Translate this page into:
Author's reply: Significance of seropositivity for syphilis in asymptomatic individuals
Correspondence Address:
Sarita Sasidharanpillai
'Rohini', Girish Nagar, Nallalom PO, Kozhikode - 673 027, Kerala
India
| How to cite this article: Sasidharanpillai S, Bindu V, Riyaz N, Beegum Sherjeena PV, Rahima S, Chandrasekhar N. Author's reply: Significance of seropositivity for syphilis in asymptomatic individuals. Indian J Dermatol Venereol Leprol 2015;81:179-181 |
Sir,
We thank the author for his interest in our article entitled "Syphilis among sexually transmitted infections (STIs) clinic attendees in a tertiary care institution: A retrospective data analysis" and for raising certain valid points. [1] Except in the early stage of infection where dark ground microscopy can aid in the detection of causative treponems in material collected from the lesion, serology remains the mainstay of diagnosis in syphilis.
In our institution all patients attending the STIs clinic are offered Venereal Disease Research Laboratory (VDRL) test screening for syphilis with a repeat testing (irrespective of the initial titer) after 3 weeks to detect any rise in titers. Dark ground microscopic examination is carried out wherever indicated.
Patients who manifest a VDRL titer equal to or more than 1:4 with no clinical evidence of syphilis are routinely advised confirmation by Treponema pallidum hemagglutination (TPHA) test as per the recommendations of World Health Organization (WHO). [2] Though some consider a VDRL titer of 1:8 or more as true reactive, [3] it has been documented that VDRL titer below 1:8 should not be taken as negative if confirmed by a positive TPHA. [4],[5]
A positive TPHA with non-reactive or weekly reactive VDRL may be seen in treated patients or in late stages of syphilis. [6] Persistence of positive serology in the treated (serofast reaction) poses a problem in distinguishing between untreated late latent syphilis patients from those showing serofast reaction. Centers for Disease Control and Prevention (CDC) recommends that the decision on such instances should be taken on the basis of history of adequate treatment. [6]
Accordingly in our centre, all asymptomatic untreated TPHA positive patients were considered as latent syphilis and those who were unable to recollect the time interval between the time of detection of positive serology and the time of diagnosis of early infective syphilis in themselves or in a sexual partner or those who did not give a history of diagnosis of syphilis in the past were grouped under syphilis of unknown duration (SUD).
All clinically or serologically diagnosed syphilis cases attending our STI clinic were assessed for any ophthalmologic or central nervous system manifestations of syphilis. Those with central nervous system or ophthalmologic manifestations of syphilis and those with co-existing human immunodeficiency virus (HIV) infection were recommended cerebrospinal fluid (CSF) analysis to rule out neurosyphilis. The two neurosyphilis cases in our study were detected following CSF study performed in patients with syphilis of unknown duration who complained of dimness of vision and headache, respectively. All the late syphilis cases were evaluated with electrocardiography and echocardiogram with the help of a cardiologist to rule out cardiovascular syphilis. None of our study population were found to have this complication.
We tried to avoid misdiagnosis of serofast reactions as syphilis of unknown duration by enquiring about previous treatment. But we cannot rule out the possibility of false positive reactions in at least some of our patients. Though not as common as with VDRL, false positive results can occur with TPHA. [7] CDC recommends that Treponema pallidum particle agglutination assay (TP-PA) should be used as the confirmatory test in doubtful cases. [6],[8] But this was not possible in our set up due to financial constraints. Hence we managed these patients as late latent syphilis (after ruling out cardiovascular and neurosyphilis) so as to avoid complications of untreated disease.
Nearly 50% of our patients were referred to us following positive serology for syphilis detected during mandatory medical checkup for going abroad, which was not surprising as they underwent both VDRL and TPHA testing, unlike in our STI clinic where TPHA test is offered only to those with VDRL reactivity 1:4 or more. This might lead to missing detection of some of the late latent syphilis cases. Recently some centers have opted for using treponemal test as the initial screening test to detect all the late latent cases and subsequent non-treponemal test to assess disease activity (reverse sequence screening). [6]
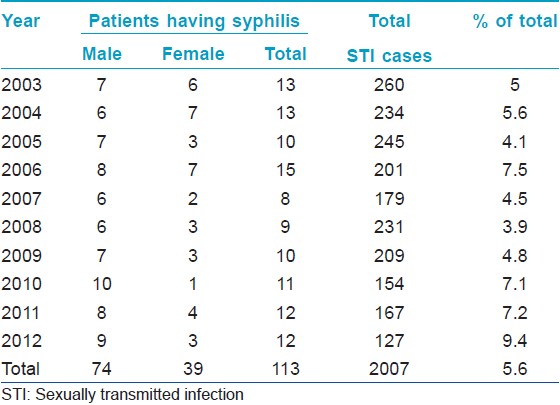
The reduction noted in the number of patients attending our institution with STIs during the past decade was not reflected in syphilis cases. A reduction in the early years of the decade was followed by a gradual increase in syphilis cases in the latter half [Table - 1]. In fact, the rise in total syphilis cases in the past couple of years was due to an increase in early stage disease as seven of the eight early syphilis cases were diagnosed in the last 3 years. The number of cases with syphilis of unknown duration has remained more or less the same over the past 6 years. A similar observation has been made by others. [9] We believe this to be a disturbing finding pointing to the rise in active disease transmission in the community since for each infective stage disease seen in a tertiary centre there will be several hidden cases in the community. Many such patients may either get partial treatment due to the widespread use of penicillins and cephalosporins nowadays for several common ailments or go untreated and remain in asymptomatic latency.
′Prenatal syphilis′ is used to denote syphilis transmitted to the fetus in utero by the infected mother and is considered to be a better terminology than congenital syphilis. [10],[11]
We suggest that all STI patients should be offered screening for syphilis with both VDRL and TPHA tests so as to detect all late latent syphilis cases.
| 1. |
Saidharanpillai S, Bindu V, Riyaz N, Beegum Sherjeena PV, Rahima S, Chandrasekhar N. Syphilis among sexually transmitted infections clinic attendees in a tertiary care institution: A retrospective data analysis. Indian J Dermatol Venereol Leprol 2014;80:161-2.
[Google Scholar]
|
| 2. |
World Health Organization. Treponemal infections. Technical reports series 674. Geneva: WHO; 1982.
[Google Scholar]
|
| 3. |
Thakar YS, Chande C, Mahalley AD, Saoji AM. Seroprevalence of syphilis by TPHA test. Indian J Pathol Microbiol 1996;39:135-8.
[Google Scholar]
|
| 4. |
Bala M, Toor A, Malhotra M, Kakran M, Murlidhar S, Ramesh V. Evaluation of the usefulness of Treponema pallidum haemagglutination test in the diagnosis of syphilis in weak reactive Venereal Disease Research Laboratory sera. Indian J Sex Transm Dis 2012;33:102-6.
[Google Scholar]
|
| 5. |
Archana BR, Prasad SR, Beena PM, Okade R. Making serological diagnosis of syphilis more accurate. Indian Sex J Transm Dis 2014;35:70-1.
[Google Scholar]
|
| 6. |
Centers for Disease Control and Prevention. Discordant Results from Reverse Sequence Syphilis Screening - Five Laboratories, United States, 2006-2010 MMWR MMWR Morb Mortal Wkly Rep 2011;60:133-7.
[Google Scholar]
|
| 7. |
Garner MF, Backhouse JL, Daskalopoulos G, Walsh JL. The Treponema pallidum haemagglutination (TPHA) test in biological false positive and leprosy sera. J Clin Pathol 1973;26:258-60.
[Google Scholar]
|
| 8. |
Cole MJ, Perry KR, Parry JV. Comparative evaluation of 15 serological assays for the detection of syphilis infection. Eur J Clin Microbiol Infect Dis 2007;26:705-13.
[Google Scholar]
|
| 9. |
Ray K, Bala M, Gupta SM, Khunger N, Puri P, Muralidhar S, et al. Changing trends in sexually transmitted infections at a Regional STD Centre in north India. Indian J Med Res 2006;124:559-68.
[Google Scholar]
|
| 10. |
Sanchez M. Syphilis. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, Editors. Dermatology in General Medicine. 7 th ed. New York: McGraw- Hill 2008. p. 1955-77.
[Google Scholar]
|
| 11. |
Siddappa K, Ravindra K. Syphilis and Nonvenereal Treponematoses. In: Valia RG, Valia AR, Editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 1803-47.
[Google Scholar]
|
Fulltext Views
4,279
PDF downloads
1,456





