Translate this page into:
Basal cell carcinoma, blue-white variant: Dermatoscopic findings in 32 cases
Corresponding author: Dr. Alberto Tlacuilo-Parra, Monte Olimpo 1413, Colonia Independencia, CP 44340, Guadalajara, Jalisco, Mexico. albtlacuilo@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Quiñones-Venegas R, Paniagua-Santos JE, Guevara-Gutierrez E, Esteban-Salerni G, Gonzalez-Ramirez RA, Tlacuilo-Parra A. Basal cell carcinoma, blue-white variant: Dermatoscopic findings in 32 cases. Indian J Dermatol Venereol Leprol 2021;87:29-33.
Abstract
Background:
The diagnosis of basal cell carcinoma is histopathological, but there are dermatoscopic criteria that confer high sensitivity and specificity to help the clinician improve its identification. However, the basal cell carcinoma blue-white variant does not totally meet these dermatoscopic criteria, and thus can be confused with other pigmented tumors. In the literature reviewed, we found only five cases of this variant.
Aims:
The present objective is to describe the dermatoscopic characteristics of the blue-white variant of basal cell carcinoma observed in a tertiary dermatology institute.
Methods:
The dermatoscopy files of patients with a histopathological diagnosis of basal cell carcinoma between January 1, 2006 and December 31, 2015 were reviewed.
Results:
A total of 32 cases with blue-white variant of basal cell carcinoma were observed over a period of 10 years. Of these cases, 97% presented dermatoscopic findings not included in the aforementioned criteria, such as whitish septa, structureless white areas, homogenous blue pigmentation and shiny white structures.
Limitations:
The small sample size and the retrospective nature of the design.
Conclusion:
We consider it important for dermatologists to know this rare variant of basal cell carcinoma and to familiarize themselves with their dermatoscopic findings, in order to prevent erroneous diagnoses or inadequate treatments.
Keywords
Basal cell carcinoma
dermatoscopy
diagnosis
Introduction
Skin cancer is the most frequent neoplasia in humans with 75–80% corresponding to basal cell carcinoma.1 Although histopathology is the gold standard for diagnosis,2 dermatoscopy is a tool augmenting diagnostic certainty from 60% with the “naked eye” to 90% with the use of dermatoscope.3-5
The dermatoscopic criteria for the diagnosis of basal cell carcinoma proposed by Menzies et al. include the absence of pigment network and at least one of the following: ulceration, blue-gray ovoid nests, blue-gray globules, maple leaves, spoke wheels and/or arborizing vessels.6 These criteria confer a sensitivity of 97% and specificity of 93%. Moreover, Altamura et al. proposed additional dermatoscopic findings known as “nonclassical criteria,” including concentric structures, multiple blue-gray dots, superficial short and fine telangiectasias, reddish-white shiny areas and multiple small erosions.7
In 2006, Felder et al. described two cases of nodular pigmented basal cell carcinoma that with dermatoscopy showed diffuse blue-white areas not previously described, associated with the existence of blue-gray ovoid nests, denominated “blue-white variant.”8 In 2012, Verduzco-Martinez et al. published three cases of this variant on dermatoscopy showing areas of diffuse blue color alternating with shiny-white areas.9 Like Felder et al., these authors considered that the blue-white pattern corresponded to large ovoid nests in lesions with more pigment.8
The clinical and dermatoscopic diagnosis of this basal cell carcinoma variant is not easily established with the criteria proposed by Menzies et al.,6 and even less with that of Altamura et al.,7 thereby rousing interest to describe the dermatoscopic findings of blue-white variant of basal cell carcinoma in order to enhance the characterization.
Methods
The dermatoscopy files of patients who were histopathologically diagnosed with basal cell carcinoma and who attended the Dermatology Institute of Jalisco, “Dr. José Barba Rubio,” between January 1, 2006 and December 31, 2015 were reviewed. Clinical images were obtained with a Nikon digital P5000 camera (Nikon Corporation; Tokyo, Japan) with 14 megapixels.
The dermatoscopic images were obtained with polarized light using a Dermlite DL3 dermatoscope (Dermlite Company; San Juan Capistrano, CA, USA), and evaluated using a blinded method by three dermatologist experts in dermatoscopy, to determine the frequency of the classical dermatoscopic criteria, nonclassical criteria and other dermatoscopic observations. A finding was considered positive when observed by at least two of the three dermatologists.
Results
A total of 32 cases with the blue-white variant were identified. Thirteen (41%) cases corresponded to males and 19 (59%) to females. The average age was 69.9 ± 14 years (range 42–92 years) and the average evolution time 31.5 ± 26 months (range 2–96 months). The affected areas were the face in 24 (75%) patients, hairy skin in 6 (19%) and the trunk in 2 (6%) patients. The 32 patients clinically had pigmented basal cell carcinoma.
The absence of pigment network was attained in 32 cases, although the classical diagnostic criteria were confirmed in 30 (94%) cases, and 2 (6%) had the absence of pigment network as a finding without any other dermatoscopic characteristic to orientate the diagnosis. In the remainder of cases the number of findings had the following distribution: one dermatoscopic finding in 5 (16%) cases, two findings in 10 (31%) cases, three findings in 12 (37.5%) cases and four findings in 3 (9%) cases. Ulceration was the most frequent finding in 21 (66%) cases.
The nonclassical dermatoscopic findings presented in 10 (31%) cases and multiple blue-gray dots were the most frequent finding in 8 (25%). Other dermatoscopic findings not included in the classical criteria or the nonclassical criteria were observed in 31 (97%) patients with the most frequent being homogenous blue pigmentation in 19 (59%) patients. Table 1 shows the frequency of dermatoscopic criteria observed, and Figures 1–4 show examples of the basal cell carcinoma blue-white variant.
| Criteria | n (%) |
|---|---|
| Classical criteria | |
| Absence of pigment network | 32 (100) |
| Ulceration | 21 (66) |
| Blue-gray ovoid nests | 15 (47) |
| Fine arborizing vessels | 15 (47) |
| Maple leaves | 11 (34) |
| Arborizing vessels | 8 (25) |
| Blue-gray globules | 3 (9) |
| Nonclassical criteria | |
| Multiple blue-gray dots | 8 (25) |
| Shiny reddish-white areas | 2 (6) |
| Other findings | |
| Homogenous blue pigmentation | 19 (59) |
| Whitish septa | 14 (44) |
| Structureless white areas | 11 (34) |
| Erythematous halo | 8 (25) |
| Shiny white structures | 4 (12.5) |
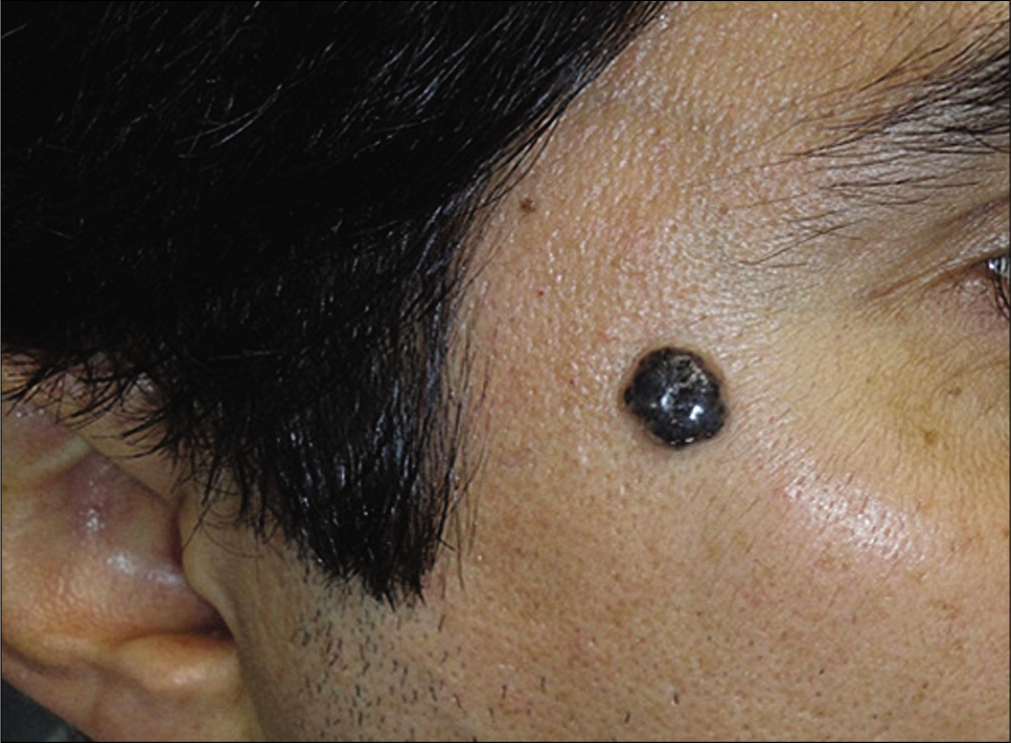
- Male, 42 years of age, with nodular lesion on the face that corresponds to an adenoid basal cell carcinoma
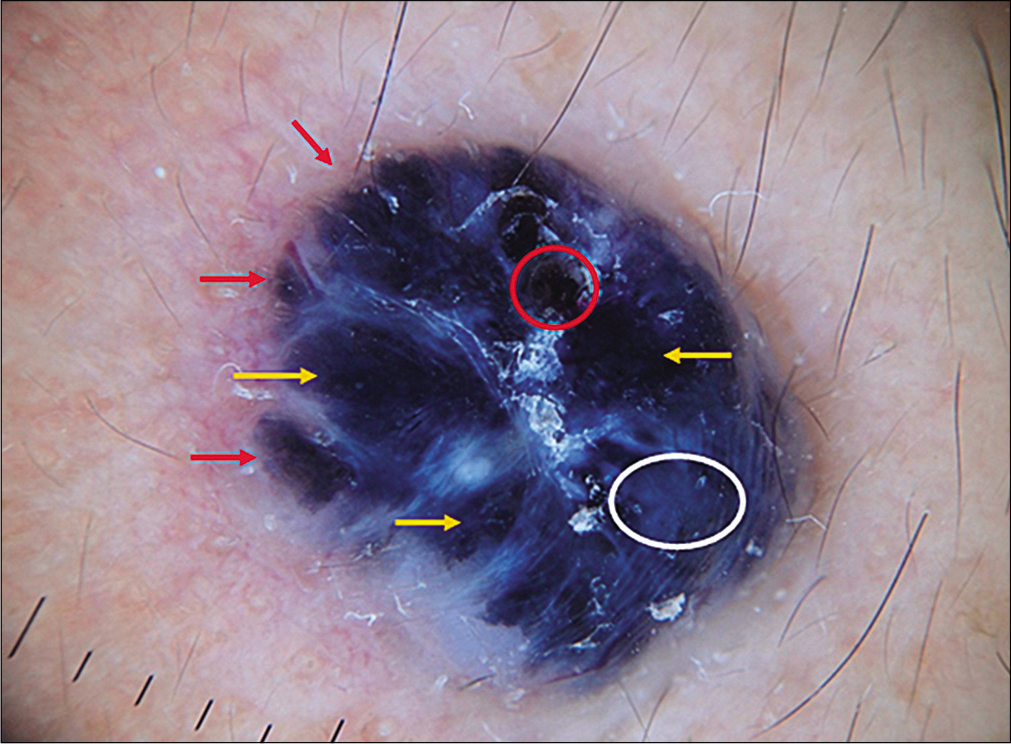
- Large ovoid nests (yellow arrows), maple leaves (red arrows), ulceration (red circle), homogenous blue area (white circle) (mode polarized light, magnification 10×).

- Female, 56 years of age, with nodular scaly lesion on the hairy skin corresponding to a superficial pigmented basal cell carcinoma
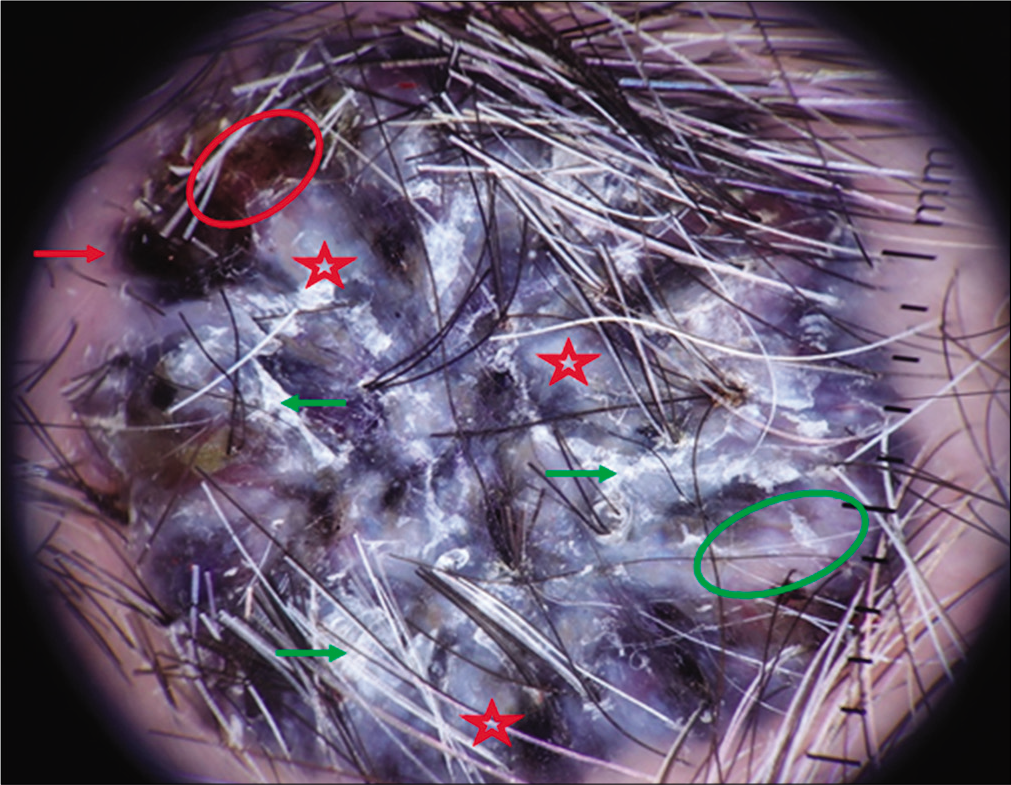
- Maple leave (red arrow), ulceration (red circle), reddish-white shiny area (green circle), structureless white areas (red stars), areas with scaling (green arrows) (mode polarized light, magnification 10×).
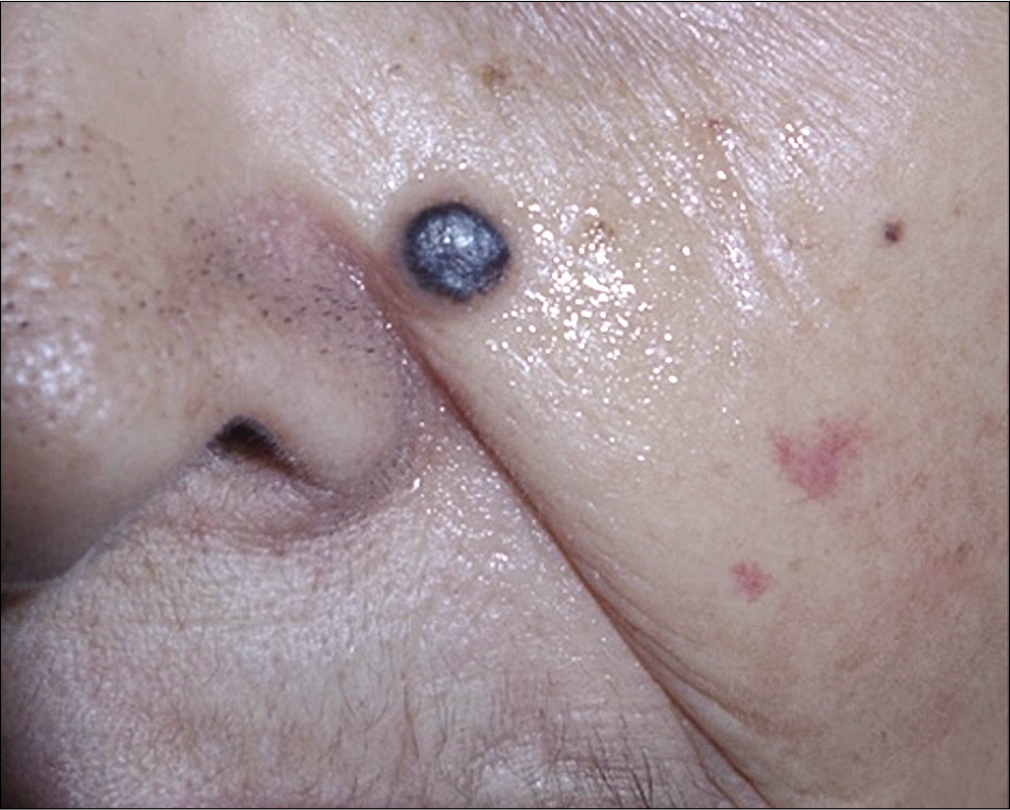
- Female, 66 years of age, with ovoid tumor that corresponds to a solid basal cell carcinoma
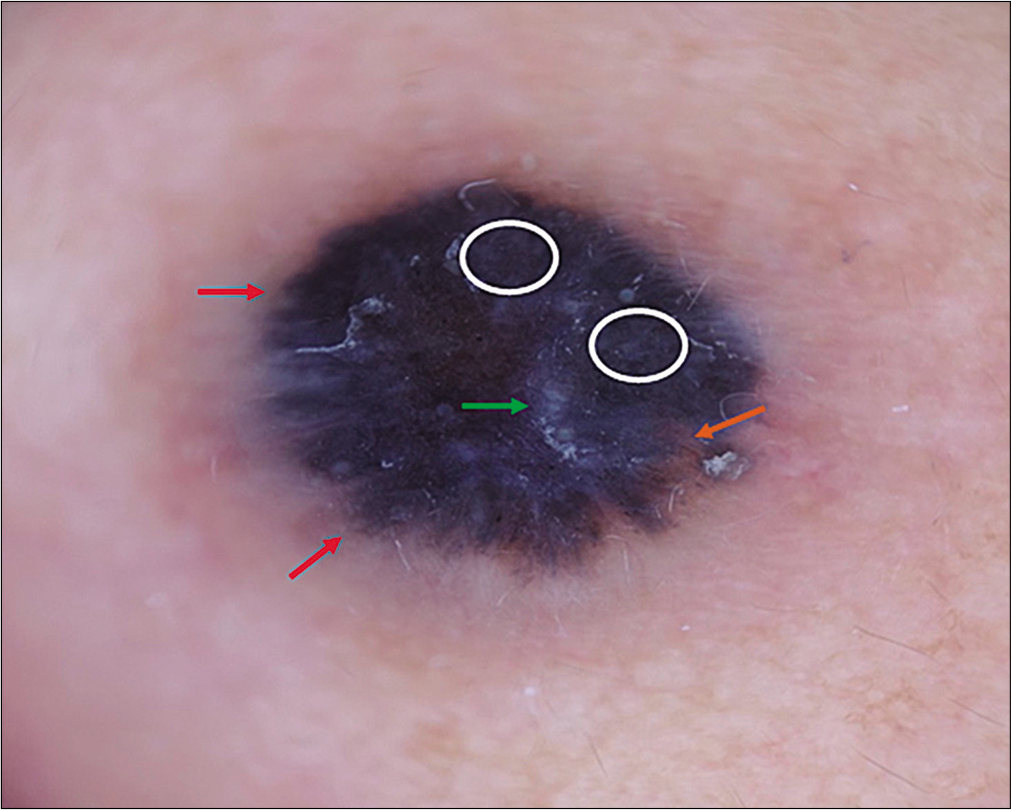
- Maple leaves (red arrows), homogenous blue area (white circle), areas with scaling (green arrow), truncated blood vessel (orange arrow) (mode polarized light, magnification 10×)

- Male, 50 years of age, with a flat tumor that corresponds to a solid pigmented basal cell carcinoma
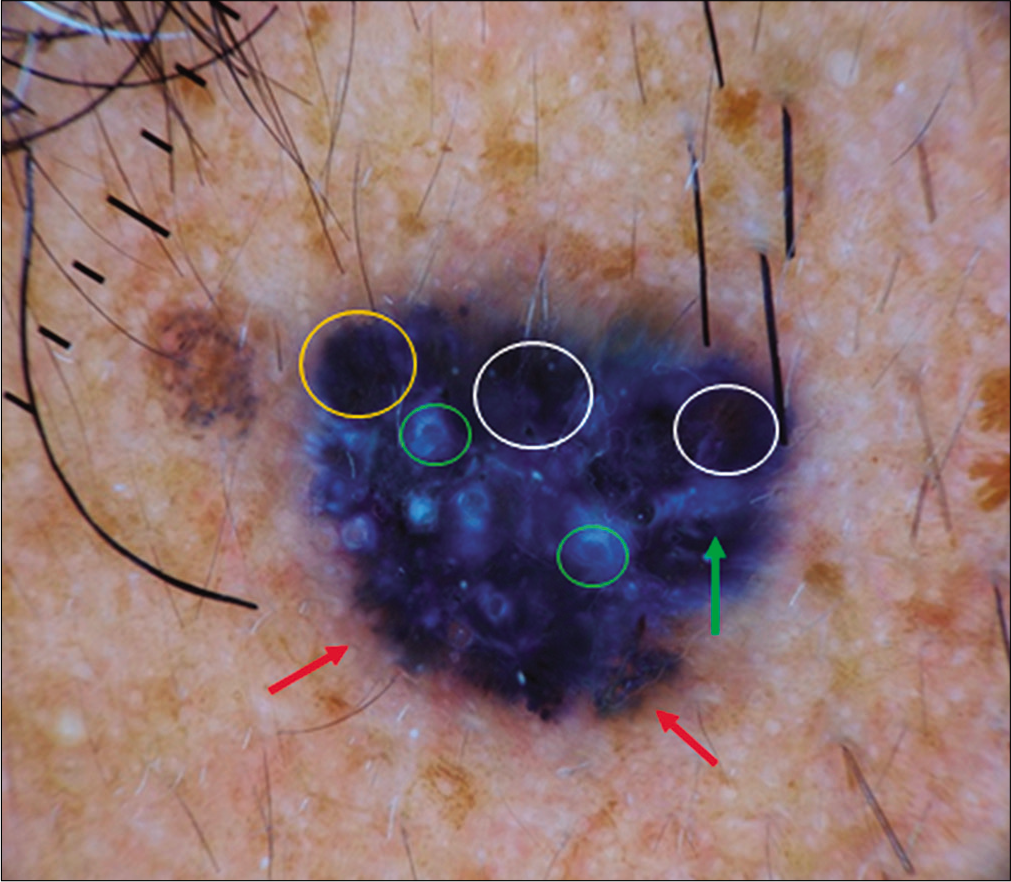
- Maple leaves (red arrow), blue ovoid nest (orange circle), homogenous blue area (white circle), shiny white structures (green arrow), white perifollicular structures (green circle) histopathologically corresponding to tumoral cells surrounding the follicle (mode polarized light, magnification 10×)
The most frequent histopathological variation was the solid-pigmented basal cell carcinoma in 15 (47%) patients, and the solid basal cell carcinoma found in 5 (16%) [Table 2].
| Histopathological variant | n (%) |
|---|---|
| Low-grade variant (n=27; 84%) | |
| Solid | 5 (16) |
| Adenoid | 4 (13) |
| Solid and pigmented | 15 (47) |
| Solid and cystic | 1 (3) |
| Superficial and pigmented | 1 (3) |
| Adenoid and pigmented | 1 (3) |
| High-grade variant (n=5; 16%) | |
| Infiltrating | 2 (6) |
| Micronodular | 1 (3) |
| Infiltrating and pigmented | 2 (6) |
Discussion
Reporting these 32 cases of blue-white variant of basal cell carcinoma is in contrast to the merely five cases previously published since its first description by Felder et al. in 2006.8 We consider this could be due to underdiagnosis because of the rarity of this variant easily confused with other pigmented lesions such as seborrheic keratosis, blue nevus or malignant melanoma; and its little diffusion in medical literature.
Previous publications mention that cases did not present all the classical dermatoscopic criteria described by Menzies et al.,6 which made their clinical-dermatoscopic diagnosis difficult.8,9 In patients reported by Verduzco-Martinez et al., one presented with maple leaves and ulceration, another with ovoid nests and ulceration and the third with only maple leaves.9 The two cases reported by Felder et al. presented only blue-gray ovoid nests and ulceration.8
In the present report, 53% of cases had only two or less of the “classical” dermatoscopic findings, which would be a more difficult diagnosis to distinguish the blue-white variant from other pigmented tumors. The most frequent classic criterion was ulceration found in 66% of cases, being a dermatoscopic characteristic also observed in four of the five cases of basal cell carcinoma blue-white variant previously published,8,9 demonstrating greater sensitivity and specificity for the diagnosis of basal cell carcinoma.10 The second most frequent findings were both fine arborizing vessels and blue-gray ovoid nests, both 47%. These latter two findings, similar to the maple leaves found in 34% of cases, were present in the two previously published cases.8,9 We found other dermatoscopic findings considered typical of basal cell carcinoma in lower percentages, such as the arborizing vessels in 25% and blue-gray globules in 9%.3-7 We did not find the typical dilated telangiectasias vessels observed in up to 57% of the conventional variants of basal cell carcinoma.3,7
Regarding the nonclassical criteria,7 they were not described in the previous cases of basal cell carcinoma blue-white variant,8,9 and presented in only 31% of our patients, including multiple blue-gray dots in 25% and shiny reddish-white areas in 6%. In 97% of cases we encountered findings not included in the aforementioned dermatoscopic criteria, the most frequent being homogenous blue pigmentation in 59% and whitish septa in 44%. These characteristics are important as we consider homogenous blue pigmentation together with blue-gray globules, multiple blue-gray dots and blue-gray ovoid nests that bestow the blue color to this dermatoscopic variant of basal cell carcinoma. It is also noteworthy that in blue-white variant of basal cell carcinoma, the type of ovoid nest is large size, to the degree of presenting a homogenous aspect. Meanwhile, the white color would be provided by whitish septa together with structureless white areas and shiny white structures.
Regarding the histopathological variations of the basal cell carcinoma blue-white variant, we found that solid basal cell carcinoma (whether single or mixed variant) corresponded to 66% of cases. Three cases reported by Verduzco-Martinez et al.9 were also solid. Felder et al.8 did not specify this data.
The main limitations of the present study are the small sample size and the retrospective nature of the design. In order to corroborate our findings, a bigger sample size as well as a correlation between the dermatoscopic findings and histology is required.
Conclusion
The importance of the basal cell carcinoma blue-white variant not only lies in establishing its rarity but also in that the dermatoscopic exploration does not present the classical criteria with the same frequency as conventional basal cell carcinoma; they can be confused with other pigmented tumors with different prognosis, such as melanoma. The dermatologist should be familiarized with the dermatoscopic findings described here in order to detect this basal cell carcinoma variant in a timely manner.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous malignancy of the head and neck. Surg Oncol Clin N Am. 2015;24:593-613.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for the management of basal cell carcinoma. Br J Dermatol. 2008;159:35-48.
- [CrossRef] [PubMed] [Google Scholar]
- The dermatoscopic universe of basal cell carcinoma. Dermatol Pract Concept. 2014;4:11-24.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of dermoscopic and histopathologic features and their correlations in pigmented basal cell carcinomas. J Eur Acad Dermatol Venereol. 2006;20:916-20.
- [CrossRef] [PubMed] [Google Scholar]
- Update on non-melanoma skin cancer and the value of dermoscopy in its diagnosis and treatment monitoring. Expert Rev Anticancer Ther. 2013;13:541-58.
- [CrossRef] [PubMed] [Google Scholar]
- Surface microscopy of pigmented basal cell carcinoma. Arch Dermatol. 2000;136:1012-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of basal cell carcinoma: Morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol. 2010;62:67-75.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic pattern of pigmented basal cell carcinoma, blue-white variant. Dermatol Surg. 2006;32:569-70.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented basal cell carcinoma with atypical dermoscopic pattern: Report of three cases with blue-white variant. Dermatol Rev Mex. 2012;56:207-9.
- [Google Scholar]
- Correlation of dermoscopic findings with histopathologic variants of basal cell carcinoma. Int J Dermatol. 2013;52:718-21.
- [CrossRef] [PubMed] [Google Scholar]






