Translate this page into:
Basal cell carcinoma in a child with xeroderma pigmentosum: Clinical response with electron beam radiation therapy
2 Department of Ocular Pathology, Dr. R.P Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Puja Sahai
Department of Radiation Oncology, Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Sahai P, Singh K, Sharma S, Kashyap S, Mohanti BK. Basal cell carcinoma in a child with xeroderma pigmentosum: Clinical response with electron beam radiation therapy. Indian J Dermatol Venereol Leprol 2013;79:533-535 |
Sir,
Xeroderma pigmentosum (XP) is a rare autosomal recessive inherited disease. It is characterized by defective nucleotide excision repair of DNA damage induced by ultraviolet (UV) rays (complementation groups A-G). Most patients with XP are not abnormally sensitive to therapeutic X-rays. We herein describe the clinical response with radiation therapy for cutaneous neoplasm in a child with XP.
A 10-year-old male child presented with cutaneous lesions on face and scalp for a duration of 1 year. He had a history of appearance of multiple hypo- and hyper-pigmented skin lesions since the age of 2 years. He also had photophobia and loss of vision in both eyes. His younger sibling did not have similar history related to XP. After evaluation in the Dermatology Clinic, a clinical diagnosis of XP was made. His physical examination showed multiple cutaneous lesions at the following sites: near right lateral canthus measuring 1.5 × 1.5 cm [Figure - 1]a, near right tragus measuring 2.5 × 1.5 cm [Figure - 1]a, near left medial canthus measuring 1.5 × 1 cm [Figure - 1]b, and on scalp measuring 3 × 3 cm [Figure - 1]c. Besides, he had multiple hypo- and hyper-pigmented macules all over his body. Ophthalmological examination showed bilateral corneal opacities. He did not have any neurological abnormality. An incisional biopsy of the scalp as well as the face lesion was performed. Histopathological examination of the biopsied specimens showed features of basal cell carcinoma (BCC) [Figure - 2]. A contrast enhanced computed tomography (CECT) of the chest and abdomen was performed to look for systemic dissemination of disease or second primary tumor. There was no abnormality detected on the imaging. The child was advised sun protection with the use of protective clothing and glasses. In addition, oral isotretinoin therapy was prescribed.
 |
| Figure 1: Clinical photograph of the patient with xeroderma pigmentosum shows basal cell carcinoma lesions: (a) nodulo-proliferative lesion near right lateral canthus and right tragus, (b) plaque-like lesion near left medial canthus, (c) ulcero-proliferative lesion on scalp; the regression of lesions after radiotherapy seen at: (d) right lateral canthus and tragus, (e) left medial canthus, (f) scalp |
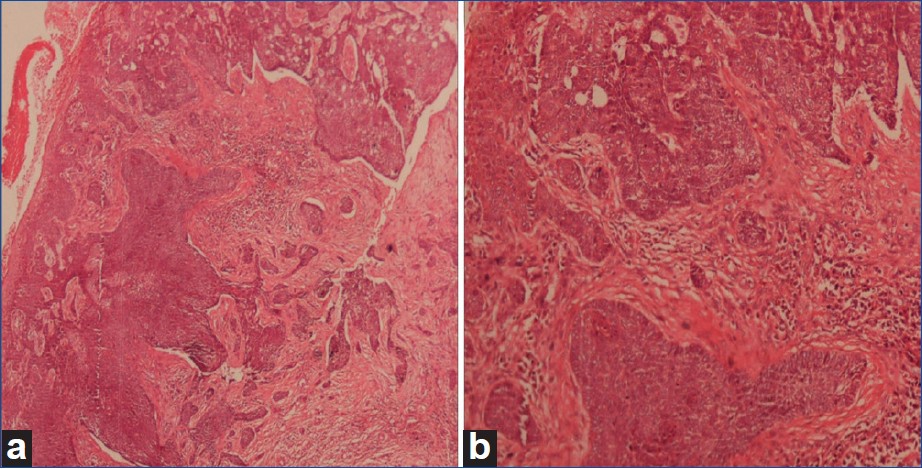 |
| Figure 2: (a) Photomicrograph shows irregular islands of basal cell carcinoma (H and E staining, × 40), (b) the section shows characteristic peripheral pallisading (H and E stain, × 200) |
Subsequently, radiotherapy was planned to treat the neoplastic lesions. The patient received 48 Gy in 16 fractions over 3.5 weeks using 8 MeV electron beam to the right-sided face lesions. He also received 36 Gy in 12 fractions over 2.5 weeks using 6 MeV electron beam for the lesion near left medial canthus. During the course of radiotherapy, grade 1 skin morbidity (follicular, faint or dull erythema/epilation/decreased sweating) [1] was observed. On review at 1 month after radiotherapy, the right-sided face lesions showed nearly 80% regression [Figure - 1]d, and the lesion near the left medial canthus showed complete resolution [Figure - 1]e. Thereafter, the scalp lesion was treated with a dose of 20 Gy in 5 fractions over a week using 10 MeV electron beam therapy. At 1 month follow-up, the scalp lesion showed complete resolution [Figure - 1]f.
The clinical features of 830 published cases of XP were reviewed by Kraemer et al. [2] Starting at the age between 1 and 2 years, these patients developed sensitivity to sunlight with appearance of freckling, atrophy, and telangiectasia. The median age for the development of first malignant neoplasm of skin was 8 years. Squamous cell carcinoma (SCC) and BCC constituted the majority of neoplasms, and 97% of those occured in the head and neck region. The life span of the patients with XP was seen reduced by approximately 30 years. The probability of surviving upto the age of 28 years was estimated at 80%.
The clinical management of XP includes avoidance of sunlight, minimizing UV exposure, early detection of skin lesions, and genetic counselling. [3] Oral 13-cis-retinoic acid has been shown to reduce the incidence of new cancers in these patients. [4] Surgical excision is the modality used for treatment of cutaneous neoplasms. However, lesions at some sites may not be amenable to adequate surgical intervention. In addition, significant aesthetic deformities may result from multiple excisions. Despite their extreme sensitivity to UV light, the patients with XP can be treated with standard doses of radiation for the treatment of neoplasms. [5] The reports of use of radiotherapy as a treatment modality for cutaneous neoplasms in patients with XP are rare. The doses and techniques for radiotherapy are not defined for these patients. Nevertheless, the schedule for radiotherapy may be individualized based on the clinical presentation and the number, type, size, and the site of the lesion. Schaffer et al., [6] described 2 patients with SCC of skin associated with XP. These patients were treated with radiotherapy. After follow-up periods of 2 and 7 years respectively, both the patients developed fewer skin cancers on the treated side of face. In addition, they did not manifest any acute or chronic complications.
Effective sun protection and early recognition of skin cancers play important roles in the management of XP. Radiation therapy is an effective therapeutic modality for the treatment of cutaneous neoplasms with XP. In view of short survival period of these patients, long-term clinical outcome and late effects of radiation therapy remain to be elucidated.
| 1. |
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341-6.
[Google Scholar]
|
| 2. |
Kraemer KH, Lee MM, Scotto J. Xeroderma pigmentosum. Cutaneous, ocular, and neurologic abnormalities in 830 published cases. Arch Dermatol 1987;123:241-50.
[Google Scholar]
|
| 3. |
Kraemer KH, DiGiovanna JJ. Xeroderma Pigmentosum. GeneReviews. Online database. Available at http://www.genetests.org. [Last accessed on 2012 May 20]
[Google Scholar]
|
| 4. |
Kraemer KH, DiGiovanna JJ, Moshell AN, Tarone RE, Peck GL. Prevention of skin cancer in xeroderma pigmentosum with the use of oral isotretinoin. N Engl J Med 1988;318:1633-7.
[Google Scholar]
|
| 5. |
DiGiovanna JJ, Patronas N, Katz D, Abangan D, Kraemer KH. Xeroderma pigmentosum: Spinal cord astrocytoma with 9-year survival after radiation and isotretinoin therapy. J Cutan Med Surg 1998;2:153-8.
[Google Scholar]
|
| 6. |
Schaffer JV, Orlow SJ. Radiation therapy for high-risk squamous cell carcinomas in patients with xeroderma pigmentosum: Report of two cases and review of the literature. Dermatology 2011;223:97-103.
[Google Scholar]
|
Fulltext Views
2,662
PDF downloads
1,123





