Translate this page into:
Bilateral “turkey ear” as a cutaneous manifestation of lupus vulgaris
2 Department of Pathology, The First Affiliated Hospital of China Medical University, Shenyang, China
Correspondence Address:
Hua Zheng
Department of Dermatology, The First Bethune Hospital of Jilin University, Changchun 130000
China
| How to cite this article: Lu Y, Wang H, Zheng H, Li X. Bilateral “turkey ear” as a cutaneous manifestation of lupus vulgaris. Indian J Dermatol Venereol Leprol 2018;84:687-689 |
Abstract
Lupus vulgaris is a common form of cutaneous tuberculosis in China, mostly involving the head and neck region. Turkey ear is a clinically descriptive term, used for a massively enlarged earlobe with bluish-red or violaceous indurated plaques and nodules, which can be a sign of lupus vulgaris. A 47-year-old female presented with edema and reddish ulcerated lesions on both ears which was diagnosed as lupus vulgaris by conventional laboratory investigations and the patient showed good response to antituberculous therapy. Occurrence of turkey ears in lupus pernio (sarcoidosis) should also be mentioned here as this presentation was originally described in this condition. Two case reports of turkey ear have been reported with cutaneous tuberculosis (not bilateral). However, occurrence of bilateral turkey ears in cutaneous tuberculosis has not been described so far in the literature.
Introduction
The most common presentation of tuberculosis is with lung involvement; however, cutaneous tuberculosis is not very uncommon and accounts for 1.5% of extrapulmonary tuberculosis.[1] Lupus vulgaris, the most common clinical variant of cutaneous tuberculosis, is mostly reported on the head and neck region. It has the potential of autoinoculation and can spread to other areas of the body. Clinically, lupus vulgaris is characterized by soft reddish-brown plaques with an 'apple jelly nodule' appearance on diascopy, in addition to healing and scarring in one area and active disease in another area. This has the clinical appearance of bilateral “turkey ears,” as previously described in lupus pernio.
Case Report
A 47-year-old female presented with painful ulcers on bilateral pinnae, which were rapidly progressing since 7 months. Symptoms began with an alleged history of mosquito bite over the right earlobe. On examination, both pinnae appeared edematous and ulcerated, coated with foul-smelling purulent discharge on the surface. The outer helix and posterior surface of the pinnae were studded with cracked micropustules, which extended to the cheek and the retroauricular area. Thin adherent crusts were visible in most areas with maceration of the retroauricular fold [Figure - 1]. The right ear was affected more severely. There were no associated constitutional symptoms, history of previous trauma, Bacille Calmette-Guérin (BCG) vaccination or medical history suggestive of systemic tuberculosis. There was no lymphadenopathy. The rest of the systemic examination was within normal limits. Computed tomography of the chest, ultrasonography of the abdomen and hematological investigations were unremarkable except for an elevated erythrocyte sedimentation rate. Serology for HIV was non reactive. Intradermal inoculation of purified protein derivative showed an induration of 18 mm. A punch biopsy from the lesion revealed normal epidermis and numerous epithelioid granulomas containing a few multinucleated giant cells throughout the dermis, accompanied by a dense lymphoid infiltrate. No central necrosis was seen [Figure - 2] and [Figure - 3]. Examination with periodic acid-shiff and Ziehl-Neelsen staining failed to reveal any organisms. Tissue culture for Mycobacterium tuberculosis revealed no growth but polymerase chain reaction (PCR) for mycobacterial complex DNA was positive. The patient was diagnosed with lupus vulgaris and was treated with isoniazid 300 mg daily, rifampicin 450 mg daily, ethambutol 750 mg daily and pyrazinamide 1500 mg daily. One month later, there was significant resolution of the lesions, both clinically and histopathologically [Figure - 4] and [Figure - 5].
 |
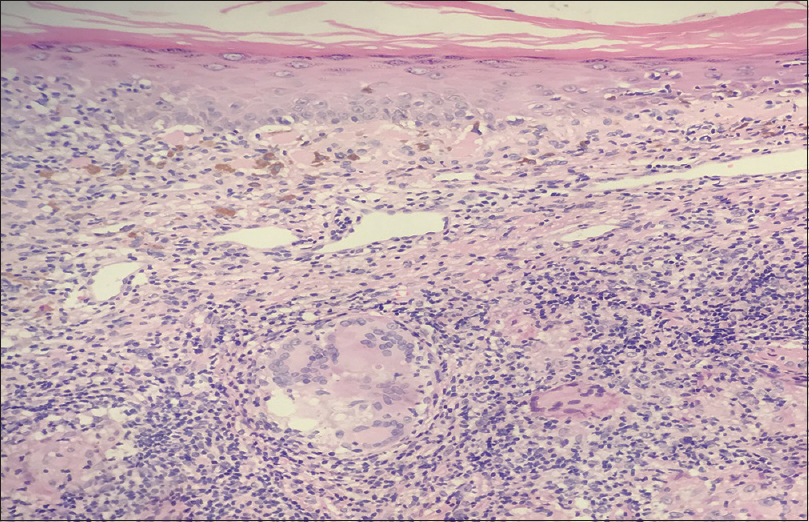 |
| Figure 2: Nonnecrotizing granulomas in the dermis and the presence of Langhans giant cells (H and E, ×200) |
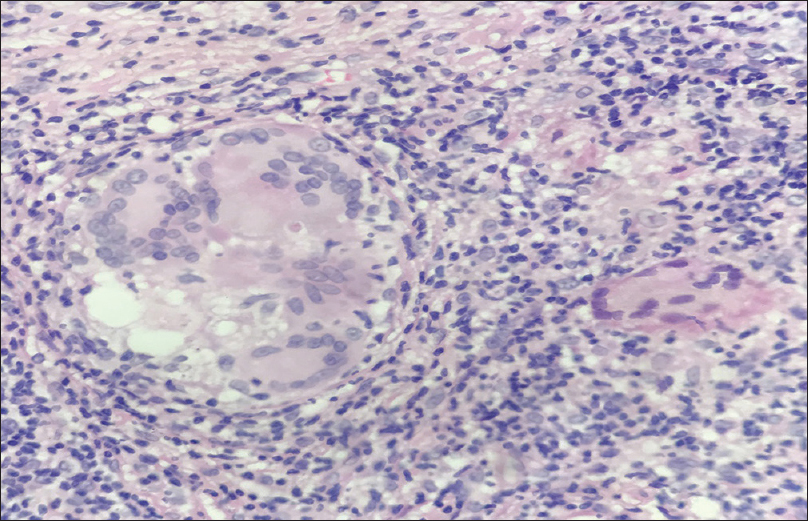 |
| Figure 3: The presence of Langhans giant cells (H and E, ×400) |
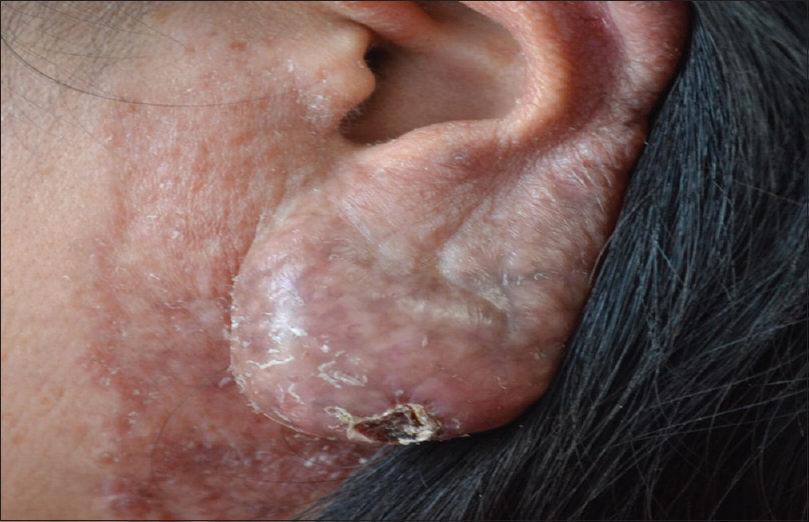 |
| Figure 4: Resolution of the ulcer after 1 month of antituberculous treatment |
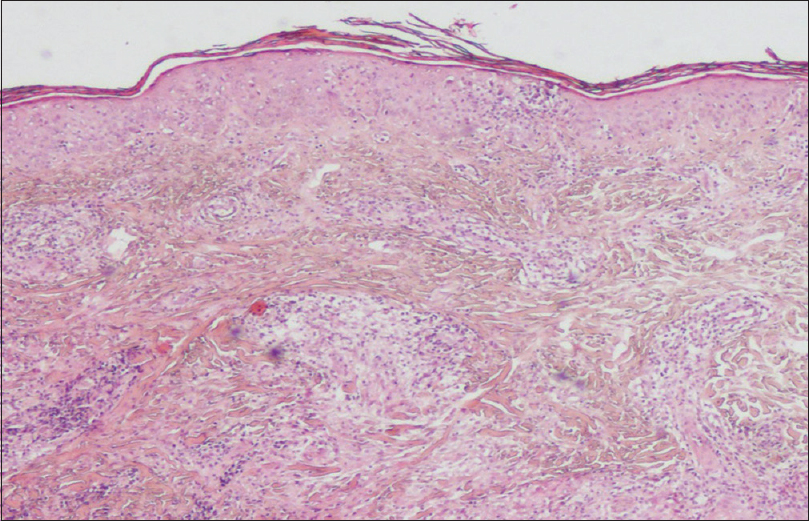 |
| Figure 5: Resolution of histological features after 1 month of antituberculous treatment (H and E, ×100) |
Discussion
Turkey ear is a descriptive term previously used specifically with regard to lupus pernio. Involved ears may become massive in lupus pernio, hence it is named “turkey ear.” Williams et al. reported a case of lupus vulgaris that had the turkey ear appearance and suggested that turkey ear could be thought of as a clinically descriptive term.[2]
Lupus vulgaris is the most common morphological variant of cutaneous tuberculosis with an average prevalence of 0.4% among dermatology patients. It is usually reinfection tuberculosis of the skin, which originates from tubercular focus elsewhere in the body, spreading by hematogenous route, lymphatics, or in a contiguous way.[1],[3] It rarely occurs after exogenous inoculation which is reported after tattoo inoculation, piercing sites, BCG vaccination, surgical wounds or injections, minor abrasions, and bindi use.[4],[5],[6],[7] However, the exact manner in which lupus vulgaris develops is difficult to assess in many cases. No endogenous source for tuberculosis was found, therefore, in the current case, we concluded that the insect bite over the right earlobe was the cause of primary inoculation.
The characteristic clinical presentation of lupus vulgaris is as a macule or a papule, with a brownish-red color and soft consistency that enlarges peripherally and forms larger plaques.[8] Ulceration and scarring may rarely occur.[2]
Diagnosing lupus vulgaris may be a formidable task. This is typically a paucibacillary form of cutaneous tuberculosis, which often makes successful culture difficult. Detection of mycobacterial DNA using PCR has been reported and may be useful where small numbers of mycobacteria are present.[9] Although it is well known that mycobacterial culture is the gold standard for diagnosis, a positive PCR helps to avoid the delay in starting presumptive antituberculous treatment in a patient with typical progressive and destructive lesions, especially when supporting features such as a reactive tuberculin skin test and classic histopathological features are present.
Case reports of lupus vulgaris regarding infection on the face indicate that the cheeks and the nose are the most frequently affected areas; primary involvement of the earlobe is extremely rare.[1] In the “myxomatous” form, huge soft tumors occur predominantly on the ear lobes, which become grossly enlarged.[2] Many conditions mimic lupus vulgaris of the ears, which include sarcoidosis (lupus pernio), tuberculoid leprosy, deep fungal infections, and chilblains. This case is unusual for the involvement of bilateral ears and the occurrence in a woman with no past history or family history of tuberculosis.
The case is worth reporting due to the presentation as “turkey ears” with obvious ulcers at the symmetric sites of earlobes, rapid progression and improvement following treatment. Awareness regarding varied clinical presentations, especially at rarer sites, is necessary as early diagnosis and treatment are keys to reduce the morbidity of the disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kaimal S, Aithal V, Kumaran MS, Abraham A. Cutaneous tuberculosis of the pinna: A report of two cases. Int J Dermatol 2013;52:714-7.
[Google Scholar]
|
| 2. |
Williams C, Mitra A, Walton S. 'Turkey ear': A diagnosis or a physical sign? Br J Dermatol 2007;157:816-8.
[Google Scholar]
|
| 3. |
Küçükünal A, Ekmekçi TR, Sakiz D. “Turkey ear” as a cutaneous maniestation of tuberculosis. Indian J Dermatol 2012;57:504.
[Google Scholar]
|
| 4. |
Dhawan AK, Pandhi D, Wadhwa N, Singal A. Tattoo inoculation lupus vulgaris in two brothers. Indian J Dermatol Venereol Leprol 2015;81:516-8.
[Google Scholar]
|
| 5. |
Kumar P, Mondal A, Lal NR, Gharami RC. Lupus vulgaris in a child: A complication of ear piercing. Indian J Dermatol Venereol Leprol 2014;80:97.
[Google Scholar]
|
| 6. |
Pace Spadaro E, Xuereb Dingli J, Doffinger R, Dinakantha K, Betts A, Pace D. BCG induced lupus vulgaris: An unexpected adverse event. Arch Dis Child 2017. pii: Archdischild-2016-312338.
[Google Scholar]
|
| 7. |
Mishra G, Rathi S, Mulani J. Bindi tuberculosis – Lupus vulgaris associated with bindi use: A case report. J Clin Diagn Res 2015;9:OD04-5.
[Google Scholar]
|
| 8. |
Yaldiz M, Erdem T, Dikicier BS, Dilek FH. Lupus vulgaris mimicking hemangioma diagnosed 42 years after onset: A case report. J Med Case Rep 2015;9:215.
[Google Scholar]
|
| 9. |
Kanada KN, Schwartz BS, Pincus LB, Berger TG, Jacobs RA, Shinkai K. A therapeutic trial of antituberculous therapy for suspected lupus vulgaris: How long does it take to see clinical improvement? J Am Acad Dermatol 2013;69:e252-4.
[Google Scholar]
|
Fulltext Views
5,827
PDF downloads
2,263





