Translate this page into:
Asymptomatic skin coloured plaques over the lower limbs
Correspondence Address:
Amrinder J Kanwar
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh-160 012
India
| How to cite this article: Kumaran MS, Dogra S, Kanwar AJ. Asymptomatic skin coloured plaques over the lower limbs. Indian J Dermatol Venereol Leprol 2005;71:374-378 |
 |
 |
 |
 |
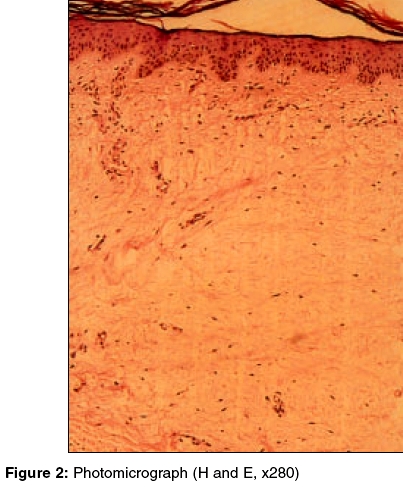
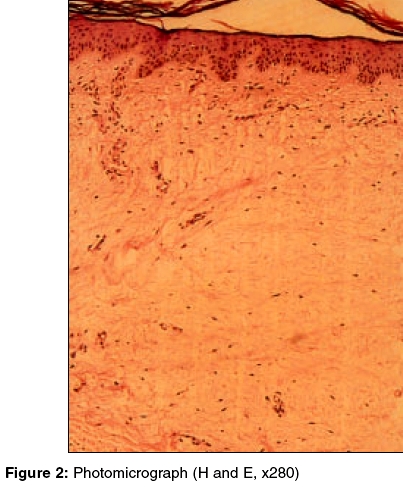
A 40-year-old female presented with two asymptomatic plaques over her left shin of one year′s duration. Clinical examination revealed two, skin coloured, almost annular, well defined plaques, located over the anterolateral aspect of the left shin, measuring about 2 cm in diameter. Surrounding the lesions were a few areas of localized hypertrichosis [Figure - 1]. Examination of other body parts, including the mucosae, hair, and nails, did not reveal any abnormality.
Her past medical history was significant for Graves′ disease for 10 years, for which she was started on oral carbimazole. However, three years later, she developed hypothyroidism for which she was receiving oral L-thyroxine. There was no history of any topical medication for the skin lesions.
The routine hematological and biochemical investigations, including the lipid profile, were within normal limits. Her thyroid hormone profile (radioimmunoassay) showed TSH, 38.8 mu/L (n = 0.5-4.5 mu/L); T3, 1.45 nmol/L (n=1.1-2.9 nmol/L) and T4, 50.7 nmol/L (n = 64-154 nmol/L). Skin biopsy was taken for histopathological examination [Figure - 2].
What is the diagnosis?
Diagnosis: Pretibial myxedema
Discussion
Microscopic examination (H and E) of the biopsied tissue revealed thinned out epidermis and edema of the dermis. Mucin deposition was seen in the dermis extending towards the subcutis along with a minimal chronic inflammatory infiltrate [Figure - 2]. Alcian blue staining confirmed the presence of mucin. These features were consistent with pretibial myxedema (PM). The lesions were treated with twice daily application of topical clobetasol propionate ointment with minimal improvement
Graves′ disease is a triad of hyperthyroidism with diffuse goiter, ophthalmopathy and dermopathy, either alone or in combination. The natural course of these manifestations is independent of each other. The onset can occur at any age and females are more commonly affected. PM is more aptly called thyroid dermopathy as it may appear anywhere on the body. Dermopathy is present in up to 4.4% of patients with Graves′ disease and 15% have associated opthalmopathy.[1] The vast majority of patients with PM have Graves′ disease, but it has also been described in hypothyroid states like Hashimoto′s thyroiditis. Thus, the thyroid status of a patient is not strictly related to the development of PM, and it has been reported in euthyroidism, hyperthyroidism or in hypothyroidism.[2] Our patient had hypothyroidism when she presented with PM.
Pretibial myxedema may present as localized erythematous to skin coloured nodules or plaques or rarely a diffuse elephantiasis pattern. Though the pretibial area is the classical site of involvement in PM, rarely it has been reported in unusual locations such as the forearms, shoulders, arms, palms, upper back, neck, pinnae and lower part of the abdomen.[3] Rarely, PM may present with overlying hyperhidrosis or hypertrichosis.[2] However, in our patient the hypertrichosis was localized around the lesions. Hypertrichosis in our patient of pretibial myxedema (which is usually associated with hyperthyroidism) could be related to her hypothyroid status as hypertrichosis has been reported with hypothyroidism without pretibial myxedema.[4] Just as pretibial myxedema is thought to be due to stimulation of fibroblasts at the site to produce mucin , hypertrichosis could also be due to stimulation of vellus hair follicles by fibroblasts which turn them into terminal hair.
The precise pathogenesis of PM is still enigmatic, but fibroblasts may play a role. TSH and TSH-R antibody binding sites have been reported on the plasma membranes of fibroblasts derived from skin of PM. It is still unclear why the fibroblasts are activated at these sites and the evidence for site-specific and generalized fibroblast activation is conflicting. However, it has been reported that fibroblasts in the lower limbs are more sensitive to serum fibroblast factor than fibroblasts from other sites. In contrast, a few studies have concluded that ophthalmopathy and PM are primarily caused by local factors (particularly in the orbit) superimposed on a systemic, low-grade connective tissue inflammation.[5] Heat shock proteins (HSP70) have been reported to be differently expressed by the fibroblasts from affected sites. These proteins may play a role in a localized immune process leading to PM.[6] Recently, a thyroid hormone (T3) response gene, ZAK1-4, has been cloned in human fibroblasts, but its role in the pathogenesis remains to be determined.[3]
Treatment of PM is difficult. It has been reported to resolve spontaneously in approximately 3.5 years.[7] Steroids (topical, intralesional, oral, or intravenous), pentoxyfylline, intravenous immunoglobulins, plasmapharesis, immunotherapy and octreotide have been used with varied success rates. Recurrence has been reported following surgical excision.
Little is known about the long-term outcome of patients with thyroid dermopathy. Fatourechi et al reviewed 150 cases of thyroid dermopathy over 20 years and found that it was a late manifestation of Graves′ disease and that its onset usually followed the diagnosis of hyperthyroidism and opthalmopathy.[1] In another review of 178 patients by Schwartz et al, 26% of patients with PM experienced complete remission in a mean period of 7.9 years, with no effect of topical steroids on long-term resolution of the lesions.[8]
| 1. |
Fatourechi V, Pajouhi M, Fransway AF. Dermopathy of Graves disease (pretibial myxedema). Review of 150 cases. Medicine 1994;73:1-7.
[Google Scholar]
|
| 2. |
Heymann WR. Advances in the cutaneous manifestations of thyroid disease Int J Dermatol 1997;36:641-5.
[Google Scholar]
|
| 3. |
Heymann WR. Cutaneous manifestations of thyroid disease. J Am Acad Dermatol 1992;26:885-902.
[Google Scholar]
|
| 4. |
Stern SR, Kelnar CJ. Hypertrichosis due to primary hypothyroidism. Arch Dis Child 1985;60:763-6.
[Google Scholar]
|
| 5. |
Rapoport B, Alsabeh R, Aftergood D, McLachlan SM. Elephantiasic pretibial myxedema: insight into and a hypothesis regarding the pathogenesis of the extrathyroidal manifestations of Graves' disease. Thyroid 2000;10:685-92.
[Google Scholar]
|
| 6. |
Heufelder AE, Wenzel BE, Gorman CA, Bahn RS. Detection, cellular localization, and modulation of heat shock proteins in cultured fibroblasts from patients with extrathyroidal manifestations of Graves' disease. J Clin Endocrinol Metab 1991;73:739-45.
[Google Scholar]
|
| 7. |
Lang PG, Sisson JC, Lynch PJ. Intralesional triamcinolone therapy for pretibial myxedema. Arch Dermatol 1975;111:197-202.
[Google Scholar]
|
| 8. |
Schwartz KM, Fatourechi V, Ahmed DD, Pond GR. Dermopathy of Graves' disease (pretibial myxedema): long-term outcome. J Clin Endocrinol Metab 2002; 87:438-46.
[Google Scholar]
|
Fulltext Views
1,666
PDF downloads
3,430





