Translate this page into:
BCGosis with erythema nodosum in a child with chronic granulomatous disease: An atypical presentation
Corresponding author: Dr. Bijaylaxmi Sahoo, Department of Dermatology, Maulana Azad Medical College, Bahadur Shah Zafar Marg, New Delhi, India. blsahooacad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahoo B, Monalisa K, Jhamb U, Saxena R. BCGosis with erythema nodosum in a child with chronic granulomatous disease: An atypical presentation. Indian J Dermatol Venereol Leprol. 2025;91:S74-S76. doi: 10.25259/IJDVL_384_2023
Dear Editor,
The World Health organisation (WHO) recommends Bacillus Calmette-Guérin (BCG) vaccination to all the neonates in India. However, the BCG vaccination may be associated with complications that may be subdivided into: i) local (vaccine area) or regional (adjacent lymph-node) vaccine-related complications referred to as Bacillus Calmette-Guérin (BCG)itis and ii) distant (affecting one site) or disseminated (affecting > 1 site or blood) BCG infection, referred to as Bacillus Calmette-Guérin(BCG)osis.1 The diagnosis of BCGitis or BCGosis is often delayed due to atypical manifestations in immunocompromised hosts which can lead to potentially lethal infections. Hence, early diagnosis and institution of anti-tubercular therapy (ATT) are indispensable. Herein, we report a case of coexistence of erythema nodosum with BCGosis in a 6-month-old child with underlying chronic granulomatous disease (CGD) who responded to ATT.
A 6-month-old male child, a known case of chronic granulomatous disease, presented with multiple erythematous papules distributed symmetrically over both the lower and upper limbs, buttocks and face with complete truncal sparing, for 3 days. Most of the lesions were topped with a punctum [Figures 1a–1b]. Based on the clinical morphology, a provisional diagnosis of ‘papular urticaria’ was considered. However, the lesions increased in number, size and progressed to form tender subcutaneous nodules, in a period of 2–3 days [Figures 2a–2b]. On further enquiry, it was noted that there were two episodes of inflammation at the BCG site, 2 and 6 weeks prior to the onset of these lesions. Patient was admitted in the paediatric ward and was on multiple antibiotics (inj. linezolid, meropenem, ceftazidime, vancomycin, metronidazole), antifungals (liposomal amphotericin B) and systemic steroids for fever of unknown origin, and not responding. Chest X-ray revealed multiple fibro-nodular opacities and pleural effusion in bilateral lung fields. Computed tomography (CT) chest confirmed the presence of multiple nodules in both the lungs with cavitation in one of the subpleural nodules of the right middle lobe [Figure 3]. Sputum and gastric aspirate for acid fast bacilli (AFB) were negative. Ultrasound of the left upper arm revealed a well-defined hypoechoic lesion with a few internal echoes in the intramuscular plane at the site of BCG vaccination suggestive of ‘Post BCG abscess formation’. Haematoxylin and Eosin stained sections from one of the subcutaneous nodules revealed mixed focal panniculitis with neutrophilic and lymphocytic infiltrate [Figure 4]. Acid fast bacilli and Periodic acid Schiff (PAS) stains were negative. Tissue culture and polymerase chain reaction (PCR) for Mycobacterium bovis (M.bovis) were negative. Based on the above clinical findings and histopathological examination, the final diagnosis of BCGosis with erythema nodosum in a patient with chronic granulomatous disease was considered and first line ATT was started empirically. The fever subsided and lesions of erythema nodosum healed with residual hyperpigmentation after 4-weeks of starting ATT [Figure 5]. In addition, there was resolution of the BCG site abscess.

- Multiple erythematous shiny papules (black circle) symmetrically present over bilateral lower limbs.

- An excoriated erythematous papule (black circle) over cheek with overlying punctum.

- Multiple well-defined tender subcutaneous nodules over bilateral thighs and legs.

- Multiple well-defined tender subcutaneous nodules over bilateral lower legs.

- Axial non-contrast computed tomography (NCCT) chest image of lower segment of right lobe showing subpleural cavitation.
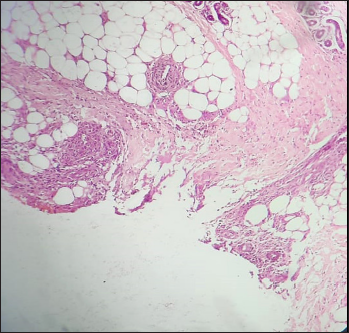
- Photomicrograph under (Haematoxylin and eosin, 40x) magnification showing lobular and septal panniculitis.

- Day 15 of antitubercular therapy (ATT): Significant improvement in the erythema and oedema of the lesions in the lower limbs.
BCGosis is a rare complication of BCG vaccination, observed in patients with underlying primary immunodeficiency disease. The European Society for Immunodeficiency (ESID), 2019, has categorised and defined the diagnostic criteria for BCGosis [Table 1]. Ong et al. observed skin and lungs involvement in 60% and 30% cases of BCGosis, respectively.2 Cutaneous involvement presents as erythema, oedema, pustulation or abscess formation at the BCG injection site 3 or as disseminated lesions as cutaneous infection, maculopapular rash or regional lymphadenitis.2 Pulmonary involvement may present as pneumonic infiltrates and lymphadenopathy in children4 or miliary tuberculosis and diffuse alveolar damage in adults.5 The innate immunity, especially T-cell immunity, interleukin-12/interferon-gamma axis and phagocytic oxidative burst activity, are essential in protecting the immune system against mycobacterial infections.6 Since the above pathway is defective in chronic granulomatous disease patients, they are more predisposed to severe mycobacterial infections.
| Diagnostic criteria for BCGosis: | |
|---|---|
|
|
| BCGosis types | Criteria |
| Definitive | 1, 2, 3 |
| Probable | 1, 2(a), 3 |
| Possible | 1, 3 |
BCG: Bacille calmette-guerin, PCR: Polymerase chain reaction
The present case of chronic granulomatous disease was at a high risk of developing BCG-related complications. The patient developed pain and inflammation at the BCG site followed by disseminated skin and lung infection. Though the diagnosis of BCGosis was considered on a very high index of clinical suspicion, it was only confirmed when the patient responded dramatically to ATT. However, such an atypical progression from papular urticaria like presentation to erythema nodosum within a short span of 2 days is unique in the present scenario. Furthermore, erythema nodosum being a type of id reaction has not been previously noted with BCGosis.
Owing to the low sensitivity (8–11%) of mycobacterial culture in detecting skin tuberculosis7 and high mortality rate (50–80%) in BCGosis,2 we recommend that in patients with underlying primary immunodeficiency diseases, the diagnostic criteria for BCGosis be modified and response to ATT should be added to the existing criteria.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Bacillus calmette-guerin (BCG) vaccine-associated complications in immunodeficient patients following stem cell transplantation. J Clin Immunol. 2021;41:147-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Disseminated bacillus-calmette-guérin infections and primary immunodeficiency disorders in Singapore: A single centre 15-year retrospective review. Int J Infect Dis. 2020;97
- [CrossRef] [PubMed] [Google Scholar]
- Local cutaneous complications after bacille calmette-guerin vaccine: Experience of a single center. Int J Clin Pediatr. 2018;6:37-41.
- [Google Scholar]
- Disseminated bacille calmette-guérin infection at a glance: A mini review of the literature. Adv Respir Med. 2019;87:239-42.
- [CrossRef] [PubMed] [Google Scholar]
- Differential diagnosis of primary immunodeficiency in patients with BCGitis and BCGosis: A single-centre study. Scand J Immunol.. 2021;94:e13084.
- [CrossRef] [PubMed] [Google Scholar]
- Primary immunodeficiency diseases and bacillus calmette-guérin (BCG)-vaccine-derived complications: A systematic review. J Allergy Clin Immunol Pract. 2020;8:1371-86.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous tuberculosis in children and adolescents: A clinicohistological study. J Eur Acad Dermatol Venereol JEADV.. 2007;21:40-47.
- [CrossRef] [PubMed] [Google Scholar]






