Translate this page into:
Basal cell nevus syndrome: A rare entity
2 Department of General Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
Correspondence Address:
Manish Bansal
Department of Dermatology and Venereology, Institute of Medical Sciences, Banaras Hindu University, Varanasi - 221005, Uttar Pradesh
India
| How to cite this article: Bansal M, Nivash S, Manchanda K, Khanna R. Basal cell nevus syndrome: A rare entity. Indian J Dermatol Venereol Leprol 2012;78:666 |
Sir,
Basal cell nevus syndrome (BCNS), also known as Gorlin syndrome is a rare autosomal dominant disorder associated with panoply of phenotypic abnormalities including developmental abnormalities and postnatal tumors, especially basal cell carcinoma. [1] It was first reported by Jarish and White (1894) and later Gorlin (1960) described the classical triad of syndrome i.e. multiple basal cell carcinomas (BCCs), keratocysts in the jaws and bifid ribs. [2] The prevalence of syndrome is estimated to be 1 in 60,000 to 1 in 120,000 persons. [1] We are hereby reporting this case because of its rarity.
Thirty-seven-year old male presented to surgery outpatient department with a raised lesion over medial canthus of left eye for 5 years which was continuously increasing in size, thus hindering vision. Excisional biopsy of lesion revealed BCC and patient was referred to dermatology department for similar lesions over trunk, face and upper extremities. There was past history of surgical correction of cleft lip in childhood. There was no history of similar illness in family. On examination, patient had scoliosis of thoraco-lumbar spine with polydactyly and syndactyly in left foot. He had facial asymmetry, coarse facies, hypertelorism and a longitudinal scar mark on left side of upper lip. On mucocutaneous examination, multiple erythematous plaques varying in size from 0.5 cm-3 cm with atrophy and elevated rolled out border were present over forehead, scalp, post auricular area, trunk and upper limbs with a total of 18 lesions [Figure - 1]a-c. Palms and soles showed multiple superficial pits [Figure - 1]d. Intraoral examination revealed absence of multiple molar and premolars teeth. Based on history and examination, provisional diagnosis of BCNS was made. Complete blood count, liver and renal function test, random blood sugar and urinalysis were normal. X-Ray chest showed ribbon-shaped, splayed and bifid ribs [Figure - 2]a. Skull radiograph showed early bridging of sella turcica, calcification of falx cerebri, and multiple bone cysts, loss of teeth and portion of mandible [Figure - 2]b. Orthopantomograph revealed multiple odontogenic cysts [Figure - 2]c. Radiograph of spine showed scoliosis of thoracolumbar spine and reduced disc space [Figure - 2]d. Histopathological examination of punch biopsy sample from lesion over forehead showed an epithelial neoplasm with tumor islands made up of small round cells which showed peripheral palisading and were restricted to papillary dermis [Figure - 3]a. Occasional pyknotic cells were scattered between these cells. Surrounding stroma showed mucin and perivascular lymphoplasmacytic infiltrate [Figure - 3]b. The diagnosis of BCNS was thus confirmed based on diagnostic criteria.
 |
| Figure 1: (a) Erythematous to hyper pigmented plaques with rolled out border over medial canthus of left eye and forehead (arrows) (b) Multiple hyper pigmented plaques over back (arrows) (c) Similar kind of lesions over upper anterior chest (arrows) (d) Multiple plantar pits alongwith syndactyly and polydactyly (arrows) |
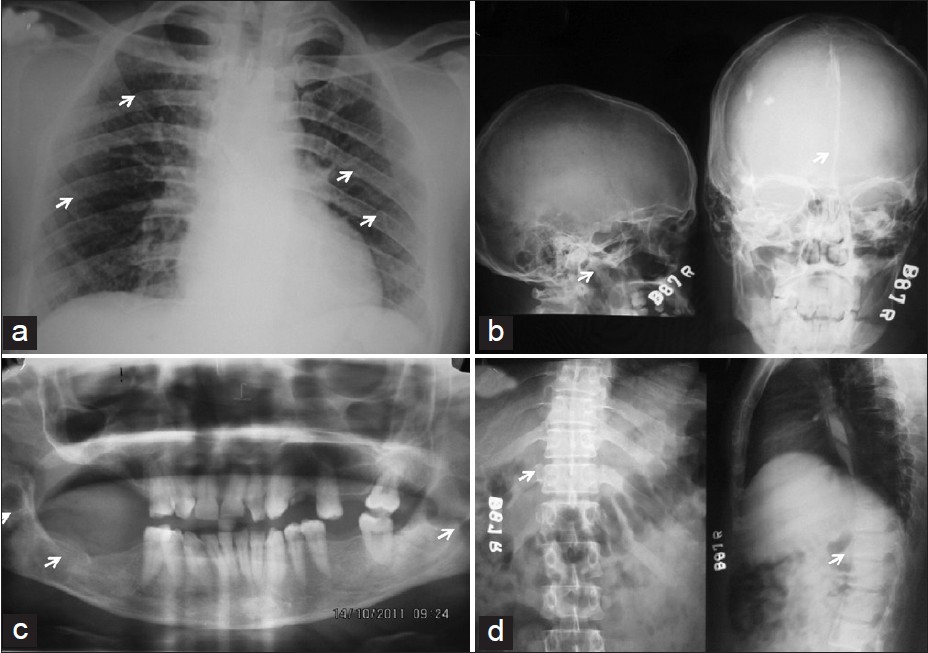 |
| Figure 2: (a) Chest radiograph showing ribbon shaped ribs (arrows) (b) Radiograph of skull showing calcification of falx cerebri and multiple bone cysts (c) Orthopantomograph showing multiple odontogenic cysts (arrows) (d) Radiograph of spine showing thoracolumbar scoliosis and bifid ribs (arrows) |
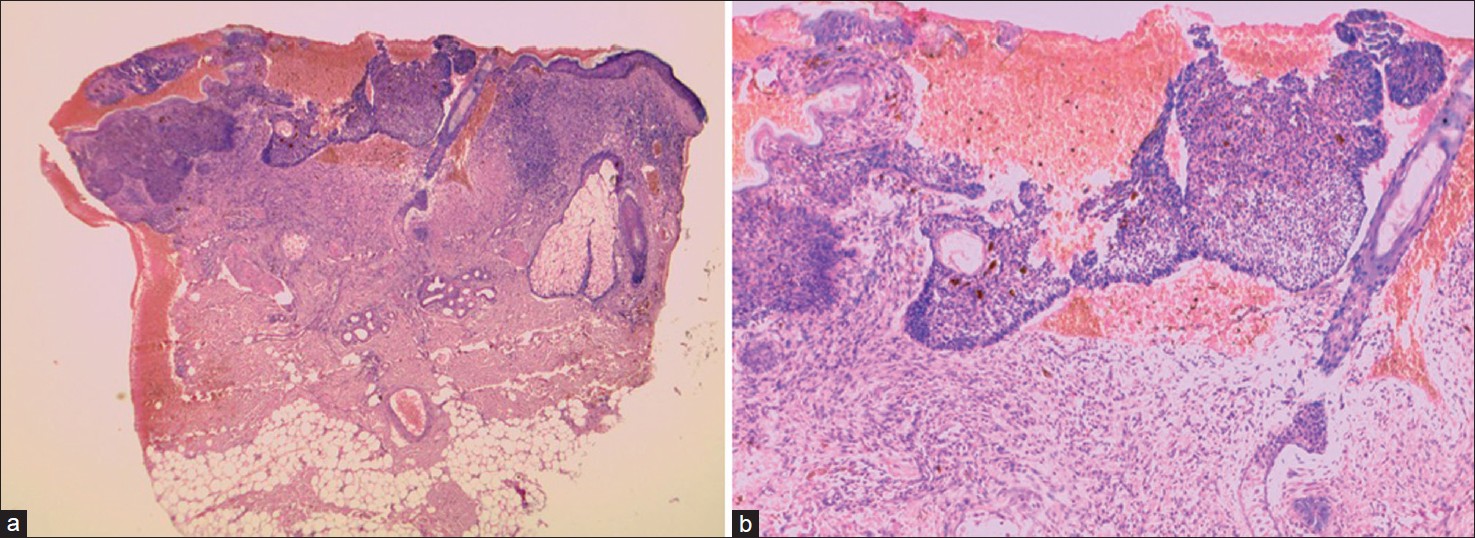 |
| Figure 3: (a) Islands of tumor cells in the epidermis (H and E, X40) (b) Neoplastic cells with dark stained pyknotic nucleus (H and E, X100) |
BCNS was delineated by Gorlin and Goltz in 1960 and has been given names as Gorlin syndrome, Gorlin-Goltz syndrome, nevoid basal cell carcinoma syndrome. [1],[2] It is a hereditary condition characterized by wide range of developmental abnormalities with predisposition to neoplasms. [3] BCNS syndrome patients carry mutation in the PTCH1 gene on 9q22.3 chromosome. [1] Main clinical manifestations include multiple BCCs, odontogenic keratocysts of the jaws, hyperkeratosis of palms and soles, skeletal abnormalities, intracranial ectopic calcifications, and facial dysmorphism (macrocephaly, cleft lip/palate and eye anomalies) with intellectual deficit in upto 5% cases. Ocular, genitourinary and cardiovascular disorders may occur. [3] The diagnostic criteria for BCNS were proposed by Evans et al. and modified by Kimoni et al. in 1997. [4] Diagnosis of Gorlin syndrome can be established when two major or one major and two minor criteria are present. Gene mutation analysis helps in confirmation of diagnosis. Genetic counseling is mandatory in every case. Antenatal diagnosis by ultrasonography and analysis of fetal cells DNA (amniocentesis or chorionic villus sampling) can be done. [3]
Management involves close surveillance and multidisciplinary approach. Surgery for BCCs is indicated when the number of lesions is limited. Other treatments include topical imiquimod 5%, laser ablation and photodynamic therapy with strict sun avoidance. [1],[3] Some authors indicated that isotretinoin at doses of 0.5-1.0 mg/kg/day cause regression of lesions less than 1.0 cm and prevent new lesions. [5] High dose oral retinoids were not found to be very useful and were associated with toxicity. [3]
Diagnosis of BCNS was confirmed as our patient met four major and three minor criteria. The patient was prescribed 5% imiquimod for cutaneous lesions and lesions showed significant improvement in erythema and induration. The patient was advised strict photoprotection along with oral isotretinoin (0.75 mg/kg/day) as chemoprevention. Issues of genetic counseling and antenatal diagnosis were discussed with patient. Family members of the patient were screened for presence of any features suggestive of BCNS. Patient was discharged on advice of regular follow up every 3 months. No new lesions appeared and previous lesions showed significant healing in 6 months follow up.
The authors thus emphasized on early diagnosis and proper management of BCNS with strict photoprotection, topical 5% imiquimod and oral isotretinoin for chemoprevention, at low dosages along with genetic counseling.
Acknowledgment
The author would like to thank the patient for providing consent to use his photograph in this article.
| 1. |
Oro EA. Basal cell nevus syndrome. In: Fitzpatrick TB, Wolff K, Goldsmith AL, Gilchrest AB, Paller SA, Leffell JD, editors. Dermtology in General Medicine. 7 th ed. New York: Mc-Graw-Hill; 2008. p. 1042-8.
[Google Scholar]
|
| 2. |
Gorlin RJ, Goltz RW. Multiple nevoid basal-cell epi-thelioma, jaw cyst and bifid rib: A syndrome. New Engl J Med 1960;5:204- 10.
[Google Scholar]
|
| 3. |
Lo Muzio L. Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet J Rare Dis 2008;3:32.
[Google Scholar]
|
| 4. |
Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet 1997;69:299-308.
[Google Scholar]
|
| 5. |
Sanchez-Conejo-Mir J, Camacho F. Nevoid basal cell carcinoma syndrome: Combined etretinate and surgical treatment. J Dermatol Surg Oncol 1989;15:868-71.
[Google Scholar]
|
Fulltext Views
4,180
PDF downloads
3,792





