Translate this page into:
Blue palms and nails: A clue to diagnosis of alkaptonuria
2 Department of Radiodiagnosis, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India
Correspondence Address:
Arpita Nibedita Rout
Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar - 751 019, Odisha
India
| How to cite this article: Sirka CS, Rout AN, Naik S, Sahu K. Blue palms and nails: A clue to diagnosis of alkaptonuria. Indian J Dermatol Venereol Leprol 2020;86:753 |
Sir,
Alkaptonuria is a rare autosomal recessive disorder of the tyrosine metabolism pathway caused by deficiency in the enzyme homogentisate-1, 2-dioxygenase.[1] Homogentisic acid is oxidized to benzoquinone acetate, which polymerizes to form a melanin-like dark yellow pigment or “ochre”, which is deposited in the cartilage and other connective tissue and causes ochronosis.[2] Skin and nail pigmentation occurs rarely.
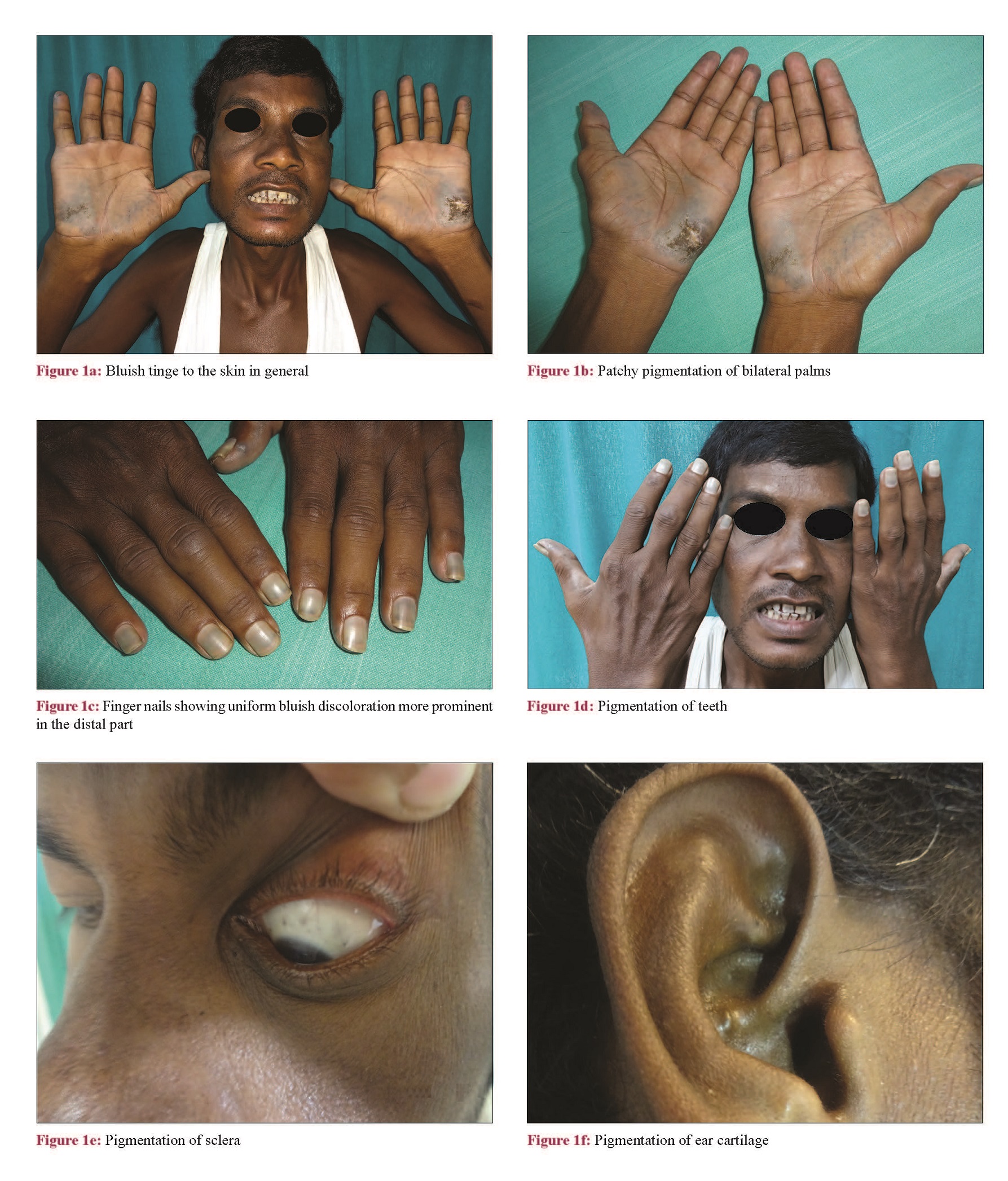
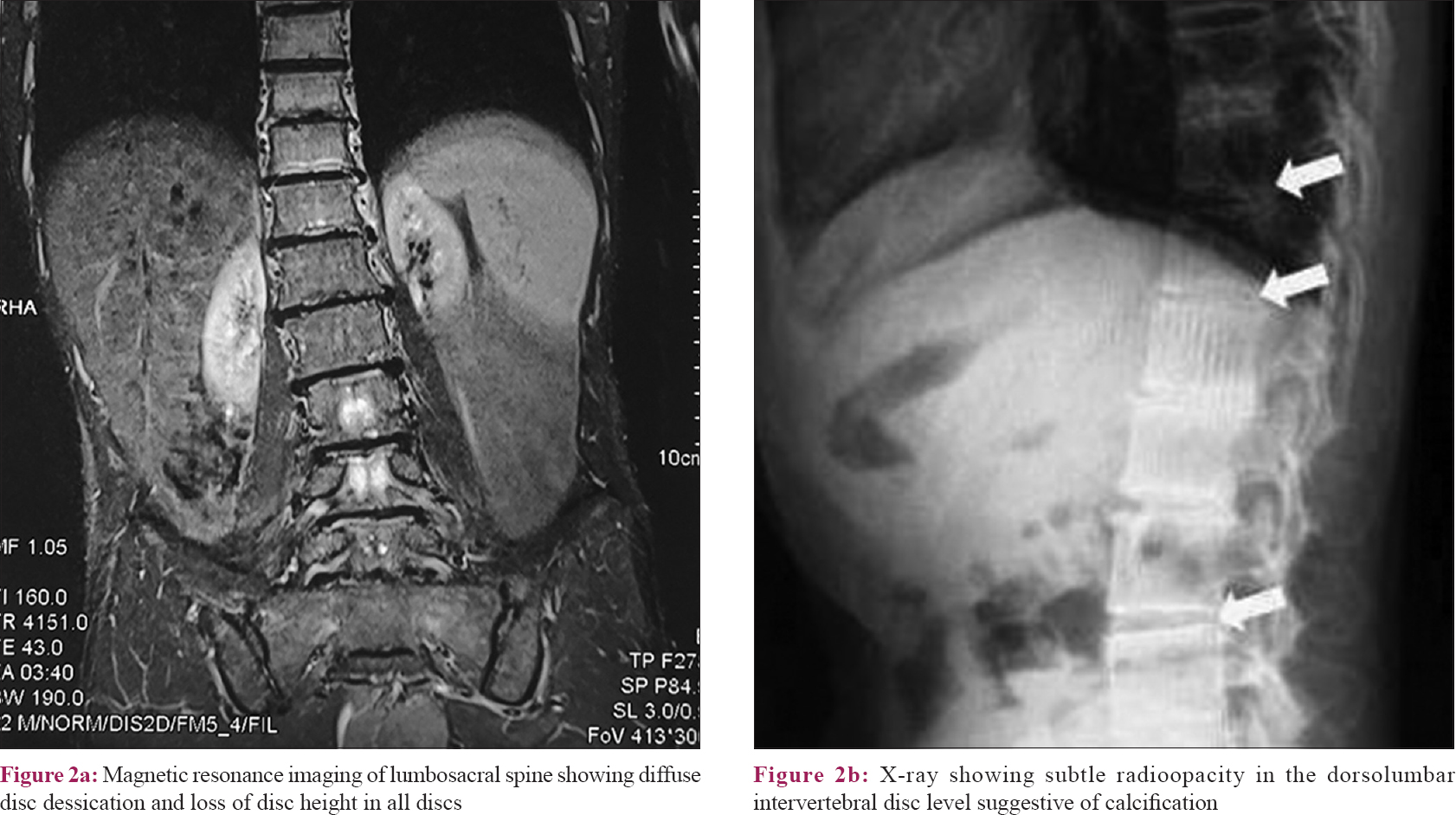
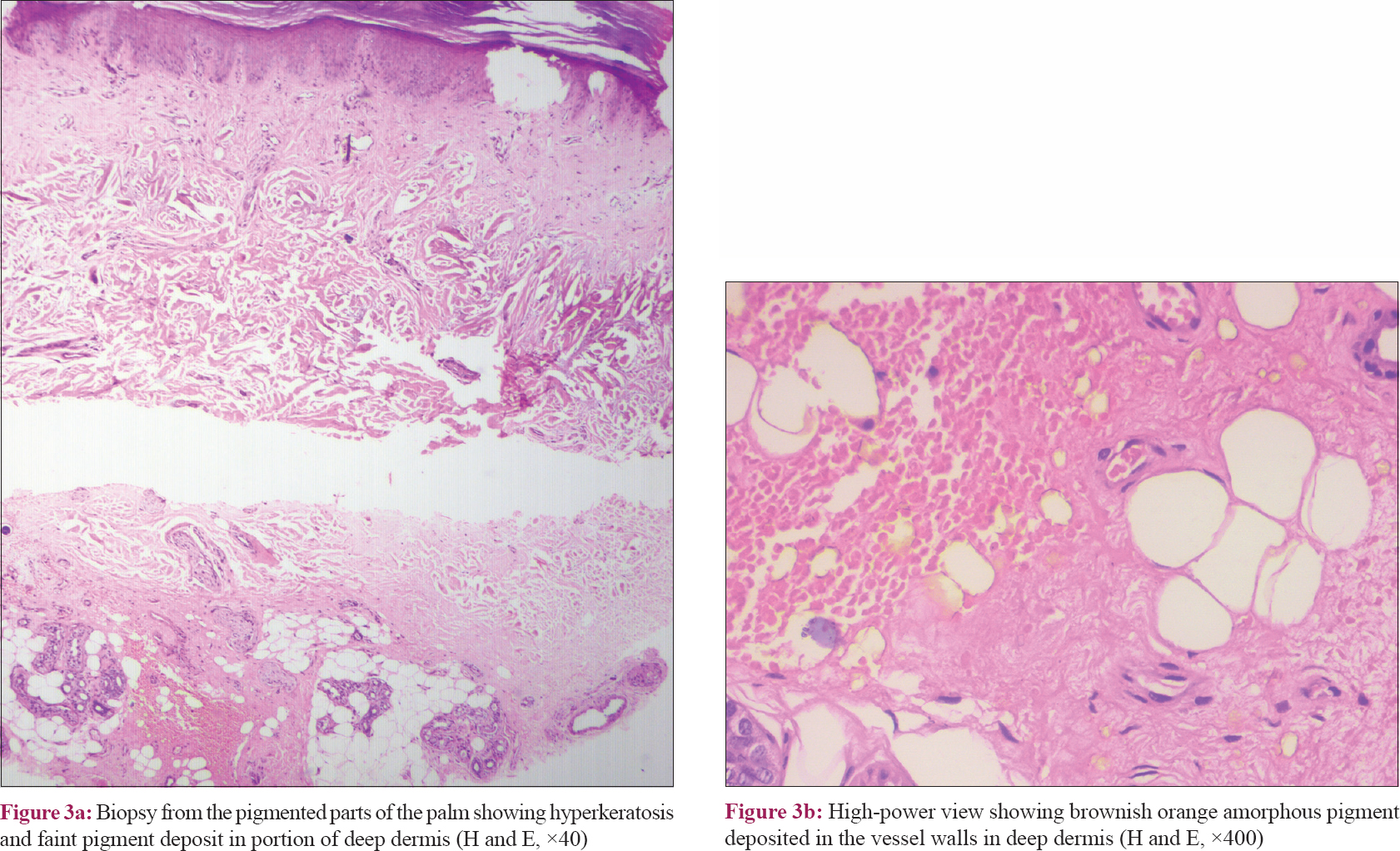
A 42-year-old male presented with 3 years- history of bluish discoloration of nails, teeth, palm soles, and sclera. He had history of low back pain since the past 10 years, for which he had taken various indigenous and ayurvedic drugs for a prolonged period. There was history of periorbital swelling intermittently. There was neither any similar history in the family or neighbors, nor any history of exposure to any heavy metal in the workplace. On examination, there was a bluish tinge to the skin in general [Figure - 1]a. There was patchy pigmentation of bilateral palms with more severe involvement of thenar eminence and the sides of fingers, with the central parts of the pigmented areas showing thickening, fissuring, and atrophy [Figure - 1]b. There was stiffness of fingers with difficulty in making a fist. All the finger nails showed uniform bluish discoloration, more prominent in the distal part with a thin strip of uninvolved area in the distal-most aspect [Figure - 1]c. There was pigmentation of teeth, sclera, and ear cartilage [Figure - 1]d, [Figure - 1]e, [Figure - 1]f. There were no features of central nervous system or gonadal involvement clinically. Based on the history and clinical findings, alkaptonuria and heavy metal toxicity were considered in the differentials. On cross-questioning, the patient gave history of noticing blackish discoloration of urine since the past 2 months. On collecting and keeping the urine in a container, it turned black. On dermoscopy, the pigmented areas showed globular structures and the nails showed bluish longitudinal streaks, suggestive of deposition of the pigment in vessel walls. There was microcytic hypochromic anemia with the hemoglobin level being 10.2 g/dL. Serum urea (93 U/dL) and creatinine (4.3 U/dL) levels were raised. Liver function test and blood sugar levels were normal. Ultrasonography of the abdomen and pelvis showed bilateral small kidneys, increased cortical echogenicity, and reduced corticomedullary differentiation suggesting chronic kidney disease. X-ray of the spine showed subtle radioopacity in the dorsolumbar intervertebral disc suggestive of calcification [Figure - 2]a. Magnetic resonance imaging of the lumbosacral spine showed diffuse disc dessication and loss of disc height in all discs with multiple anterior and posterior marginal osteophytes [Figure - 2]b. Biopsy from the pigmented parts of the palm showed brownish orange amorphous pigment deposited in the vessel walls in deep dermis [Figure - 3]a and [Figure - 3]b. Urine homogentisic acid levels could not be assessed due to nonavailability of the test. On alkalinization with 10% ammonia, the urine turned black [Figure - 4]. Thus, based on the clinical and laboratory findings, the final diagnosis of alkaptonuria was made and the patient was advised oral ascorbic acid, low-protein diet, and sodium bicarbonate 250 mg, nifedipine 5 mg, and analgesics (sos) for renal and joint symptoms. On follow-up after 2 months, there was improvement in the joint pain (not requiring analgesics) and decreased stiffness of the pigmented areas of palms.
 |
 |
 |
 |
| Figure 4: On alkalinization of urine with 10% ammonia, the urine turned black |
Darkening of the urine upon standing is one of the first symptoms of alkaptonuria, often noticed from the staining of the diaper. In developing countries like India, this may be missed because of the lack of practice of using diaper. Pigmentation of sclera (Osler's sign), ear cartilage, antihelix, tragus (ochronosis), mucosae, tendons, nail bed, crown of the teeth, skin, thenar and hypothenar eminences, and sides of fingers along with pits sparing the center of the palm is seen around fourth decade.[3],[4] Other findings include ochronotic arthropathy involving weight-bearing joints (spine and knees) and narrowing of joint spaces and calcifications.
Heavy metal poisoning can be ruled out by history of exposure and systemic complications. Exogenous ochronosis, following systemic antimalarials, can be excluded by lack of systemic effects and negative urine alkalinization test.[5],[6]
Classically, histopathology shows stout, sharply defined, crescentic, vermiform, or banana-shaped ocher-colored fibers; however, small pigmented deposits in the dermis, in macrophages, in the endothelial cells of blood vessels, and the basement membrane of sweat glands have also been described.[7] Our case had patchy deposits of orange-brown pigments around blood vessels and in the deep dermis.
Supportive medical management is the mainstay of treatment. It includes a low-protein diet, analgesia, nitisinone, spinal surgery, arthroplasty, and alkalinization of urine.[8],[9],[10]
Our patient had presented to many general physicians and nephrologists before, however their failure to correlate history of joint pain and facial swelling to the discoloration of nails and skin had delayed the diagnosis. In darker skin types, the subtle change in skin, sclera, and cartilages may go unnoticed for long. Pigmentation of the skin over palms and soles and nails in the presence of arthropathy and nephropathy should raise a suspicion of alkaptonuria and simple alkalinization of the urine can lead to a diagnosis in resource-poor settings. In our patient, alkalinization of urine with sodium bicarbonate resulted in symptomatic improvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Zatkova A. An update on molecular genetics of alkaptonuria (AKU). J Inherit Metab Dis 2011;34:1127-36.
[Google Scholar]
|
| 2. |
Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21.
[Google Scholar]
|
| 3. |
Dogra A, Bajwa GS, Bajwa N, Khurana S. Alkaptonuria. Indian J Dermatol Venereol Leprol 2001;67:271-2.
[Google Scholar]
|
| 4. |
Khatu SS, More YE, Vankawala D, Chavan D, Gokhale NR. Alkaptonuria: Case report. Med J DY Patil Univ 2015;8:84-6.
[Google Scholar]
|
| 5. |
Bhattar PA, Zawar VP, Godse KV, Patil SP, Nadkarni NJ, Gautam MM. Exogenous ochronosis. Indian J Dermatol 2015;60:537-43.
[Google Scholar]
|
| 6. |
Koska L, Srsen S. A simple urine screening test for alcaptonuria. N Engl J Med 1977;297:1471-2.
[Google Scholar]
|
| 7. |
Ranganath LR, Milan AM, Hughes AT, Dutton JJ, Fitzgerald R, Briggs MC, et al. Suitability of nitisinone in alkaptonuria 1 (SONIA 1): An international, multicentre, randomised, open-label, no-treatment controlled, parallel-group, dose-response study to investigate the effect of once daily nitisinone on 24-h urinary homogentisic acid excretion in patients with alkaptonuria after 4 weeks of treatment. Ann Rheum Dis 2016;75:362-7.
[Google Scholar]
|
| 8. |
Weedon D. Cutaneous deposits. In: Patterson JW, editors. Weedon's Skin Pathology. 4th ed. London: Churchill Livingstone Elsevier; 2016. p. 445-6.
[Google Scholar]
|
| 9. |
Davison AS, Norman BP, Smith EA, Devine J, Usher J, Hughes AT, et al. Serum amino acid profiling in patients with alkaptonuria before and after treatment with nitisinone. JIMD Rep 2018;41:109-17.
[Google Scholar]
|
| 10. |
Williams DP, Lawrence A, Meng X. Pharmacological and toxicological considerations of homogentisic acid in alkaptonuria. Pharmacologia 2012;3:61-74.
[Google Scholar]
|
Fulltext Views
5,152
PDF downloads
1,978





