Translate this page into:
Atypical generalized morphea-like scleroderma occurring in a patient exposed to organic solvents and having chronic hepatitis C virus infection
2 Sousse University; Department of Gastro-Enterology, Sahloul Hospital, Sousse University, Sousse, Tunisia
3 Sousse University; Department of Immunology, Farhat Hached Hospital, Sousse University, Sousse, Tunisia
4 Sousse University; Department of Occupational Health, Farhat Hached Hospital, Sousse University, Sousse, Tunisia
5 Sousse University; Department of Pathology, Farhat Hached Hospital, Sousse University, Sousse, Tunisia
Correspondence Address:
Ines Lahouel
Department of Dermatology, Farhat Hached Hospital, Ibn El Jazzar Street 4000
Tunisia
| How to cite this article: Aounallah A, Lahouel I, Mokni S, Ksiaa M, Hayouni M, Belajouza C, Kotti F, Saidi W, Boussofara L, El Maalel O, Guerfala M, Sriha B, Denguezli M, Ghariani N, Nouira R. Atypical generalized morphea-like scleroderma occurring in a patient exposed to organic solvents and having chronic hepatitis C virus infection. Indian J Dermatol Venereol Leprol 2018;84:221-224 |
Sir,
Generalized morphea-like scleroderma has been proposed as a subtype of diffuse cutaneous systemic sclerosis among people exposed to organic solvents.[1] Chronic hepatitis C virus (HCV) infection has been associated with many dermatologic conditions, including systemic sclerosis and localized scleroderma (morphea).[2],[3] We did not find any previous reports of generalized morphea-like scleroderma associated with HCV infection. Here, we describe an interesting case of atypical generalized morphea-like scleroderma occurring in a patient having chronic HCV infection and occupational exposure to organic solvents.
A 45-year-old male was referred to our department of dermatology for management of sclerotic plaques on the face and trunk. He had a history of occupational exposure to organic solvents (aliphatic hydrocarbons) for 7 years. He did not have any relevant history or predisposing factors for autoimmune diseases. One year earlier, he had noticed “tightness” of the skin on face, neck and back that got progressively worse. The patient complained of photosensitivity and dysphagia to solids. General physical examination was normal. Cutaneous examination showed sclerotic, hyperpigmented, plaques of 3–5 cms diameter [Figure - 1]. The lesions were distributed on the back, abdomen, neck, axillary folds, thigh and penis, and were associated with sclerosis of the upper face along with lower eyelid ectropion [Figure - 2]. The patient did not have sclerodactyly. Systemic examination was normal.
 |
| Figure 1: Sclerotic, hyper pigmented, plaques of 3 to 5 cms in diameter located in the back |
 |
| Figure 2a: Sclerosis of the upper face with lower eyelid ectropion, Front view |
 |
| Figure 2b: Sclerosis of the upper face with lower eyelid ectropion, Profile view |
Laboratory tests including blood cell count, C-reactive protein, renal function tests and hepatobiliary enzyme levels were normal. Protein electrophoresis showed polyclonal hypergammaglobulinemia (chronic inflammatory disease profile). Antinuclear antibodies (ANA) (1/3200) and anti-centromere antibodies were positive (1/300). Anti-ds DNA and anti-scl70 antibodies were negative. Serology test for hepatitis B virus was negative, but it was positive for hepatitis C virus with a very high HCV viral load (1,330,000 IU/ml). Capillaroscopy showed minor capillary dystrophies without specific signs of microangiopathy. Skin biopsy showed hyperkertosis with orthokeratosis. The dermis was thickened and eccrine glands were abnormally situated within the upper dermis. Collagen fibers were broadened [Figure - 3]. A mild inflammatory cell infiltrate was present in the superficial dermis. Pulmonary function test showed a restrictive ventilatory deficit not associated with an abnormality of the alveolocapillary distribution, which was in favor of parietal origin of the restriction. Esophageal manometry showed a major hypotonia of the lower esophageal sphincter associated with retained overlying traction. Accordingly, the patient was diagnosed with generalized morphea-like scleroderma.
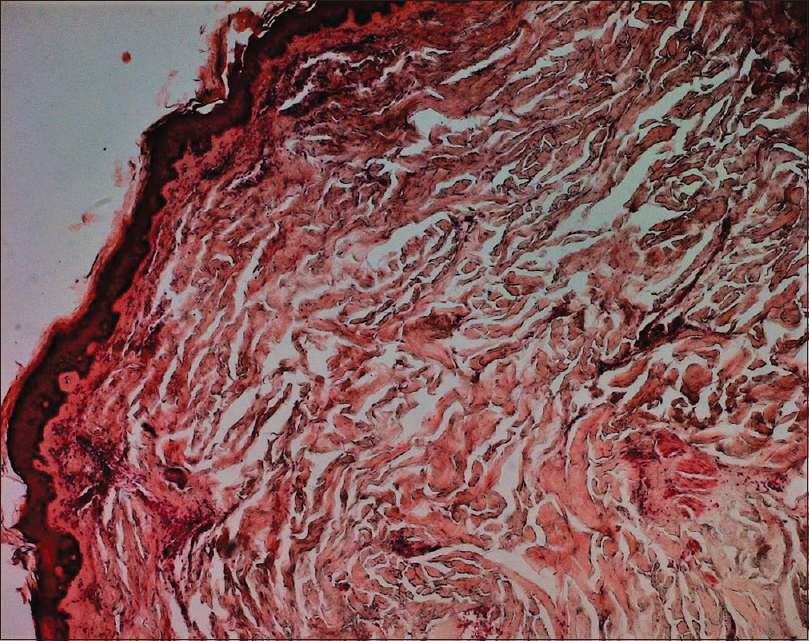 |
| Figure 3: Marked thickening of the dermal collagen (H and E ×400) |
Generalized morphea-like scleroderma has features that include male predominance, rapid progression, high incidence of exposure to organic solvents and low incidence of internal organ involvement compared with the usual diffuse systemic sclerosis or scleroderma.[4] All these criteria were present in the case described here. Clinical features include symmetrical skin sclerosis demarcated from the surrounding areas, with an erythematous border and involving the upper lateral forearms, lumbar area and back.[4] Compared with generalized morphea-like scleroderma, sclerodactyly and visceral involvement are not observed in the usual generalized morphea patients.[5] The case described here is atypical due to the localization of the sclerosis on the upper face associated with lower eyelid ectropion and the absence of sclerodactyly. Previous authors have reported an association between organic solvent exposure and increased risk of systemic sclerosis. A meta-analytic review estimated the risk for occupational exposure to organic solvent being 2.4 (95% CI 1.7–3.4) in systemic sclerosis.[6] The pathogenic mechanisms of organic solvents in the onset of systemic sclerosis remains unclear. It has been suggested that organic solvents may link with nucleic acids and proteins, resulting in immune disruptors and increased risk of systemic sclerosis.[6]
Generalized morphea-like scleroderma was first proposed as a unique subtype of diffuse systemic sclerosis in people exposed to organic solvents.[1] The development of a sclerodermatous condition has been suggested to be associated with exposure to various environmental agents, drugs (anti-cancer agents), irradiation and professional exposure to solvents, as in the case described here. These agents might damage endothelial cells and activate T cells with secretion of cytokines and chemokines, modulating the production of extracellular matrix proteins by fibroblasts.[2]
Chronic HCV infection has been associated with lichen planus, porphyria cutanea tarda, cutaneous necrotizing vasculitis, erythema nodosum and multiforme, urticaria, morphea and systemic sclerosis.[2],[3] In studies reporting the association of viral hepatitis and systemic sclerosis, the role of interferon therapy has been discussed.[2] Only a few cases of a sclerodermatous condition associated with HCV infection have been published.[2],[3] As the case presented here is atypical from the classical generalized morphea-like scleroderma associated with exposure to solvents, we suggest that HCV possibly caused the condition. To our knowledge, generalized morphea-like scleroderma associated with HCV infection has not been reported in literature.
The role of HCV infection in the pathogenesis of sclerodermatous condition is unknown. It is possible that the replication of HCV outside the liver, particularly in mononuclear cells, may suppress immune tolerance in genetically predisposed individuals.[2] Extrahepatic effects could be caused by circulating immune complexes depositing in tissues, viral antigens inducing autoantibodies reacting with local tissue antigens or the virus reacting directly on local tissue.[2],[3]
Generalized morphea-like scleroderma described here is a rare entity associated with exposure to organic solvents, and its association with HCV infection has not been reported before.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Yamakage A, Ishikawa H. Generalized morphea-like scleroderma occurring in people exposed to organic solvents. Dermatology 1982;165:186-93.
[Google Scholar]
|
| 2. |
Abu-Shakra M, Sukenik S, Buskila D. Systemic sclerosis: Another rheumatic disease associated with hepatitis C virus infection. Clin Rheumatol 2000;19:378-80.
[Google Scholar]
|
| 3. |
Mihas AA, Abou-Assi SG, Heuman DM. Cutae morphea associated with chronic hepatitis C. J Hepatol 2003;39:458-9.
[Google Scholar]
|
| 4. |
Nagai Y, Igarashi N, Ishikawa O. Generalized morphea-like systemic sclerosis: A subtype of diffuse cutaneous systemic sclerosis presenting with unusual cutaneous features. Eur J Dermatol 2008;18:715-6.
[Google Scholar]
|
| 5. |
Taniguchi Y, Okazaki M, Kagawa T, Nakajima K, Nakajima H, Terada Y, et al. Atypical generalized morphea-like scleroderma presenting deep sclerosis on the fingers. Mod Rheumatol 2011;21:232-4.
[Google Scholar]
|
| 6. |
Miller FW, Alfredsson L, Costenbader KH, Kamen DL, Nelson LM, Norris JM, et al. Epidemiology of environmental exposures and human autoimmune diseases: Findings from a National Institute of Environmental Health Sciences Expert Panel Workshop. J Autoimmun 2012;39:259-71.
[Google Scholar]
|
Fulltext Views
4,204
PDF downloads
2,041





