Translate this page into:
Blastic plasmacytoid dendritic cell neoplasm misdiagnosed and treated as acute febrile neutrophilic dermatosis
Corresponding author: Dr. Lin Gong, Department of Dermatology, The First Affiliated Hospital of Dalian Medical University, Liaoning Province, Dalian, China. drglin@163.com
-
Received: ,
Accepted: ,
How to cite this article: Song Y, Dong Y, Gong L. Blastic plasmacytoid dendritic cell neoplasm misdiagnosed and treated as acute febrile neutrophilic dermatosis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_413_2024
Dear Editor,
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is an aggressive haematological malignancy that typically manifests as skin lesions and cytopenia. Skin lesions in BPDCN appear as red or purple plaques or nodules. The bone marrow, lymph nodes, or visceral organs may be involved as well. Here, we present a case of BPDCN with lymph node and bone marrow involvement mimicking infiltrated erythematous plaques.
A 69-year-old woman had a 2-month-history of erythematous infiltration with pruritus on her face and legs and multiple reddish nodules with mild tenderness on the trunk and limbs [Figures 1a and 1b], accompanied by fever and joint pain. Laboratory results taken from another institution over a month ago revealed nearly normal complete blood counts. She was diagnosed with acute febrile neutrophilic dermatosis and treated with glucocorticoids for one month. Some skin lesions and fever disappeared after treatment but relapsed after a week of discontinuation. A repeat workup at our institution showed laboratory values of complete blood count, indicating cytopenia (white blood cells 1.89 × 109/L ↓, platelet 74 × 109/L ↓, red blood cells 3.10 × 1012/L ↓, hemoglobin 87 g/L ↓). Enlarged axillary lymph nodes were observed on the computed tomography scan. The bone marrow blood smear results were indicative of partial differentiation of acute myeloid leukaemia (M2 type) with dyserythropoiesis and dysgranulopoiesis. Flow cytometry of the bone marrow identified blasts that were positive for CD34, CD123, Human leukocyte antigen (locus) DR (HLA-DR), nTDT, CD303, and CD304; partially positive for TCL-1, CD2, CD4, CD13, CD33, CD36, CD38, CD117, CD141, and CD1c; and negative for cCD3, CD7, CD8, CD14, CD19, CD20, CD56, CD64, and anti-myeloperoxidase (MPO) [Figure 2]. This result was consistent with acute myeloid leukaemia (partial differentiation into plasmacytoid dendritic cells). The final diagnosis was made using skin biopsy and immunohistochemistry. Skin biopsy revealed a clear grenz zone between the epidermis and dermis [Figure 3a]. Extensive infiltration of neoplastic cells with nuclear atypia and immature nuclear chromatin patterns with occasional nucleoli were observed throughout the dermis [Figure 3b]. Immunohistochemistry was positive for CD38 [Figure 3c], CD123 [Figure 3d] and CD56 [Figure 3e]. Immunohistochemistry was negative for CD34 [Figure 3f] and MPO [Figure 3g]. According to the immunophenotypic diagnostic criteria proposed by the World Health Organisation, the patient was diagnosed with BPDCN.1 The patient refused the recommended therapeutic plan and is still under follow-up.

- (a) Infiltrated erythematous plaques on face and legs, and multiple erythematous nodules on trunk and limbs. (b) Multiple erythematous nodules and infiltrated erythematous plaques on trunk and limbs.
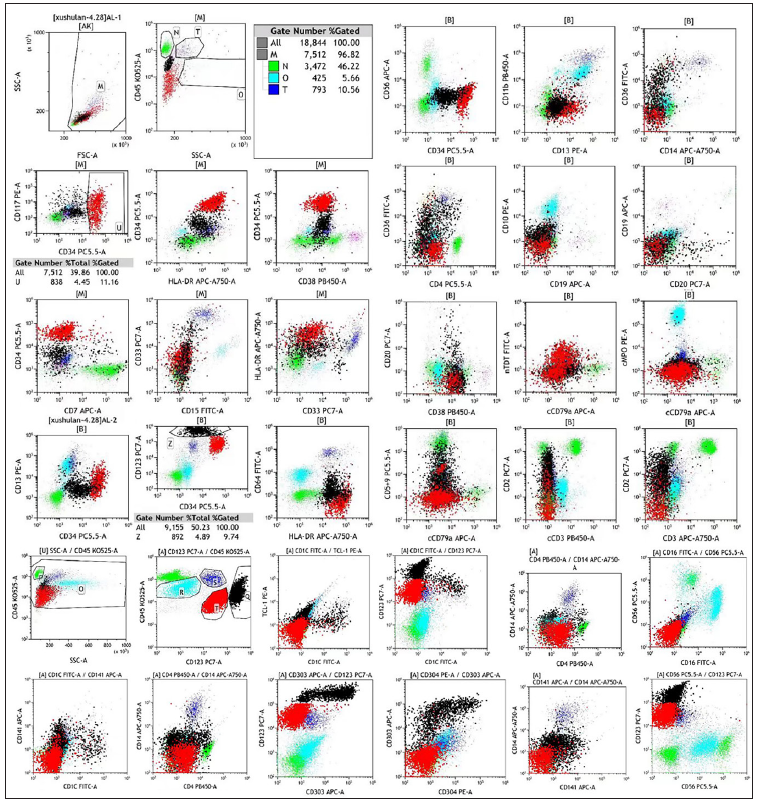
- Flow cytometry of bone marrow identified CD34+, CD123+, Human leukocyte antigen (locus) DR+, nTDT+, CD303+, CD304+blasts.
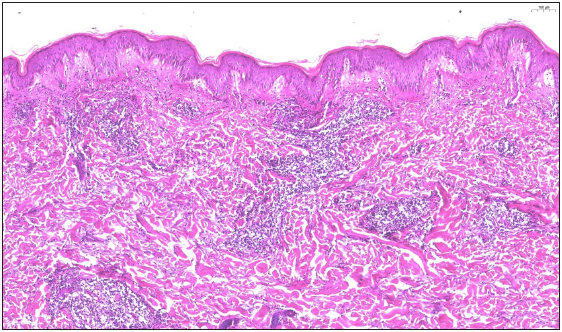
- A clear grenz zone between epidermis and dermis (Haematoxylin and eosin, 100x).
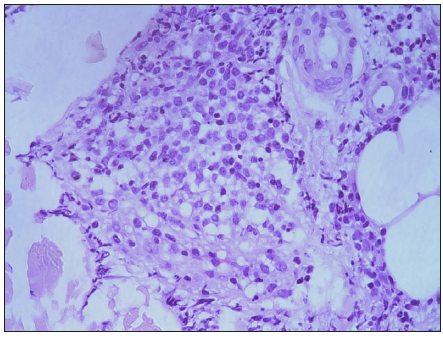
- The extensive infiltration of neoplastic cells which demonstrated nuclear atypia and immature nuclear chromatin pattern with occasional nucleoli in the entire dermis (Haematoxylin and eosin, 400x).
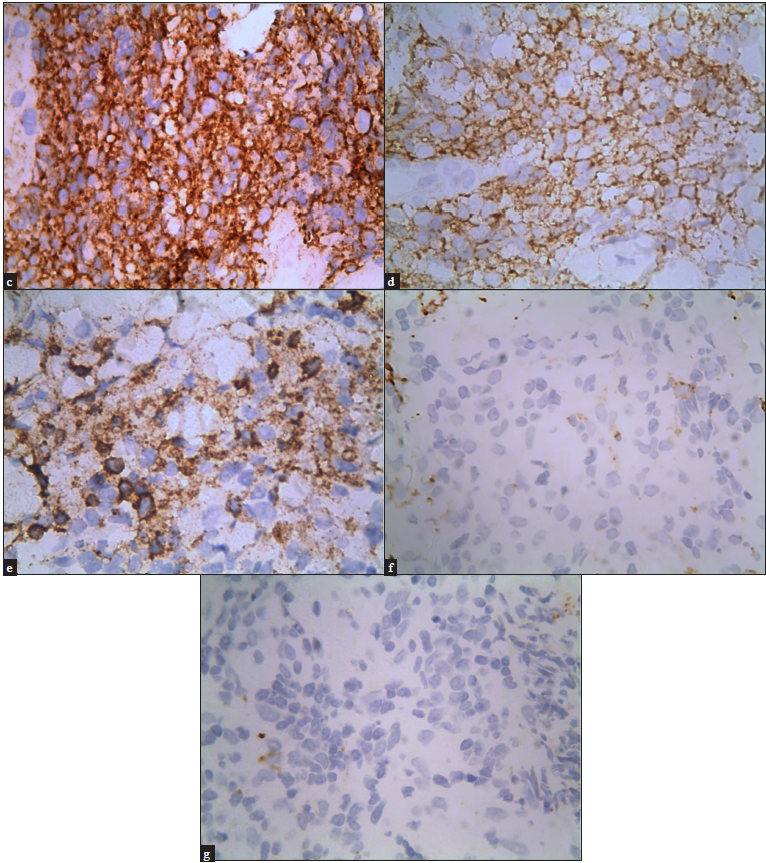
- Immunohistochemical staining demonstrated that the tumour cells were diffusely positive for (c) CD38, 400x, (d) CD123, 400x, (e) CD56, 400x, and negative for (f) CD34, 400x, and (g) anti-myeloperoxidase, 400x.
BPDCN is a rare haematologic malignancy that is derived from plasmacytoid dendritic cells (pDC) that overexpress interleukin-3 receptor subunit alpha.2 The markers related to plasmacytoid dendritic cell origin (HLA-DRhigh, CD123, CD303, CD304, and cTCL1), and CD4 and CD56 are positive in BPDCN. Moreover, the elevated expression of some lineage markers (CD33, CD7, and CD22) with HLA-DRhigh, CD4 and CD56 positivity without specific markers from the myeloid, B-lymphoid, and T-lymphoid lineages (CD19, cCD3, MPO, CD14, and CD64) cannot exclude this diagnosis.3 Intensive chemotherapy regimens for acute myeloid or lymphoblastic leukaemia can be used for the treatment of BPDCN. Allogeneic stem cell transplantation in patients fit for it should be considered to potentially improve overall survival. In recent years, targeted therapy (tagraxofusp, Bcl-2 inhibitor) has become a new treatment option.2 However, regardless of the treatment method, BPDCN has a poor prognosis, especially when present with leukemic presentation, in which the median overall survival is 8.7 months.4
Skin lesions were the initial manifestations. Skin lesions of BPDCN often appear as asymptomatic bruise-like lesions, papules, plaques, or nodules. BPDCN clinically mimicking dermatomyositis, lymphoma/leukaemia cutis, and cutaneous lupus erythematosus has also been reported.5-7 The present patient had a recurrent nodular erythematous pattern, which reminds us that BPDCN should be considered in the differential diagnosis of refractory skin lesions. The bone marrow biopsy findings were consistent with acute myeloid leukaemia. To avoid delayed treatment, early skin biopsy and immunochemistry should be emphasised in the differential diagnosis of BPDCN and acute myeloid leukaemia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The 5th edition of the World Health Organization classification of haematolymphoid tumours: Myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36:1703-19.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Blastic plasmacytoid dendritic cell neoplasm: Diagnosis, manifestations, and treatment. Curr Opin Hematol. 2020;27:103-7.
- [CrossRef] [PubMed] [Google Scholar]
- How should we diagnose and treat blastic plasmacytoid dendritic cell neoplasm patients? Blood Adv. 2019;3:4238-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: An Italian multicenter study. Haematologica. 2013;98:239-46.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Blastic plasmacytoid dendritic cell neoplasm mimicking dermatomyositis. JAAD Case Rep. 2023;39:70-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A rare case of blastic plasmacytoid dendritic cell neoplasm in a child mimicking lymphoma/leukemia cutis. Dermatopathology (Basel). 2022;9:321-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case of blastic plasmacytoid dendritic cell neoplasm initially mimicking cutaneous lupus erythematosus. Cancer Res Treat. 2010;42:239-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






