sex-matched controls were selected from the healthy children who did not have a history of having the disease. The children in the control group were those who were coming along with other patients to our outpatients' department and were healthy.
Detailed history and clinical examination was done in all the patients. Patient’s sera were tested for antibody to HIV which was confirmed by Western blot assay. Complete blood count, chest X-ray and ultrasonography of abdomen were done to rule out any underlying malignancy. Anemia was diagnosed on the basis of both peripheral blood smear and mean corpuscular volume.
Anemia was defined as hemoglobin concentration <11 g/ dL for children between 6 and 59 months; <11.5 g/dL for children between 5 and 11 years and <12 g/dL for children aged 12 years according to the WHO.2 MCV >100 fL was considered as megaloblastic anemia. Statistical Package for the Social Sciences for Windows version 22.0 was used for statistical analysis. Comparisons among groups were performed using the χ2 test. Crude odds ratio was calculated.
Thirty patients of childhood herpes zoster were included in the study [Figure 1]. The demographic and clinical data are tabulated in Table 1 [Figures 2 and 3]. None of our patients developed complications except scarring at the site of the lesions in two patients. All patients were treated with oral acyclovir and symptomatic treatment.
Comparison of various risk factors within the study and control groups is given in Table 1. On evaluating patients’ complete blood count, it was found that 21 out of 30 patients had megaloblastic anemia which was significantly associated with occurrence of childhood herpes zoster [Table 2]. Thus, megaloblastic anemia had significantly increased odds for occurrence of the condition in childhood (odds ratio: 21; 95% confidence interval: 3.9–112.7).
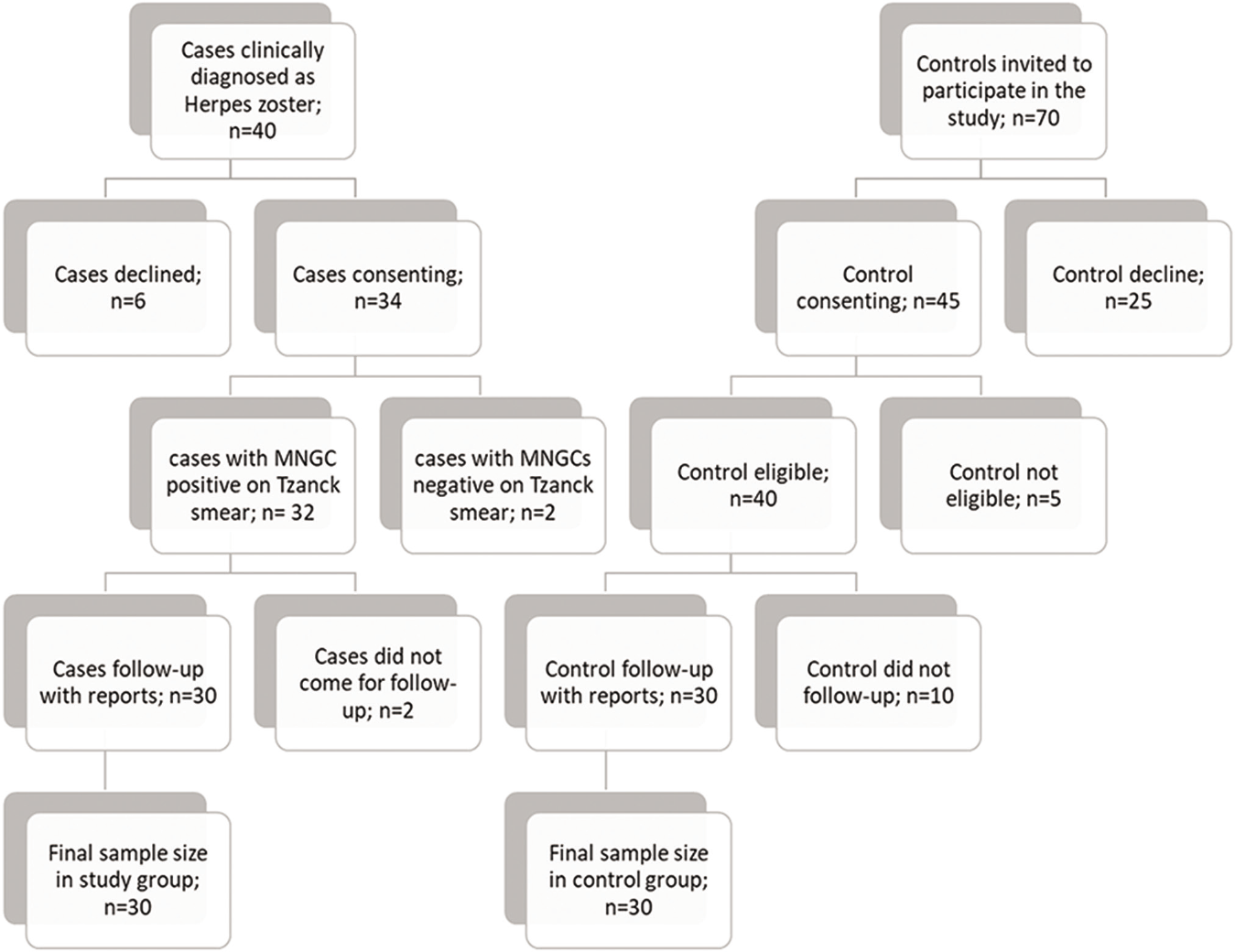
- Flowchart of patient recruitment in the study and control groups

- A 12-year-old girl presented with scarring following herpes zoster along T1-T2 dermatome on the right side arm and back

- A 12-year-old girl presented with scarring following herpes zoster along T1-T2 dermatome on the right side arm and back

- A 1-year-old child presented with herpes zoster of the right T1 dermatome
| Characteristics | Study patients (n=30) | Control (n=30) | P-value | Odds ratio with confidence interval |
|---|---|---|---|---|
| Age (mean±SD) | 8.70±4.2 years | 8.90±3.7 years | 0.9 (insignificant) | - |
| Sex (M: F) | M=19, F=11 | M=18, F=12 | - | - |
| Duration of disease (days) | 2.5±0.9 | - | - | - |
| Prodromal symptoms | - | - | - | |
| Mild burning sensation | 3 | |||
| Itching | 5 | |||
| Pain | 17 | |||
| Itching and pain | 2 | |||
| Nil | 3 | |||
| Dermatome involved: | - | - | - | |
| Thoracic | 19 | |||
| Lumbar | 6 | |||
| Head and neck | 5 | |||
| Contact of chickenpox | Present in six patients | Present in four patients | 0.7 (insignificant) | 1.6 (0.4–6.5) |
| History of chickenpox | Present in eight patients | Present in seven patients | 0.766 (insignificant) | 1.2 (0.4–3.9) |
| Vaccination history | Present in two patients | Present in two patients | 1.00 (insignificant) | 1 (0.1–7.6) |
| History of maternal varicella | Present in two patients (1st patient at the age of 6 years and 2nd patient at the age of 5 years) | Present in one patient | 1.00 (insignificant) | 2.1 (0.18–24.1) |
| Evidence of immunosuppression | Present in two patients | Present in none of the patients | 0.4 (insignificant) | 2.1 (1.6–2.7) |
| Presence of megaloblastic anemia | Present in 21patients | Present in two patients | <0.001 (significant) | 21 (3.9–112.7) |
| Groups | Megaloblastic anemia present | Megaloblastic anemia absent |
|---|---|---|
| Study group | 21 Case 1: Hb–9 g/dl; MCV–103 fL Case 2: Hb–9.5 g/dl; MCV–102 fL Case 3: Hb: 10 g/dl; MCV–101 fL Case 4: Hb: 8.8 g/dl; MCV–101 fL Case 5: Hb: 9.8 g/dl; MCV–102 fL Case 6: Hb: 9.5 g/dl; MCV–100 fL Case 7: Hb: 8.7 g/dl; MCV–103 fL Case 8: Hb: 9.4 g/dl; MCV–102 fL Case 9: Hb: 9.8 g/dl; MCV–102 fL Case 10: Hb: 8.8 g/dl; MCV–103 fL Case 11: Hb: 8.5 g/dl; MCV–103 fL Case 12: Hb: 8.2 g/dl; MCV–104 fL Case 13: Hb: 8.6 g/dl; MCV–103 fL Case 14: Hb: 9.2 g/dl; MCV–102 fL Case 15: Hb: 10 g/dl; MCV–101 fL Case 16: Hb: 9.6 g/dl; MCV–102 fL Case 17: Hb: 8.9 g/dl; MCV–102 fL Case 18: Hb: 9 g/dl; MCV–102 fL Case 19: Hb: 8.5 g/dl; MCV–104 fL Case 20: Hb: 9 g/dl; MCV–102 fL Case 21: Hb: 10 g/dl; MCV–101 fL |
9 |
| Control group | 2 | 28 |
Vaccination with live-attenuated virus could be one of the reasons for recent rise in childhood herpes zoster according to a few reports.3 However, our study is in concordance, with those studies which have revealed that varicella vaccination does not increase the incidence of zoster.4 It is proposed that vaccine strain is attenuated and has less chance of reactivation as compared to wild-type virus. However, the effect of vaccination on occurrence of the disease in childhood cannot be commented on as the trend of vaccination against varicella is not so much prevalent in our country. The previous studies have also shown varicella during early life as an important risk factor.5 In our study, the difference was statistically insignificant, but a history of chickenpox may be a risk factor as the episode of chickenpox is mild in immunocompetent children and may go unnoticed. History of maternal varicella during pregnancy or history of contact with chickenpox patients may also be risk factors.1 However, in our study, these factors were not significantly associated with the study group when compared with the control group. It may be due to unreliable history given by the patients.
Recently, studies have shown that there is no increase in the incidence of malignancy in childhood herpes zoster.1 A greater number of patients in the study group had immunosuppression with respect to the control group but the difference was statistically insignificant. Therefore, our study is in concordance with the findings of recent studies. However, our study had a very small sample size to conclude these facts.
In our study, we found a strong significant association between megaloblastic anemia and pediatric herpes zoster. The most common cause of megaloblastic anemia is deficiency of vitamin B12 or folic acid. This may be cause of immature immune response leading to low levels of natural killer cells, lymphocytes and cytokines along with virus-specific immunoglobulins which may be the cause of inability to maintain varicella zoster virus latency, leading to appearance of herpes zoster at an early age.1 However, as our sample size was small, this association cannot be affirmed.
Serology could not be done for detecting antibodies. There may be a possibility of recall and confounding bias. Confounding bias, such as nutritional status of the patients, could have been present. We could not find the underlying cause of megaloblastic anemia.
Despite elaborate literature search, we are unable to find any such study to report the possibility of association of anemia with pediatric herpes zoster. Further prospective population-based studies with better investigation profile and evaluation of nutritional status of these children are required to confirm our observation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A clinicoepidemiological study of childhood herpes zoster. Indian Dermatol Online J. 2018;9:383-8.
- [Google Scholar]
- Iron Deficiency Anaemia: Assessment. 2001. Prevention and Control, a Guide for Programme Managers. Geneva, Switzerland: World Health Organization; Available from: https://www.who.india_assessment_prevention_control [Last accessed on 2020 Apr 01]
- [Google Scholar]
- Pediatric vaccine-strain herpes zoster: A case series. Pediatr Dermatol. 2017;34:665-7.
- [CrossRef] [Google Scholar]
- Incidence and clinical characteristics of herpes zoster among children in the varicella vaccine era, 2005-2009. J Infect Dis. 2013;208:1859-68.
- [CrossRef] [Google Scholar]
- The incidence and clinical characteristics of herpes zoster among children and adolescents after implementation of varicella vaccination. Pediatr Infect Dis J. 2009;28:954-9.
- [CrossRef] [Google Scholar]





