Translate this page into:
Asteatotic eczema following paclitaxel and carboplatin chemotherapy for lung carcinoma
Corresponding author: Dr. Prachi Vinayak Gole, Department of Dermatology, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India. prachigole2@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vishwanath T, Mahajan SA, Gole PV, Kulkarni M. Asteatotic eczema following paclitaxel and carboplatin chemotherapy for lung carcinoma. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_569_2024
Dear Editor,
A variety of eczematous adverse drug reactions are reported due to cancer chemotherapeutic agents.1 These are especially pronounced with epidermal growth factor receptor (EGFR) inhibitors due to cutaneous dysmaturation. Other mechanisms include altered cutaneous immunologic profile and skin-directed cell-mediated immunity.1 Older chemotherapeutic agents rarely cause such changes. We describe a case of eczema craquele following paclitaxel and carboplatin chemotherapy with clinico-dermoscopic and histopathologic features.
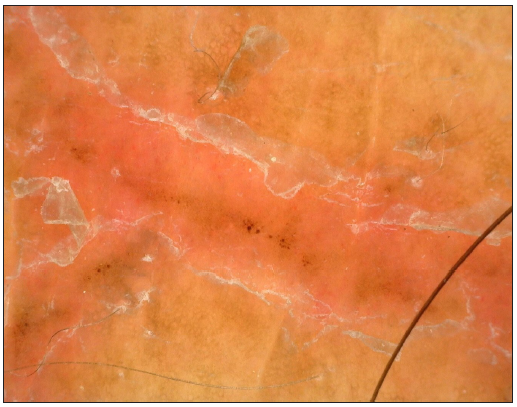
A 68-year-old male diagnosed with non-small cell carcinoma of the lung presented with sudden onset generalised severe itching and dryness of the skin along with non-tender fissures on the flanks, thighs and legs [Figure 1a and 1b]. This began 2–3 days after administration of paclitaxel and carboplatin 3 months after diagnosis. There was no history suggestive of atopic diathesis, other concomitant medications, comorbidities, or similar complaints in the past. On examination, the patient was averagely built and nourished. There was generalised xerosis along with linear dull erythematous non-tender wavy fissures on the waist and lower limbs. Polarised dermoscopy (Dinolite videodermoscope, polarised mode, 50x) revealed fissures with scales having double free edges, scattered red dots and linearly arranged brown dots and clods [Figure 2]. Biopsy (after informed consent) revealed focal parakeratosis with orthokeratosis, scattered necrosis, and dysmaturation of keratinocytes scattered throughout the epidermis, superficial perivascular and interstitial lymphocytes, and erythrocyte extravasation [Figure 3a and 3b]. A diagnosis of eczema craquele (asteatotic eczema) probably due to paclitaxel and carboplatin was made (Naranjo score=6; previous conclusive reports (+1), appearance after drug administration (+2), improvement after discontinuation and specific therapy (+1), adverse reaction reappearing after drug administration (+2), objective evidence (+1, cutaneous dysmaturation noted on histopathology), alternative causes (−1, in this case, the malignancy). After a 2-week course of tablet levocetirizine 5 mg at night and emollients, the lesions resolved completely. He continued to have similar episodes with similar intensity after each chemotherapy cycle which would resolve with the same treatment.

- Eczema craquele presenting with wavy linear erythematous fissures on the flanks.

- Eczema craquele presenting with wavy linear erythematous fissures on the lower limbs.
- Polarised dermoscopic image depicting double-edged white scales, irregularly distributed red dots and linear brown dots and clods with a red background in the fissures.
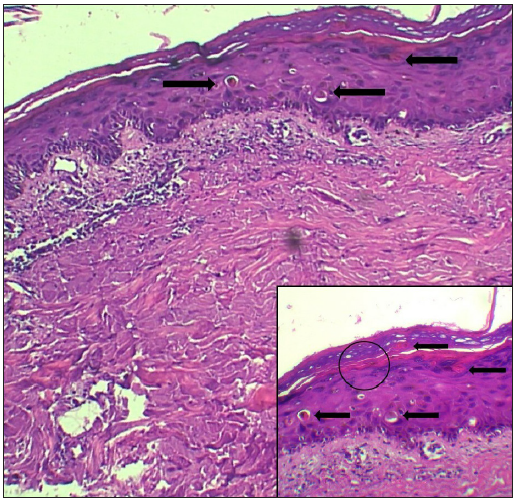
- Focal parakeratosis and focal scattered keratinocyte dyskeratosis at multiple epidermal levels (black arrows) and superficial perivascular and interstitial mononuclear infiltrate. (Haematoxylin and eosin; 100x). Inset (200x) shows dyskeratosis (black arrows), focal parakeratosis overlying a focally attenuated granular layer (black circle).
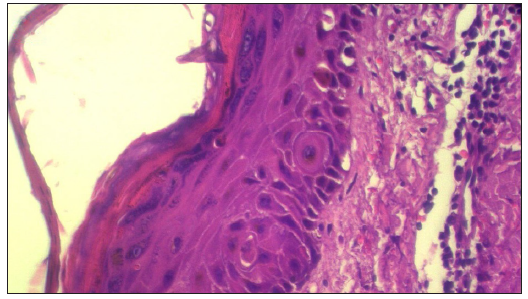
- Keratinocyte dysmaturation with parakeratosis with superficial lymphocytic infiltrate (Haematoxylin and eosin, 400x).
Eczema craquele is a peculiar form of dermatitis usually seen in the elderly, caused due to loss of cutaneous lipids which normally constitute a formidable barrier to transepidermal elimination of water. Clinical manifestations are characteristic and comprise of pruritic, erythematous, linear, and wavy fissures in various configurations on a background of xerotic skin predominantly on the trunk and lower extremities. A variety of underlying causes exist such as altered weather conditions (cold, dry weather in particular), malnutrition, hypothyroidism and malignancies (especially lymphomas).2 Drugs constitute an important, treatable cause of eczema craquele and cutaneous xerosis.2 Thiazide diuretics, statins and retinoids are common causes. Among anti-neoplastic drugs, EGFR and multikinase inhibitors such as erlotinib are among the commonest class of drugs. Very few reports of traditional chemotherapeutic drugs causing this adverse event exist. Drugs implicated include paclitaxel, carboplatin and pemetrexed.3-5 The short duration between chemotherapy administration and the onset of symptoms is striking and has also been reported previously.4 The likely pathogenic mechanism is epidermal dysmaturation causing impaired cutaneous barrier which increases transepidermal water loss. Carboplatin andpaclitaxel are highly lipid soluble and are synergistically cytotoxic.6,7 Their combined high-dose administration and consequent diffusion into the lipid-rich epidermis in the patient who was already at risk for eczema craquele owing to his age and malignancy could account for the acute onset of symptoms. This was corroborated on histopathology in the present case. Dermoscopic features of scales with double free edges and irregularly distributed dotted vessels in the superficial fissure also suggest the diagnosis.
Although distressing for the patient, simple measures such as administration of antihistaminics and emollients, commencing several days before and extending several days after chemotherapy beside avoidance of harsh soaps and scratching are usually sufficient.1 Dermoscopy may also be a valuable non-invasive adjunct to diagnosis with less than five cases described previously. Future research may also elucidate histopathologic differences between various forms of eczematous drug eruptions besides uncovering newer mechanisms. This may help in developing newer drugs with less adverse event profile.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Eczematous drug eruptions. Am J Clin Dermatol. 2021;22:349-66.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Asteatotic eczema. In: Stat pearls. Treasure Island (FL): Stat Pearls Publishing; 2023.
- [Google Scholar]
- The first case of drug-induced pseudoscleroderma and eczema craquelé related to nab-paclitaxel pancreatic adenocarcinoma treatment. Postepy Dermatol Alergol. 2018;35:106-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diffuse rash after the administration of carboplatin and paclitaxel. Am J Dermatopathol. 2016;38:365.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized eczema craquelé (asteatotic dermatitis) associated with pemetrexed treatment. J Eur Acad Dermatol Venereol. 2016;30:e81-3.
- [CrossRef] [PubMed] [Google Scholar]
- A simple passive equilibration method for loading carboplatin into pre-formed liposomes incubated with ethanol as a temperature dependent permeability enhancer. J Control Release. 2017;252:50-61.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular drug delivery. Life (Basel). 2024;14:451.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





