Translate this page into:
Blastomycosis-like pyoderma: Novel use of potassium iodide
2 Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India
Correspondence Address:
Dincy C. V. Peter
Department of Dermatology, Venereology and Leprosy, Christian Medical College, Vellore, Tamil Nadu
India
| How to cite this article: Borra SK, Peter DC, Balakrishnan N, Pulimood S, Bhindra M. Blastomycosis-like pyoderma: Novel use of potassium iodide. Indian J Dermatol Venereol Leprol 2017;83:720-721 |
Sir,
Blastomycosis-like pyoderma, an unusual form of pyoderma presenting with large verrucous plaques studded with multiple pustules and draining sinuses, is seen in immunocompromised patients with chronic myeloid leukemia, underlying neoplasm, diabetes mellitus, and alcoholism.[1] The treatment of blastomycosis-like pyoderma can be challenging. We report a case of blastomycosis-like pyoderma which responded favourably to saturated solution of potassium iodide.
A 57-year-old lady presented with asymptomatic lesions over her left leg for last 1 year. Initially a painless papule developed over her shin, which gradually enlarged to form a plaque with central ulceration and peripheral extension to attain the present form. There was no history of trauma. Her general and systemic examinations were unremarkable. Cutaneous examination revealed a well-defined large plaque, sized 18 × 13 cm with central scarring, peripheral hyperkeratotic crust, and ulceration over the left shin and a similar smaller plaque over the left ankle [Figure 1a] and [Figure 1b]. Left inguinal lymphadenopathy was noted.
 |
| Figure 1a: Well-defined large plaque with central scarring and peripheral hyperkeratotic crust and ulceration over the left shin |
 |
| Figure 1b: Well-defined plaque with central scarring and peripheral hyperkeratotic crust over the left ankle |
The clinical differential diagnoses included lupus vulgaris, atypical mycobacterial infection, chromoblastomycosis, and cutaneous nocardiosis. Her investigations were within normal limits except for an elevated c-reactive protein and blood sugars (postprandial sugar – 218 mg/dl). Mantoux test was negative. Histopathology showed pseudoepitheliomatous hyperplasia and upper dermal abscesses with predominantly neutrophilic infiltrate [Figure 2a] and [Figure 2b]. There were no granulomas and special stains were negative for fungal elements. Tissue bacterial cultures grew Enterococci, Proteus mirabilis, and Escherichia coli repeatedly at different occasions. The tissue fungal and mycobacterial cultures were negative.
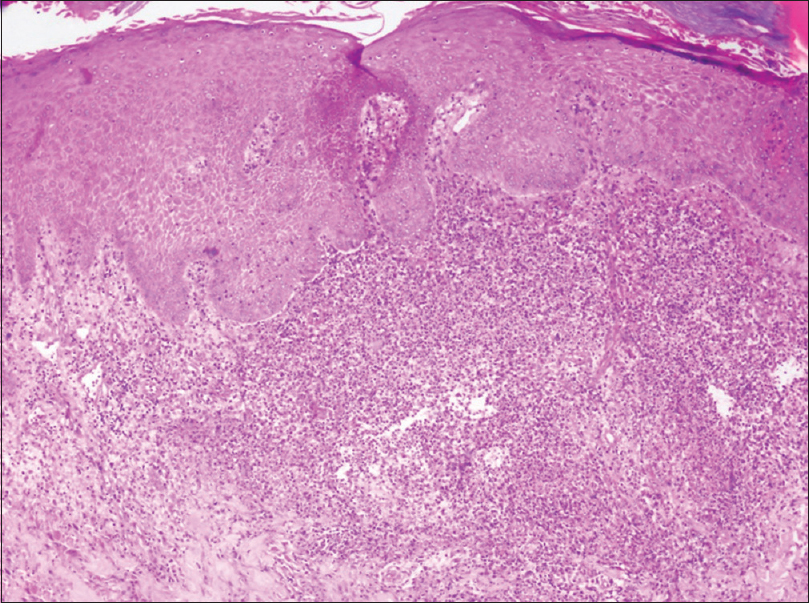 |
| Figure 2a: Skin biopsy showing pseudoepitheliomatous hyperplasia with multiple upper dermal abscesses. H and E, ×100 |
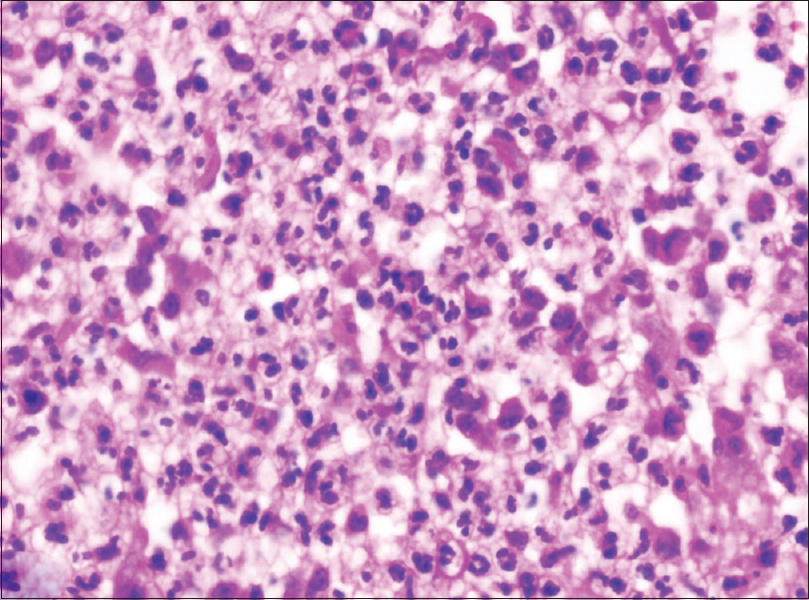 |
| Figure 2b: Skin biopsy showing predominant neutrophilic dermal infiltrate. H and E, ×400 |
A diagnosis of blastomycosis-like pyoderma was made as our patient met 4 of 6 criteria proposed by Su, Duncan and Perry: (1) Isolation of a pathogenic microbe; (2) clinical presentation of large verrucous plaques with multiple pustules and elevated borders; (3) microscopic findings of pseudooepitheliomatous hyperplasia with neutrophil-rich microabscesses within the epidermis and dermis; (4) negative culture for deep fungi, atypical mycobacteria, and mycobacterium tuberculosis; (5) negative fungal serology test result; and (6) bromide level in the blood within reference range.[2] The first four criteria were present in our patient.
The patient was initiated on tablet metformin 500 mg twice a day for diabetes, following which her glycemic control improved. Specific therapy included several courses of systemic antibiotics including piperacillin-tazobactam, linezolid, amikacin, and meropenem based on antibiograms for a period of 2 months and was later continued on doxycycline. Acitretin was given for 4 months along with adjuvant therapies such as cryotherapy, curettage, intralesional steroids, and ablative carbon dioxide laser. The modalities were used along with acitretin one at a time and discontinued before the next modality of treatment as the patient did not show significant improvement in skin lesions. She developed new lesions even while on acitretin and antibiotics. Acitretin was stopped due to financial constraints and was continued on co-trimoxazole and doxycyline. As there was no significant clinical improvement, saturated solution of potassium iodide was added in a dose of three drops thrice daily with a gradual increase to 12 drops thrice daily. Resolution of vegetating granulation tissue was observed within 1 month and complete remission in 3 months [Figure - 3]. Thereafter, saturated solution of potassium iodide was tapered and stopped over the next 3 months.
 |
| Figure 3: Resolution of lesions after 3 months of saturated solution of potassium iodide |
Blastomycosis-like pyoderma is an unusual vegetative proliferating tissue response to an infection. Common organisms isolated from tissue cultures of patients with blastomycosis-like pyoderma include Staphylococcus aureus, Beta-hemolytic streptococci, Pseudomonas aeruginosa, Proteus mirabilis, E. coli, and Candida albicans and anaerobes including Prevotella and Corynebacterium. As the condition is unresponsive to antibiotics alone, the role of these bacteria in the pathogenesis of the condition is unclear.[1]
Blastomycosis-like pyoderma is usually managed with systemic antibiotics. Recent reports have demonstrated the use of acitretin with good response.[3] Other treatment options include topical and intralesional steroid, saturated solution of potassium iodide, dapsone, cyclosporine, cryosurgery, electrodessication and CO2 laser ablation.[4] Our patient showed remarkable response with saturated solution of potassium iodide, despite the failure of all other therapeutic modalities. There was complete resolution within 3 months and she is in complete remission for more than 6 months. Saturated solution of potassium iodide acts by decreasing the inflammatory reaction, suppressing the neutrophil chemotaxis, and release of their toxic intermediates.[5]
We postulate that saturated solution of potassium iodide is a good therapeutic option in patients with blastomycosis-like pyoderma based on our patient's response. As it is cheap, easily available, and with minimal side effects, we propose saturated solution of potassium iodide as the first line agent along with an appropriate antibiotics to treat blastomycosis-like pyoderma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Burns T, Breathnach S, Cox N, Griffiths C, editors. Bacterial infections. In: Rook's Textbook of Dermatology. 8th ed. Edinburgh: Blackwell Publishing Ltd.; 2010; Vol 2. p. 30.77-30.78.
[Google Scholar]
|
| 2. |
Su WP, Duncan SC, Perry HO. Blastomycosis-like pyoderma. Arch Dermatol 1979;115:170-3.
[Google Scholar]
|
| 3. |
Lee YS, Jung SW, Sim HS, Seo JK, Lee SK. Blastomycosis-like pyoderma with good response to acitretin. Ann Dermatol 2011;23:365-8.
[Google Scholar]
|
| 4. |
Su O, Demirkesen C, Onsun N. Localized blastomycosis-like pyoderma with good response to cotrimoxazol and cryotherapy. Int J Dermatol 2004;43:388-90.
[Google Scholar]
|
| 5. |
Schulz EJ, Whiting DA. Treatment of erythema nodosum and nodular vasculitis with potassium iodide. Br J Dermatol 1976;94:75-8.
[Google Scholar]
|
Fulltext Views
3,695
PDF downloads
2,113





