Translate this page into:
Bacillary angiomatosis presenting as a digital ulcer
Correspondence Address:
Jo�o V�tor Pina Alves
Av. Torrado da Silva; 2801-951 Almada
Portugal
| How to cite this article: Alves JV, Matos DM, Furtado CM, Fernandes B�rtolo EF. Bacillary angiomatosis presenting as a digital ulcer. Indian J Dermatol Venereol Leprol 2015;81:398-400 |
Sir,
Bacillary angiomatosis is a rare infectious vasculoproliferative disorder caused by Bartonella henselae or Bartonella quintana. [1] This condition was first described by Stoler et al., in 1983 as a cutaneous or disseminated infection in patients infected with human immunodeficiency virus (HIV). [2] Bacillary angiomatosis is mostly seen in advanced stages of acquired immune deficiency syndrome (AIDS) with a CD4 count less than 200 cells/mm3. [1] The most common site of the infection is the skin but lesions may also occur in liver, lymph node, soft tissue and bone. [1],[3]
We report a case of a 42-year-old HIV-seropositive male construction worker on irregular treatment with antiretroviral therapy (zidovudine, lamivudine, and lopinavir/ritonavir) for the past 2 years. He presented with an asymptomatic ulcer involving the distal phalanx of his left fourth finger for 1 year. The patient was otherwise well and denied fever, malaise or weight loss. Physical examination revealed the presence of a solitary ulcer with irregular borders and a fibrino-necrotic floor occupying the dorsal aspect of the distal phalanx of left ring finger with loss of nail plate [Figure - 1]. There was no lymphadenopathy or palpable hepatosplenomegaly. The clinical differential diagnosis included squamous cell carcinoma and an infectious condition. Skin biopsies were sent for histopathological and microbiological examination. Histological examination showed lobular proliferations of small blood vessels with a diffuse, predominantly perivascular, inflammatory infiltrate composed of neutrophils, lymphocytes and histiocytes with abundant nuclear debris involving the superficial and deep dermis [Figure - 2]a-c. Warthin-Starry stain demonstrated the presence of solitary and clustered bacilli in the dermis [Figure - 2]d. Tissue cultures were negative for bacteria, fungi and mycobacteria. Blood chemistry revealed a CD4 count of 239 cells/mm 3 with a viral load of 85,000 copies with a normal hemogram and liver enzyme levels. Given the immunosuppressed state of the patient and suggestive histopathological findings, we made a diagnosis of bacillary angiomatosis. Radiography of the finger excluded bone involvement. Abdominal ultrasound did not reveal hepatic or splenic peliosis or lymphadenopathy. The patient was treated with oral doxycycline, 100 mg twice a day. The ulcer healed completely with atrophic scarring of the nail bed and loss of nail plate after 2 months of therapy [Figure - 3].
 |
| Figure 1: Ulcer on the nail bed of the fourth left finger with loss of nail plate |
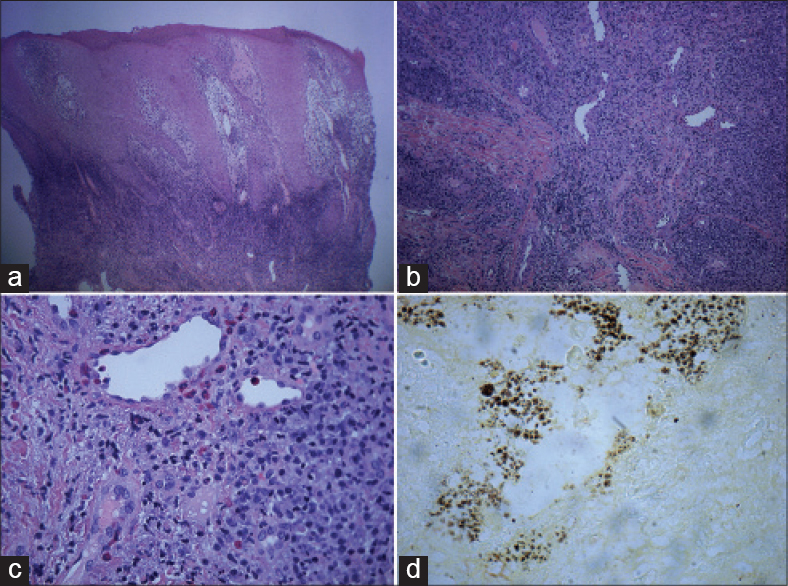 |
| Figure 2: (a) Epidermal acanthosis and a diffuse inflammatory infiltrate involving dermis with proliferation of blood vessels (H and E, 40×) (b) Lobular proliferations of small diameter blood vessels with a diffuse and a predominantly perivascular inflammatory infiltrate in deep dermis composed by neutrophils, lymphocytes, and histiocytes (H and E, 100×) (c) Detail of the vessels and the inflammatory infiltrate (hematoxilin and eosin 400×) (d) Clustered bacilli in the dermis (Warthin– Starry, 100×) |
 |
| Figure 3: Healing of the lesion after 2 months of therapy |
Bacillary angiomatosis is an uncommon infectious vasculoproliferative disorder, commonly associated with immunosuppression. Skin is the most common site of infection. [1],[3] Disease may be preceded traumatic cat contact or exposure to cat fleas. Ticks, lice and sandflies have also been implicated in the transmission of various Bartonella species. [4] In our patient, there was no history of direct contact with cats, potential exposure to ticks, lice or sandflies or history of recent travel. Clinically, bacillary angiomatosis has three distinct morphological presentations: (a) pyogenic granuloma-like (b) subcutaneous nodules and (c) hyperpigmented indurated plaques. The first type is more common and is characterized by solitary or multiple reddish, angiomatous papules and nodules affecting different areas of the skin. The face, neck, trunk, extremities and back are most commonly affected. [3] Atypical lesions have also been described including those resembling Kaposi′s sarcoma, verruga peruana or leg ulcers. [4],[5] Regional lymphadenopathy can occur and it is often painful. Disseminated disease involves the liver, spleen, lymph nodes, gastrointestinal tract, bone, brain and other organs and can occur without cutaneous lesions. [1],[5] The diagnosis is based on the demonstration of bacilli in histological sections stained with silver dyes. Culture from the biopsied tissues (which can be difficult due to the fastidious nature of the organism), electron microscopy examination, serology (which may be unreliable in immunocompromised patients due to lack of antibody response) and polymerase chain reaction are other procedures that can be used to establish the diagnosis. [4],[5]
This case is interesting due to the rarity of this condition and the extremely atypical clinical manifestation. We were unable to find any previous reports with the clinical presentation of a solitary digital ulcer. Our patient had a CD4 cell count greater than 200 cells/mm3 which is not commonly observed in bacillary angiomatosis in immunocompromised patients. Perhaps, this CD4 cell count contributed to the onset of a solitary lesion, preventing the development of a more typical disseminated disease. This case also emphasizes that bacillary angiomatosis should be considered in the differential diagnosis of skin ulceration in immunocompromised patients. The exclusion of malignancy and the recognition of Bartonella infection are important because the latter is readily treatable with antibiotic therapy.
| 1. |
Mohle-Boetani JC, Koehler JE, Berger TG, LeBoit PE, Kemper CA, Reingold AL, et al. Bacillary angiomatosis and bacillary peliosis in patients infected with human immunodeficiency virus: Clinical characteristics in a case-control study. Clin Infect Dis 1996;22:794-800.
[Google Scholar]
|
| 2. |
Stoler MH, Bonfiglio TA, Steigbigel RT, Pereira M. An atypical subcutaneous infection associated with acquired immune deficiency syndrome. Am J Clin Pathol 1983;80:714-8.
[Google Scholar]
|
| 3. |
Kayaselçuk F, Ceken I, Bircan S, Tuncer I. Baccilary angiomatosis of the scalp in a human immunodeficiency virus-negative patient. J Eur Acad Dermatol Venereol 2002;16:612-4.
[Google Scholar]
|
| 4. |
Karakas M, Baba M, Homan S, Akman A, Acar MA, Memiºoğlu HR, et al. A case of bacillary angiomatosis presenting as leg ulcers. J Eur Acad Dermatol Venereol 2003;17:65-7.
[Google Scholar]
|
| 5. |
Holmes NE, Opat S, Kelman A, Korman TM. Refractory Bartonella Quintana bacillary angiomatosis following chemotherapy for chronic lymphocytic leukaemia. J Med Microbiol 2011;60:142-6.
[Google Scholar]
|
Fulltext Views
2,513
PDF downloads
2,413





