Translate this page into:
Asymptomatic papules and nodules of the vulva
Corresponding author: Dr. Emilio De Dios Berna-Rico, Department of Dermatology, Hospital Universitario Ramon y Cajal, IRYCIS, Madrid, Spain. emilioberna2a@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Berna-Rico EDD, Jimenez-Cauhe J, Guevara-Barona KE, Gonzalez-Cantero A, del Real CMG. Asymptomatic papules and nodules of the vulva. Indian J Dermatol Venereol Leprol 2023;89:469-71.
An otherwise healthy 74-year-old woman presented with a 2-year history of asymptomatic lesions that appeared gradually on her vulva. Clinical examination revealed multiple yellowish and blue-grey papules and nodules located on both labia majora, some with an open-comedo-like appearance [Figure 1a]. Dermoscopy confirmed these findings, also showing an erythematous background and few radiating capillaries at the periphery of some papules [Figure 1b]. There was neither a history of trauma nor inflammation in the vulvar skin prior to the development of lesions. She denied any family history of cutaneous disorders. A punch biopsy from a yellowish papule with a peripheral pore was obtained.
Histological examination revealed a mid-dermal cyst [Figure 2a] lined by stratified squamous epithelium with a granular layer [Figure 2b]. The lumen of the cyst was occupied by orthokeratin with a laminated appearance, admixed with various calibre vellus hair shafts and keratin debris [Figure 2c].
What is your diagnosis?

- Papules and nodules on both labia majora, some of them resembling open comedones
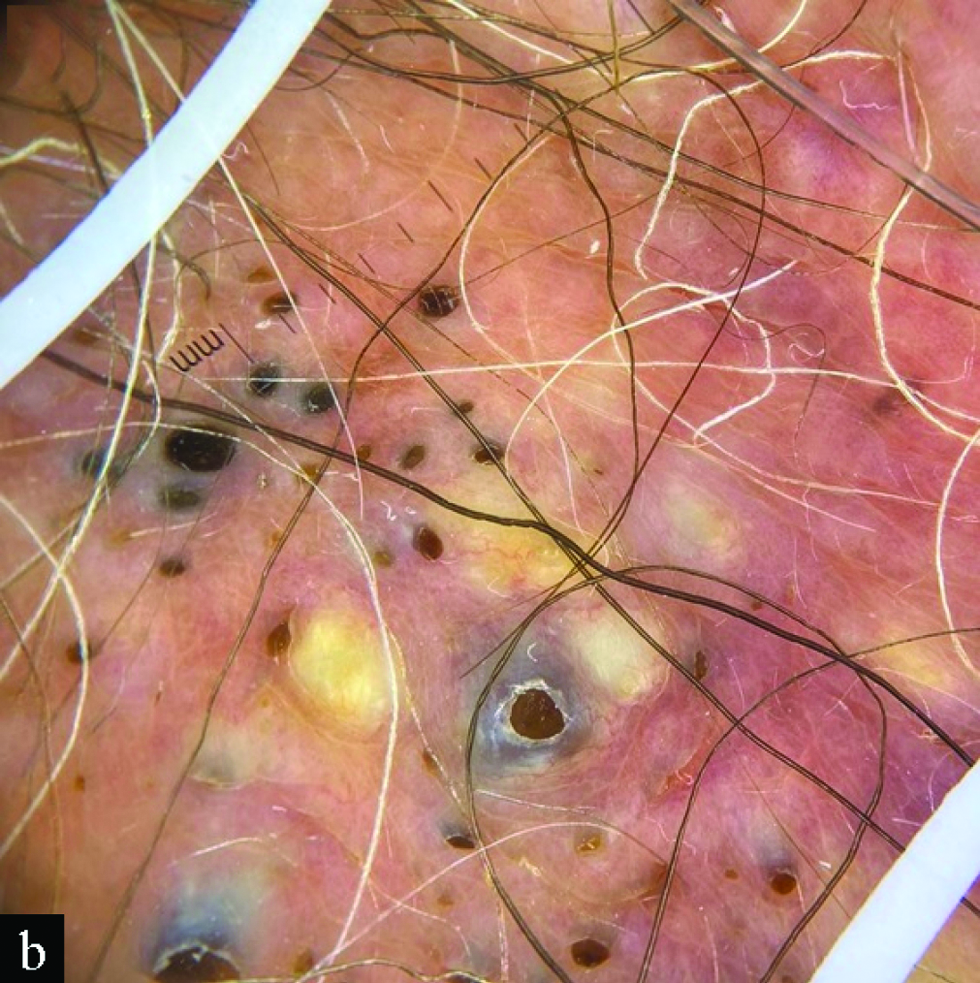
- Dermoscopy shows multiple non-melanocytic round yellowish or blue-grey papules with central or peripheral comedo-like openings
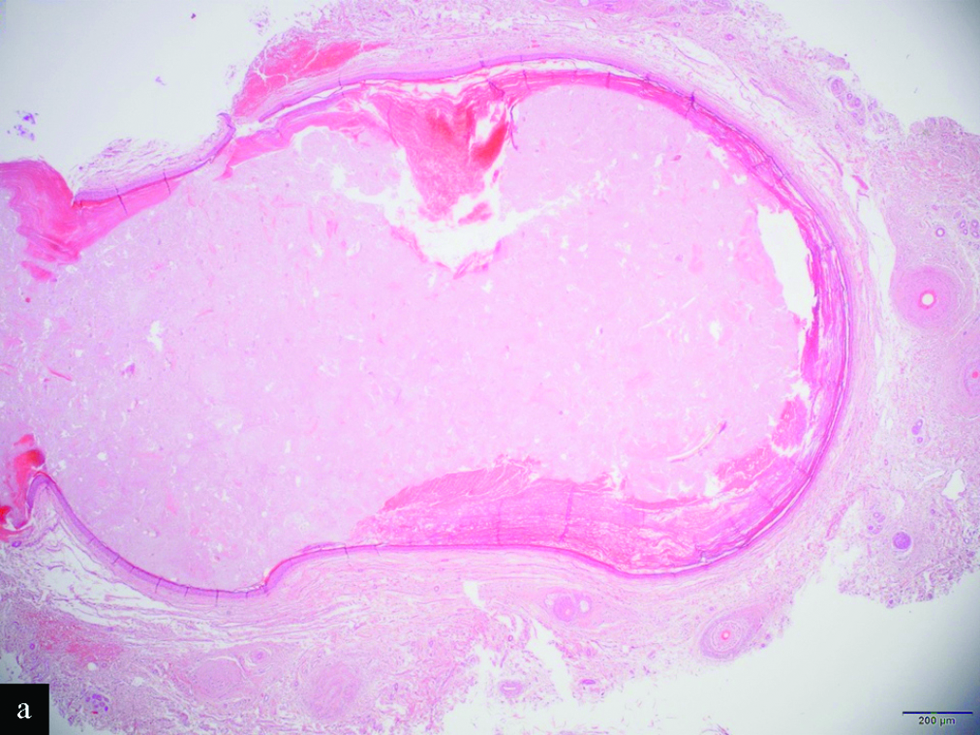
- Scanning magnification shows a mid-dermal cyst (H&E, x2)
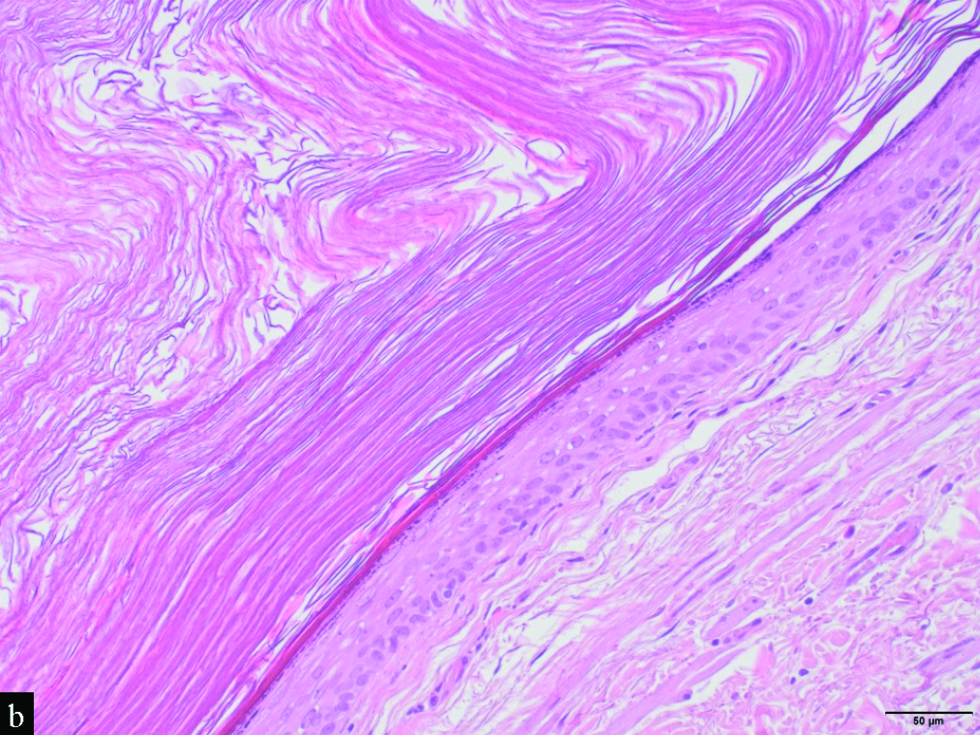
- Detail of the cystic wall, which is lined by a stratified squamous epithelium with a granular layer. Note the laminated keratin within the cyst (H&E, x20)
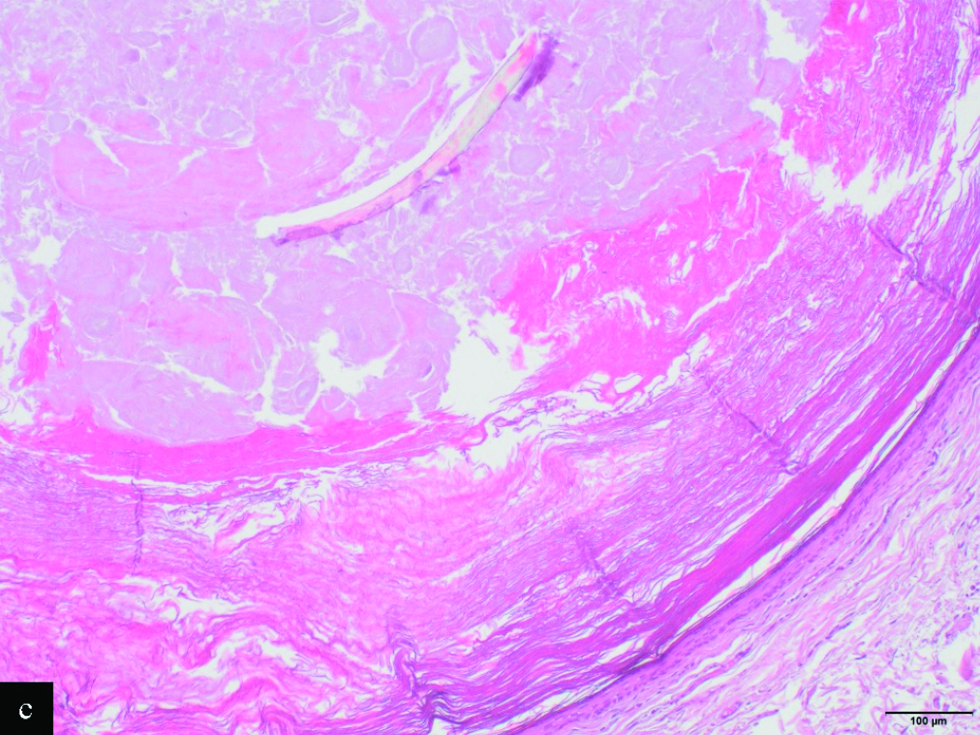
- The lumen is occupied by orthokeratin with laminated appearance, admixed with a large vellus hair shaft and keratin debris (H&E, x10)
Answer
Eruptive vellus hair cysts
Discussion
Eruptive vellus hair cysts are an uncommon condition caused by abnormal development of the infundibular portion of the hair follicle, leading to its occlusion. Clinically, they are characterized by multiple asymptomatic, 1–7 mm dome-shaped papules or nodules that are skin-coloured, erythematous, blue-grey or yellowish. Papules resembling open comedones could also be encountered. Most cases are sporadic, but 19 families affected by eruptive vellus hair cysts have been reported, with a suggested autosomal dominant inheritance with incomplete penetrance.1 More than 91% of eruptive vellus hair cysts cases appear before the age of 35, typically occurring symmetrically on the chest, abdomen or upper limbs. There are also presentations with limited involvement of the face.1 However, isolated involvement of the labia majora is rare, with very few cases published in the literature.1-3 Including ours, two of those six (33.3%) published cases showed multiple polyporous comedones, suggesting this presentation could be particularly frequent in the vulva.2
Dermoscopy of eruptive vellus hair cysts usually shows non-melanocytic, round, light yellow or blue-grey homogeneous structures, some of them surrounded by an erythematous halo and/or radiating capillaries.4 Our case additionally showed a striking open-comedo-like pattern. Oiso et al., reported bright yellow openings of these cysts to the epidermis,3 and Zhu et al., described comet-like bleary blue-grey lines next to follicular openings.5 We suggest that this presentation could represent a later stage of eruptive vellus hair cysts resulting from the oxidation of keratin and/or melanin pigment present in the exposed material.
Differential diagnosis of eruptive vellus hair cysts includes eruptive syringomas, trichogenic tumours, molluscum contagiosum, milia and comedonal acne, among others. The particular presentation in our patient should also include idiopathic calcinosis of the vulva and given the open-comedo-like appearance, epidermal inclusion cysts and a nevus comedonicus.1,2 The presence of hair and keratin within a dermal cyst lined by stratified squamous epithelium could also be suggestive of a dermoid cyst. However, they are usually congenital benign tumours that present at birth or during the first years of life, as slowly growing subcutaneous nodules located on the head and neck. The main diagnostic challenge of eruptive vellus hair cysts is their differentiation from steatocystoma multiplex. Both have an overlapping clinical appearance, may co-exist in the same patient and there are reports of hybrids cysts. Nevertheless, its histopathologic features are usually distinctive. Eruptive vellus hair cysts are lined by stratified squamous epithelium with a granular layer and contain laminated keratin and vellus hair shafts, that represent its diagnostic hallmark.1-3,5 Steatocystoma multiplex originate from the sebaceous duct rather than the infundibulum, and usually show sebaceous glands within the cyst wall, which is formed by a thin stratified squamous epithelium with undulating configuration and without or minimal granular layer. There is also a constant prominent hyaline cuticle lining the inner surface of the cyst wall. Finally, the keratin expression profile is also different between them. While steatocystoma multiplex express both K17 and K10, eruptive vellus hair cysts only express K17.1
Regarding its treatment, several options have been reported to be effective, especially topical retinoids, surgical approaches and CO2 laser.1,2,5 In our case, the larger lesions were successfully treated with CO2 laser, without recurrence at a 2-months follow-up visit.
In conclusion, eruptive vellus hair cysts should be considered in the differential diagnosis of asymptomatic papules and nodules of the vulva. Aside from yellow or blue-grey structures, open-comedo-like plugs could be encountered in the dermoscopy of eruptive vellus hair cysts and could represent a diagnostic clue in locations where acne and variants are uncommon, as in the vulva.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Eruptive vellus hair cysts: A systematic review. Am J Clin Dermatol. 2012;13:19-28.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive vellus hair cysts of the vulva. Australas J Dermatol. 2017;58:e254-55.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive vellus hair cysts of the labia majora: Detection of openings of the cysts to the epidermis by dermoscopy. Eur J Dermatol. 2013;23:417-18.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy distinction of eruptive vellus hair cysts with molluscum contagiosum and acne lesions. Pediatr Dermatol. 2012;29:772-73.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive vellus hair cysts diagnosed using dermatological imaging technique. Australas J Dermatol. 2021;62:86-88.
- [CrossRef] [PubMed] [Google Scholar]





