Translate this page into:
Atypical fibroxanthoma successfully treated with a single dose of cemiplimab
Corresponding author: Dr. Chiara Battilotti, Dermatology Unit, Department of Clinical Internal, Anesthesiological and Cardiovascular Sciences, Sapienza University of Rome, Italy. chiara.battilotti@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Proietti I, Battilotti C, Fiorentino F, Svara F, Potenza C. Atypical fibroxanthoma successfully treated with a single dose of cemiplimab. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1514_2024
Dear Editor,
Atypical fibroxanthoma (AFX) is a rare tumour with intermediate clinical behaviour, typically occurring in sun-exposed skin of elderly, fair-skinned males. It is classified as a dermal mesenchymal neoplasm of uncertain differentiation and is considered to be a part of the same pathological spectrum as pleomorphic dermal sarcoma (PDS).1
We describe the case of a 93-year-old man with advanced non-small cell lung carcinoma (NSCLC) presenting with a scalp lesion that appeared six months earlier. His medical history included hypothyroidism, diabetes mellitus, atrial fibrillation, and senile dementia. He was undergoing treatment with levothyroxine, metformin, rivastigmine, and diazepam. Physical examination revealed an enlarging 4.2 cm x 3.8 cm erythematous and crusted plaque in the left parietal region [Figure 1]. Initially nodular, the lesion bled following trauma and subsequently flattened. The dermoscopic examination was limited to crusting, revealing only haemorrhagic scales on an erythematous background with structureless red and white areas and out-of-focus polymorphous vessels. An incisional biopsy was performed, and the patient began cemiplimab immunotherapy for NSCLC the following day. Histopathological analysis showed a dense infiltrate of irregularly arranged spindled-to-epithelioid cells with marked pleomorphism and numerous mitotic figures [Figure 2]. Immunohistochemistry revealed CD68 positivity, while CD34, CD45, S-100, MelanA, HMB-45, MART1, and Cytokeratin AE1/AE3 were negative, confirming AFX diagnosis. AFX is a diagnosis of exclusion with a nonspecific immunohistochemical marker profile. The utility of negative IHC markers is critical in ruling out other common neoplasms, such as melanoma (S-100, HMB-45 negativity), epithelial malignancies (AE1/AE3, CK5/6 negativity), dermatofibrosarcoma protuberans (CD34 negativity), and haematopoietic malignancies (CD45 negativity). Six weeks post-biopsy and prior to the second cemiplimab infusion, the patient was re-evaluated to schedule the radical excision of the lesion. No topical treatment was administered during the intermittent period. However, the examination revealed only an erythematous area with minimal crusting [Figure 3a]. A second incisional biopsy was performed, and the histological examination revealed an intense intradermal inflammatory infiltrate [Figure 3b]. No recurrences were observed during the 12-month follow-up.

- Crusted plaque measuring 4.2 cm x 3.8 cm on the left parietal region of the scalp. (inset) Close-up of the lesion.
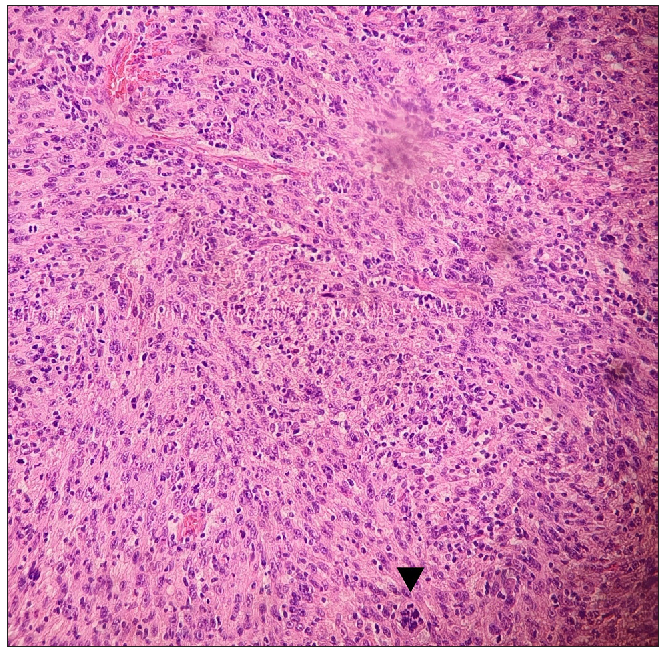
- Histopathological image showing highly cellular neoplasia composed of irregularly arranged spindled to epithelioid cells with marked pleomorphism and numerous mitotic figures, including atypical forms (black arrowhead). (Haematoxylin & eosin, 100x).

- Complete remission of the lesion after a single dose of cemiplimab. Photo taken 6 weeks after cemiplimab infusion.
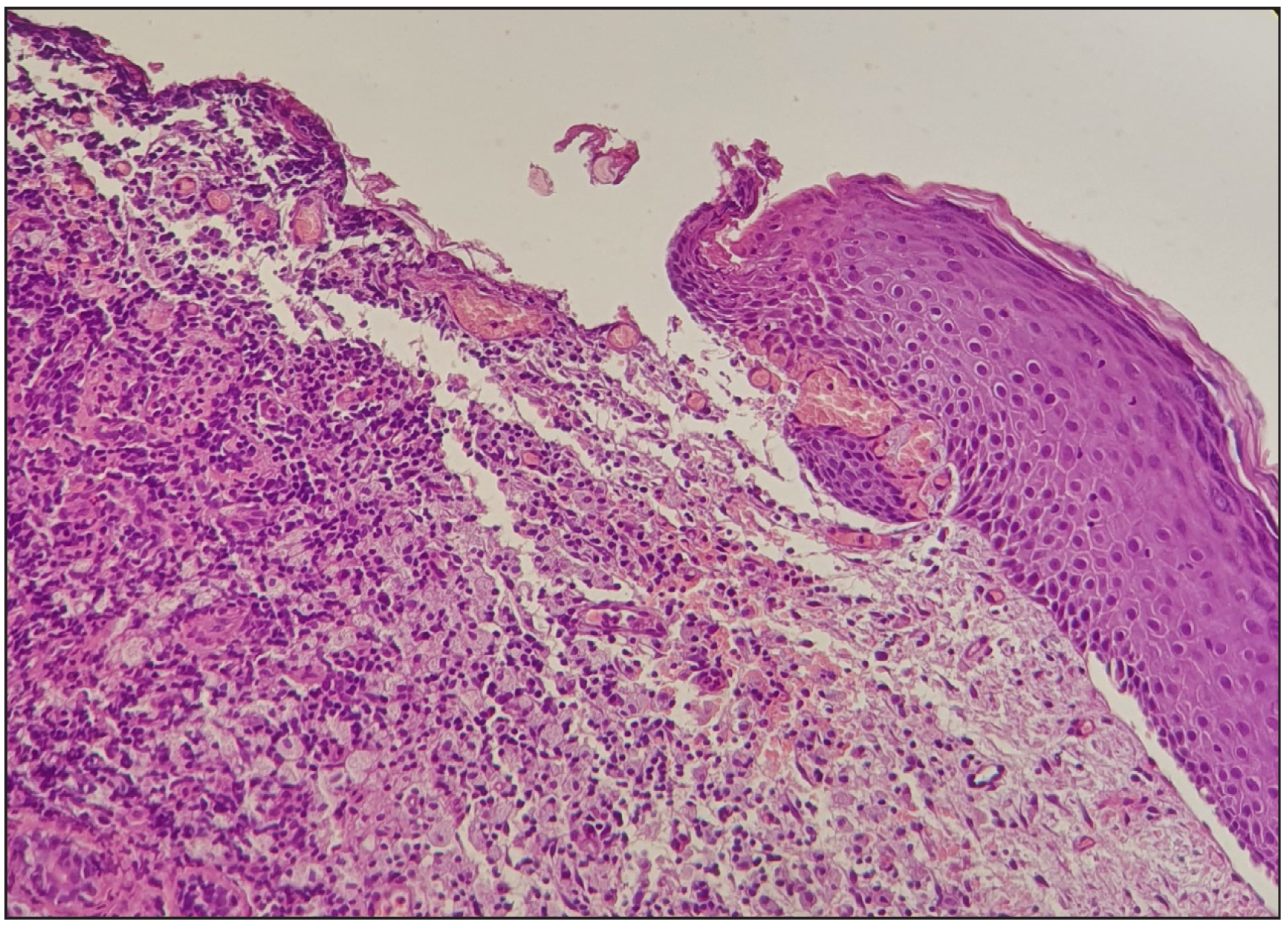
- Histopathological image of epidermal erosion and abundant chronic inflammation predominantly composed of lymphocytes and histiocytes with mild fibrosis in the dermis. (Haematoxylin & eosin, 100x).
AFX is an uncommon tumour predominantly affecting elderly individuals with a history of prolonged UV exposure. The most commonly affected sites include the scalp, ears, and face. Clinically, it usually presents as a rapidly growing, painless, often ulcerated, non-pigmented nodule. Histologically, AFX consists of pleomorphic spindle and epithelioid cells with prominent mitotic activity and marked atypia. An IHC panel is critical for excluding other malignancies, such as melanoma, cSCC (Cutaneous squamous cell carcinoma), and DFSP (Dermatofibrosarcoma protuberans). Importantly, AFX must be differentiated from PDS (Pleomorphic dermal sarcoma), which, by contrast, demonstrates necrosis, subcutaneous involvement, and perineural invasion. AFX diagnosis is particularly challenging due to its clinical resemblance to more common malignant skin neoplasms and the lack of specific dermoscopic features. Moreover, histopathological evaluation alone may not be conclusive, as AFX shares morphological characteristics with other spindle-cell neoplasms. Therefore, a comprehensive diagnostic approach integrating clinical, histopathological, and immunohistochemical findings is crucial for definitive diagnosis and appropriate management. Mohs micrographic surgery or wide local excision with at least a 0.5 cm margin is the treatment of choice, with a 5-year risk of local recurrence and metastasis of approximately 10% and 1%, respectively.2,3 In case of unresectable, recurrent, or metastatic disease, the therapeutic options include radiation therapy and chemotherapy.4 AFX is characterised by a high tumour mutation burden with a UV signature, which is even higher than in other UV-induced skin tumours, such as cSCC. Additionally, gene mutation and expression analyses demonstrate that AFX/PDS shares a very high similarity with cSCC.5 It is, therefore, reasonable to consider that therapies effective for cSCC may also be beneficial for AFX. In fact, recent case reports have documented the efficacy of a topical combination of imiquimod, tazarotene, and 5-fluorouracil, as well as pembrolizumab, for treating AFX and advanced PDS, respectively.6,7 Cemiplimab is a monoclonal antibody targeting the programmed cell death 1 (PD-1) receptor approved for patients with locally advanced or metastatic cSCC, basal cell carcinoma, and NSCLC. It enhances T-cell-mediated immune responses, leading to T-cell activation and proliferation against the tumour cells. The potential effectiveness of cemiplimab against AFX is supported by the high mutation burden of this neoplasm, which makes it more sensitive to effector T-cells in the contest of immune checkpoint blockade. To the best of our knowledge, this is the first case report of AFX successfully treated with cemiplimab. Our clinical case demonstrated that a single infusion of cemiplimab led to complete response in a patient with AFX, suggesting that it may be a powerful and effective therapeutic option in treating this rare cutaneous tumour.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- International Agency for Research on Cancer. WHO Classification of Tumours Online. WHO 5th classification of skin tumors [beta version ahead of print]. Available from: https://tumourclassification.iarc.who.int, Last accessed September 10, 2024.
- S1-guideline atypical fibroxanthoma (AFX) and pleomorphic dermal sarcoma (PDS) J Dtsch Dermatol Ges. 2022;20:235-43.
- [Google Scholar]
- Atypical fibroxanthoma and pleomorphic dermal sarcoma: Local recurrence and metastasis in a nationwide population-based cohort of 1118 patients. J Am Acad Dermatol. 2023;89:1177-84.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical fibroxanthoma and pleomorphic dermal sarcoma: Updates on classification and management. Dermatol Clin. 2019;37:253-9.
- [CrossRef] [PubMed] [Google Scholar]
- Immune checkpoint inhibitors for unresectable or metastatic pleomorphic dermal sarcomas. Front Oncol. 2022;12:975342.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Atypical fibroxanthoma treated with a topical combination of imiquimod, tazarotene, and 5-fluorouracil. Dermatol Ther (Heidelb). 2024;14:1049-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- First report on two cases of pleomorphic dermal sarcoma successfully treated with immune checkpoint inhibitors. Oncoimmunology. 2019;8:e1665977.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






