Translate this page into:
Blaschkoid mastocytosis
Correspondence Address:
Sharad Mehta
8A, Tulsinagar, near Sai baba temple, Hiranmagri, sector 5, Udaipur - 313 001, Rajasthan
India
| How to cite this article: Mehta S, Masatkar V, Khare AK, Mittal A, Gupta LK. Blaschkoid mastocytosis. Indian J Dermatol Venereol Leprol 2015;81:72-73 |
Mastocytosis is a heterogeneous group of hematopoietic disorders, characterized by an abnormal increase and accumulation of mast cells in one or more organ systems. It is classified into two broad categories: Cutaneous mastocytosis (CM) and systemic mastocytosis (SM). [1] The course of mastocytosis is variable and is dependent on the subtype and age of onset. [2]
We report the case of a 12-year-old boy who presented to us with multiple, asymptomatic erythematous to skin-colored lesions over the left half of trunk and left upper extremity for six months. There was no history of flushing, nausea, vomiting, diarrhea, palpitations, hypotension, headache, syncope, dyspnea, wheezing, bone pain, or weight loss. There was no history of atopic dermatitis, allergic rhinitis, asthma, or food intolerance in the patient or his family members.
On physical examination, multiple well demarcated, edematous, erythematous to skin-colored papules, plaques, and nodules of size ranging from 0.5 × 0.5 to 2 × 3 cm, were present over the left half of trunk and left upper extremity along the Blaschko′s lines [Figure - 1]. Darier′s sign was negative.
 |
| Figure 1: Multiple well demarcated, edematous, erythematous to skin colored papules, plaques and nodules along Blaschko's lines |
The differential diagnoses of mucinosis, nodular histiocytosis, xanthogranuloma, cutaneous T cell lymphoma, mastocytosis, tumid lupus erythematosus, sarcoidosis, and lymphocytoma cutis were considered.Routine laboratory investigations including complete blood count, liver and renal function tests, blood sugar, urine microscopy, and electrolytes were normal. Ultrasonography (USG) of the abdomen was normal. Biopsy of a characteristic lesion showed a moderately dense perivascular infiltrate of lymphocytes, eosinophils, and mast cells in the superficial and mid-dermis. Numerous mast cells and extracellular mast cell granules were scattered in the interstitium of reticular dermis [Figure - 2]. Giemsa staining showed the presence of metachromatic granules in the cells which was confirmatory of mastocytosis [Figure - 3].
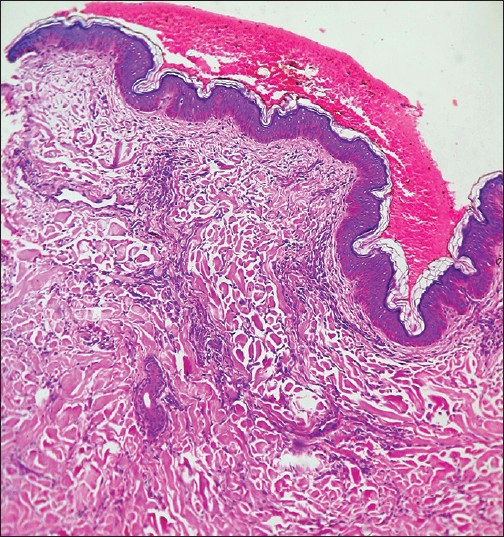 |
| Figure 2: Histopathology (H and E, ×10) showing dense superficial and mid-dermal perivascular infiltrate of lymphocytes, mast cells and eosinophils with extracellular mast cell granules, scattered in the interstitium of reticular dermis |
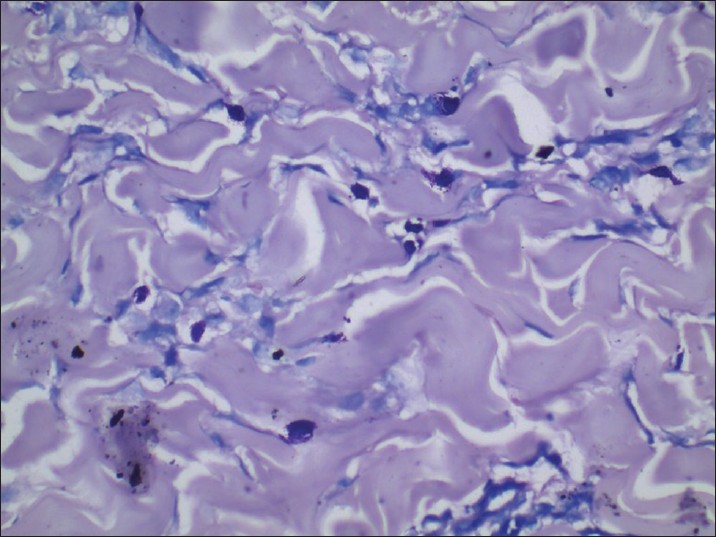 |
| Figure 3: Giemsa staining (×40) showing the presence of metachromatic granules |
Bone marrow biopsy and serum tryptase levels were not performed considering the asymptomatic nature, localized involvement, and fair prognosis in children.
The various categories of mastocytosis are urticaria pigmentosa, mastocytoma, diffuse cutaneous mastocytosis, and telangiectasia macularis eruptiva perstans, in the order of occurrence.
Mastocytosis can occur at any age. Patient usually presents with localized or generalized pruritus but it can be asymptomatic, as in our case. Darier′s sign is strongly suggestive of mastocytosis, but may be absent, as in our case.
The lines of Blaschko represent a form of "mosaicism." Many nevoid and acquired skin conditions may follow these lines including incontinentia pigmenti, focal dermal hypoplasia, epidermal nevus, sebaceous nevus, lichen nitidus, lichen planus, lichen striatus, lupus erythematosus, vitiligo, and psoriasis. [3] However, blaschkoid pattern of mastocytosis has not been described in literature though various other atypical and infrequent presentations of mastocytosis have been reported, including bullous, pseudoxanthomatous, anetoderma, and giant inguinal and suprapubic masses. [4]
Medical treatment of cutaneous mastocytosis is only symptomatic, including antihistamines, mast cell stabilizers, and avoidance of trigger factors. [5]
The diagnosis of mastocytosis is easily missed and often delayed until years after onset, sometimes resulting in a disastrous outcome.
We report this case for its unusual morphology and unique blaschkoid pattern, asymptomatic nature, and absence of Darier′s sign. Mastocytosis was not our first clinical impression, but histopathology and special stains showed the characteristic features.
| 1. |
Tharp M. Mastocytosis. In: Bolognia JL, Jorrizo J, Schaffer JV, editors. Dermatology. 3 rd ed. Philadelphia: Elsevier; 2003. p. 1993-2002.
[Google Scholar]
|
| 2. |
Middelkamp Hup MA, Heide R, Tank B, Mulder PG, Oranje AP. Comparison of mastocytosis with onset in children and adults. J Eur Acad Dermatol Venereol 2002;16:115-20.
[Google Scholar]
|
| 3. |
Ghorpade AK. Naevoid blaschkoid psoriasis. Indian J Dermatol Venereol Leprol 2010;76:449.
[Google Scholar]
|
| 4. |
Del Pozo J, Pimentel MT, Paradela S, Almagro M, Martínez W, Fonseca E. Anetodermic mastocytosis: Response to PUVA therapy. J Dermatolog Treat 2007;18:184-7.
[Google Scholar]
|
| 5. |
Kiszewski AE, Duran-Mckinster C, Orozco-Covarrubias L, Gutiérrez-Castrellón P, Ruiz-Maldonado R. Cutaneous mastocytosis in children: A clinical analysis of 71 cases. J Eur Acad Dermatol Venereol 2004;18:285-90.
[Google Scholar]
|
Fulltext Views
3,319
PDF downloads
2,710





