Translate this page into:
Asymptomatic, extensive brownish macules and patches on the lower abdomen and legs
Corresponding author: Dr. Yoon-Seob Kim, Department of Dermatology, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Wonmi-gu, Bucheon, Korea. kysbbubbu@catholic.ac.kr
-
Received: ,
Accepted: ,
How to cite this article: Lee KH, Jeong JH, Kim Y-S. Asymptomatic, extensive brownish macules and patches on the lower abdomen and legs. Indian J Dermatol Venereol Leprol. 2025;91:261-3. doi: 10.25259/IJDVL_396_2024
A 72-year-old man presented with asymptomatic, extensive brownish macules and patches on the lower abdomen and legs for 1 week [Figure 1]. He had a medical history of asthma. Histopathological examination revealed diffuse perivascular and interstitial eosinophil infiltration, extravasation of red blood cells, and nuclear debris throughout the dermis [Figures 2a and 2b]. Laboratory findings revealed eosinophilia (2740 eosinophils/uL) and a high level of C-reactive protein (22.08 mg/L; normal range 0–5 mg/L), high levels of immunoglobulin E (7293 IU/mL; normal range 0–100 IU/mL) and immunoglobulin G4 (>352 mg/dL; normal range 3.9–86.4 mg/dL), negativity for p-anti-neutrophil cytoplasmic antibody (ANCA), c-ANCA, antinuclear antibodies, rheumatoid factor, cryoglobulins and anti-cyclic citrullinated peptide. There were no abnormal findings in complement levels (C3, C4) or routine urine analysis. A computed tomographic scan of the whole body showed a retention polyp in the right maxillary sinus [Figure 3a] and coarse ground-glass opacity in the lungs accompanied by bilateral pleural effusions [Figure 3b].
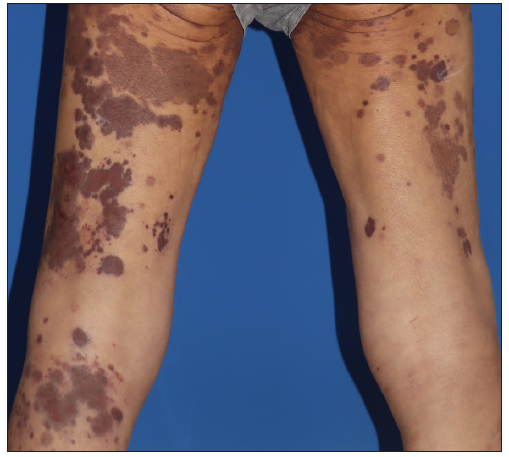
- Asymptomatic, extensive brownish macules and patches on the lower limbs.
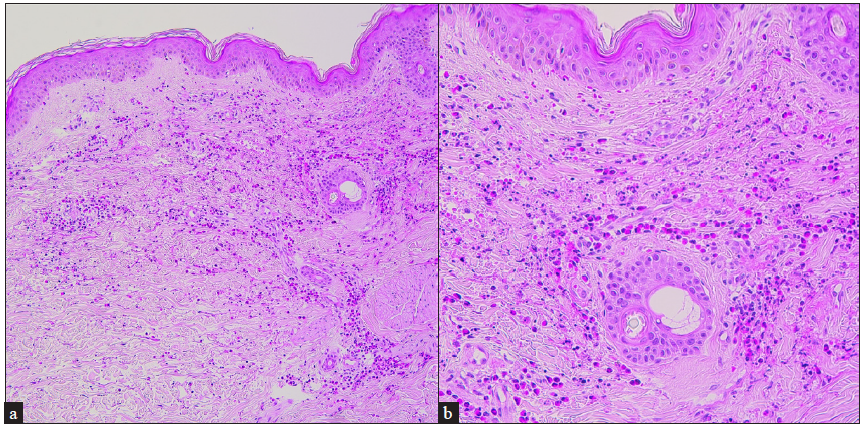
- Diffuse perivascular and interstitial eosinophil infiltrations extravasation of red blood cells, and nuclear debris throughout the dermis on Haematoxylin and eosin stained skin biopsy; (a) 100x and (b) 200x.

- Retention polyp on right maxillary sinus (indicated by white arrow) was found by computed tomographic scan on the neck.
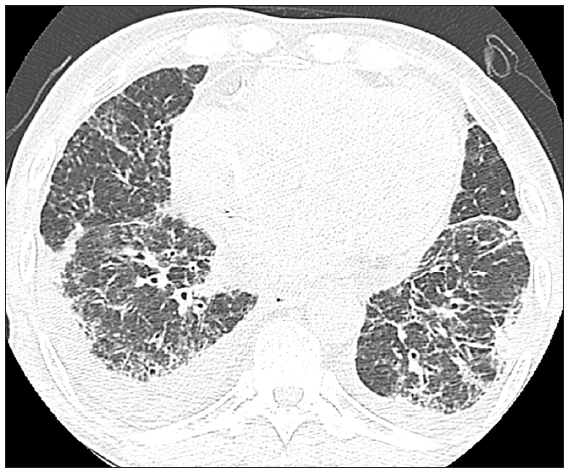
- Coarse ground glass opacity in the entire lung accompanied with bilateral pleural effusion was found by computed tomographic scan on the chest.
Question
What is your diagnosis?
Answer
Eosinophilic granulomatosis with polyangiitis.
Discussion
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as Churg–Strauss syndrome, is a rare but severe systemic vasculitis associated with asthma and eosinophilia.1 EGPA is categorised as a small vessel, ANCA-associated, eosinophil-rich vasculitis, characterised by necrotising granulomatous inflammation often involving the lungs and necrotising vasculitis of small to medium-sized vessels.2 The phenotype of EGPA is quite heterogeneous with varying proportions of clinical findings: positivity for p-ANCA in ∼40%, and asthma in >90%, ear-nose-throat disease in 60%–80% of the cases.3 Other common clinical findings include peripheral neuropathy and various visceral organ involvement such as pulmonary, renal, cardiac, gastrointestinal, and central nervous system.2 The clinical course of EGPA is characterised by three sequential phases: (1) prodromic or allergic phase (asthma, allergic rhinitis, and sinusitis), (2) eosinophilic phase (eosinophilia and eosinophilic organ infiltration predominantly affecting the lungs), (3) vasculitic phase (purpura, peripheral neuropathy, fever, and malaise).2 Cutaneous lesions include lesions ranging from palpable purpura by the vasculitis of small-sized vessels to subcutaneous nodules by the vasculitis of deeper, medium-sized vessels.4 Mainly glucocorticoids and other immunosuppressive agents such as cyclophosphamide, azathioprine, and methotrexate are recommended for remission induction and maintenance of EGPA.2,3 Skin biopsy extending to the level of the subcutis taken from the most recently-developed, non-ulcerated purpuric, or erythematous lesion is crucial for the diagnosis of EGPA.4 The diagnosis of systemic vasculitis is suspected by the presence of vasculitis in deep dermal vessels, and adjunct testing is needed for cases with a possible diagnosis of EGPA, including direct immunofluorescence and laboratory studies (IgG4, IgE, ANCA, eosinophil count, cytological, or radiological studies).4
Because our patient fulfilled the 2022 American College of Rheumatology criteria for the diagnosis of EGPA (nasal polyps, obstructive airway disease, eosinophilia, and extravascular eosinophilic-predominant inflammation on biopsy), we diagnosed the patient as EGPA. High IgE/IgG4 levels and negative findings of autoantibodies and complements also support the diagnosis of EGPA. Based on the clinicopathological and laboratory findings, possible differential diagnoses of IgA-associated vasculitis, microscopic polyangiitis, polyarteritis nodosa, and cryoglobulinemic vasculitis can be excluded. The possibility of other major organ involvement of EGPA was excluded by interdisciplinary study of physical examination, laboratory tests, echocardiogram, electromyography, and computed tomographic scan for the whole body. Intravenous methylprednisolone was administered at 10 mg/kg for 3 days with gradual tapering. After 1 week of treatment, the eosinophilia and the skin lesions resolved. Our case highlights the rare, but typical manifestations of EGPA. Our case represents a rare diagnosis of EGPA in an elderly patient with severe pulmonary involvement, and the delayed diagnosis which was made in the vasculitic phase of EGPA in spite of prodromic symptoms. The patient was much older than the mean age (50-year-old) of diagnosis for EGPA.3 Dermatologists should be aware of the diagnosis of EGPA in patients with clinical findings of obstructive airway disease, nasal polyps, eosinophilia and histopathological findings of extravascular eosinophilic-predominant inflammation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Reference
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): State of the art. Allergy. 2013;68:261-73.
- [CrossRef] [PubMed] [Google Scholar]
- Eosinophilic granulomatosis with polyangiitis: An overview. Front Immunol. 2014;5:549.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evidence-based guideline for the diagnosis and management of eosinophilic granulomatosis with polyangiitis. Nat Rev Rheumatol. 2023;19:378-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Eosinophilic granulomatosis with polyangiitis: Cutaneous clinical and histopathologic differential diagnosis. J Cutan Pathol. 2021;48:1379-86.
- [CrossRef] [PubMed] [Google Scholar]





